Translate this page into:
Recommendations for Cutaneous and Aesthetic Surgeries during COVID-19 Pandemic
Address for correspondence: A. Somaiah Savitha, Department of Dermatology, Sapthagiri Institute of Medical Sciences & Research Centre, Bengaluru, Karnataka, 560090, India. E-mail: drsavithasomaiah@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Amid the coronavirus disease 2019 (COVID-19) pandemic, dermatologists must be prepared to restructure their practice of procedural dermatology and cutaneous aesthetic surgeries. The COVID-19 pandemic has presented several challenges and has ushered in several changes in practice such as teledermatology, with many physicians adopting virtual consultations and treatments. Performing procedures in the times of COVID-19 pandemic presents challenges such as risk of transmission to doctors and staff due to potential aerosolization, release of virus droplets during the procedures, and risk of virus transfer through the instruments both in the peri- and postoperative period. This can have several medical, administrative, and legal implications.
Objectives:
This document aimed to outline best practices that can be followed in this scenario to perform cutaneous surgeries and procedures to ensure safer skin surgery.
Recommendations:
Standard precautions include social distancing of at least 1 m, hand hygiene, appropriate use of personal protective equipment (PPE), safe injection practices, sterilization and disinfection of medical devices, environmental cleaning, and respiratory hygiene. It is generally advisable to see patients only by appointments. Each clinic should have a special area at entry for screening patients and providing sanitizers and masks. Procedures, which are of short duration, performed on nonfacial areas are considered as low risk and require donning surgical mask. Procedures involved with minimal invasiveness and bleeding, short duration procedures on the face such as injectables, chemical peels, and aerosol-generating procedures on nonfacial areas are considered moderate risk. These procedures need apron with head cover, N95 mask, face shield, double gloves, and smoke evacuator with high-efficiency particulate air (HEPA) or ultralow particulate air (ULPA) filter. Aerosol and plume-regenerating procedures (such as ablative lasers on the face), prolonged surgeries on head (such as hair transplantation), intraoral, and intranasal procedures are considered high risk. These procedures must be carried out with full body cover with surgical gown, head cover, N95 mask, face shield, double gloves, and smoke evacuator. Physicians should be aware of local epidemiological situation and adhere to the relevant guidelines issued by the relevant governmental agencies.
Keywords
Aesthetic dermatology
coronavirus disease 2019
dermatosurgery
INTRODUCTION AND BACKGROUND
The coronavirus disease 2019 (COVID-19) pandemic has caused global havoc affecting the physical, mental, and financial health of the human race. The severe acute respiratory syndrome corona virus 2 (SARS-CoV2) poses novel challenges for all medical and surgical specialties, including dermatology, cutaneous, and aesthetic surgery. Dermatologists and dermatologic surgeons must, therefore, be prepared to restructure their practice and adapt to embrace the changes that are likely to stay for a long time.
Dermatology is unique in being a very visual specialty where many skin conditions can be diagnosed on visualizing skin lesions with some exceptions. The COVID-19 pandemic has ushered in an era of teledermatology, with many physicians adopting virtual consultations and treatments. Though consultations, to a varying extent, can be done using telemedicine, procedures cannot be performed virtually. Procedural dermatology and cutaneous aesthetic surgery is a significant component of practice, with 30%–60% revenue being generated from it. Inability to perform these procedures can lead to incomplete patient care, disruption in continuity of treatment (many procedures require multiple sessions), revenue loss, and possible financial issues for staff payments, servicing loans, and so on. The situation varies greatly in different parts of the country and so do governmental regulations. The regulations were strict in the early period of the pandemic, with restriction on all nonessential elective procedures. Now there has been a gradual relaxation of these restrictions with routine procedures being allowed to be performed in all but containment areas. But even when regulations permit routine work, the risk of transmission of virus to the doctor, staff and other patients continue to exist. Hence dermatosurgical practice continues to be under stress and we need to devise strategies to adapt to these challenges.
The challenges in this scenario are as follows:
How and when do we take up procedures—Dermatosurgical, aesthetic, and laser?
What are the risks involved to the dermatologists, their staff, and patients?
What safety measures do we follow and precautions do we take?
How to sterilize our equipment?
The only time we can be absolutely certain of safety is with the development of an effective and easily available vaccine or the population develops herd immunity. But such a time is definitely at least months, if not years away. There is a need to be prepared to perform these procedures in a safe manner till that time, both for patients and staff. This situation has been faced earlier with hepatitis B and human immunodeficiency virus (HIV) infections. Although there was much confusion early on, once reliable testing and definite knowledge of methods of transmission were established, the doctors adopted safe practices to prevent transmission before and while doing surgery.
Performing any surgical procedures in the times of COVID-19 pandemic presents huge challenges. Risk of transmission is very high due to following factors:
There are multiple modes of transmission—droplet, aerosol, fomites, and possibly others such as fecal transmission. Skin to skin transmission has not been documented so far[1]
Risk is higher in healthcare professional than the average population due to higher viral load and repeated exposures
Severe illness is likely in elderly[2]
Risk is posed to family members and community of the healthcare professional
In the event of the patient turning positive for COVID-19, the clinic can be sealed off, staff can face isolation. There is also the possibility of the clinic getting the stigma of corona. It can also be argued that essential equipment such as personal protective equipment (PPE) may be misused for such procedures, which can safely be postponed. In view of these factors, it has been thought prudent to postpone the procedures during the lockdown period.[3] Box 1 enumerates the special features of dermatosurgical procedure.
Box 1: Special features of dermatosurgical procedures
Most dermatosurgical procedures are day care procedures and often less invasive
Often, they need multiple sessions and hence repeated visits to the clinic
Only few are considered essential (e.g., biopsy, skin cancer, treatment of infectious conditions such as viral warts, molluscum contagiosum, and abscess)
Many are considered as cosmetic treatments
Some are associated with plumes and aerosol (e.g., electrocautery, ablative radiofrequency [RF], ablative laser, dermabrasion, and follicular unit extraction [FUE] hair transplantation)
Many of them are on the face and hence exposure to nose and throat is likely
Many of them need prolonged period, even hours (e.g., vitiligo surgery, hair transplantation, liposuction, and autologous fat graft)
Some surgeries need multiple assistants (e.g., hair transplantation)
It is also important to understand that although dermatosurgical procedures may be minor, emergencies can occur during any procedure, which may need interventions such as resuscitation and intubation. These need to be considered seriously while choosing to perform such procedures.
Objectives of this document and disclaimer
This document aimed to outline best practices that can be followed in the scenario of COVID-19 pandemic to perform procedures. It is important to note that these recommendations are being drafted in the light of limited Indian experience and based on the experience in other countries, and hence need to be considered provisional and could change in future. These will serve only as a guide and do not include every possible measure needed. The treating dermatosurgeon will have to consider each case on its merit and take precautions and adopt procedures as needed. These recommendations will not limit the dermatosurgeon from taking any additional precautions for the patient as he/she deems necessary or as advised by the local health authorities. In summary, these recommendations are minimum recommendations, in the light of current evidence available or based on expert opinion, but subject to change and modifications. Also, these guidelines are subject to guidelines and instructions issued by appropriate governmental agencies in that particular geographical COVID zones, and where these guidelines are in conflict, the governmental guidelines will take precedence. Neither the authors nor Association of Cutaneous Surgeons (India) (ACS(I)) nor Journal of Cutaneous and Aesthetic Surgery (JCAS) will be liable for any medicolegal issues that may arise out of adopting these recommendations.
Mode of virus transmission
SARS-CoV2 is transmitted through respiratory droplets (size, >5–10 microns) and physical contact routes.[45] A person in close contact (<1 m) with a patient having symptoms such as sneezing and/or coughing is at risk, with the possibility of his/her oronasal mucosae and conjunctivae getting exposed to potentially infective droplets. Fomites and the immediate environment of the infected person can also transmit the infection.[6] Airborne transmission is not proven yet. According to a recent publication in the New England Journal of Medicine (NEJM), experimentally generated aerosol in the COVID-19 patient’s vicinity showed persistence of virus for 3h.[7] Being an experimentally generated aerosol, this finding does not reflect the clinical setting, in which aerosol generating procedures are performed. Transmission via skin has not been documented.
Risk of viral transmission in dermatology clinics
The virus is not dermatotropic and transmission via skin has not been documented. However, viral transmission can occur during performance of dermatosurgical procedure by the above routes. Hence dermatology clinics and outpatient departments should develop appropriate preventive measures.[8] The fomites, which may transmit the virus in the clinic or hospital, are enumerated in Box 2. Table 1 shows the persistence of the virus on different surfaces.[9]
| Type of surface | Virus | Temperature | Persistence |
|---|---|---|---|
| Steel | HCoV | 21°C | 5 days |
| Aluminum | HCoV | 21°C | 2–8 h |
| Metal | SARS-CoV | RT | 5 days |
| Wood | SARS-CoV | RT | 4 days |
| Paper | SARS-CoV Strain P9 | RT | 4–5 days |
| SARS-CoV Strain GVU6109 | RT | 24h (106 inoculum) | |
| 3h (105 inoculum) | |||
| <5 min (104 inoculum) | |||
| Glass | SARS-CoV | RT | 4 days |
| HCoV | 21°C | 5 days | |
| Plastic | SARS-CoV Strain HKU39849 | 22°–25°C | ≤5 days |
| SARS-CoV Strain P9 | RT | 4 days | |
| SARS-CoV Strain FFM1 | RT | 6–9 days | |
| HCoV Strain 229E | RT | 2–6 days | |
| PVC | HCoV | 21°C | 5 days |
| Silicon rubber | HCoV | 21°C | 5 days |
| Surgical glove (latex) | HCoV | 21°C | ≤ 8 h |
| Disposable gown | SARS-CoV | RT | 2 days (106 inoculum) |
| 24h (105 inoculum) | |||
| 1h (104 inoculum) | |||
| Ceramic | HCoV | 21°C | 5 days |
| Teflon | HCoV | 21°C | 5 days |
HCoV = human coronavirus, SARS = severe acute respiratory syndrome, RT = room temperature
Box 2: Fomites, which may transmit the virus in the clinic or hospital
Reception desk, landline, and mobile phones at the reception
Currency, card swipe machine
Armrests of chairs–sofa, magazines, newspapers, brochures
Old prescriptions or files that patients carry
Examination bed, bedcover, and so on
Patient chair in waiting areas and consultation rooms
Magnifying glass, dermatoscope, headlights
Laptop, desktop
Remote controls
Devices and their keys
Elevator panel, staircase handle bars, door knobs
Electrical switch board
Employee biometric machines
Doors and the mesh of ultraviolet (UV) chambers
And many such things, where there is a possibility of patient touching with hands
Office procedures in the clinic, minor, and major operating theaters (OT) pose additional risks, both for the healthcare worker (HCW) and the patient undergoing the procedure. This risk is due to potential aerosolization, release of virus droplets during the procedures, and risk of virus transfer through the instruments both in the peri- and postoperative period. Aerosols with diameter of 5 microns can remain suspended for long period, especially in closed environments and in high viral concentrations, and can gain entry into respiratory tract.
Most dermatosurgical procedures are minor and done in day care theater. Some procedures need magnification such as hair transplantation, which poses additional challenge, necessitating modifications in the face shield for the surgeon. These can be performed with proper PPE and risk stratification, to be explained later.
Major surgeries needing general anesthesia and intubation are rarely performed in dermatosurgical practice. However, if they are planned, these should be performed in a major theater, as dermatosurgical theater is not equipped in the same way as a standard theater in a tertiary care hospital. High-efficiency particulate air (HEPA) respirators/filters are at least 99.97% efficient in removing particles ≥0.3 μm in diameter.[10] Social distancing is difficult to adopt and using shields or even masks may not be feasible when major surgeries are to be done on the face.
RECOMMENDATIONS FOR MINIMIZING RISK OF INFECTION
Recommendations to prevent transmission of healthcare-associated infections include standard precautions and transmission-based precautions.[11]
Standard precautions are a set of practices applied to the care of patients, regardless of the state of infection, whether suspected or confirmed. These include hand hygiene, appropriate use of PPE, safe injection practices, sterilization and disinfection of medical devices, environmental cleaning, and respiratory hygiene. Transmission-based precautions include extra precautions to prevent transmission by contact, droplet, and airborne routes.[11]
All personnel including dermatosurgeons, nurses, receptionists, patients, and attendants need to adopt protective measures. As viral spread occurs very easily from person-to-person contact and droplet transmission, triage of patients is of pivotal importance to detect patients with suspected COVID-19 infection at the first point of contact with the healthcare system.
Social (physical) distancing
Social distancing means keeping space between yourself and other people outside of your home.[1213] The authors feel this is better termed as physical distancing in the context of procedures. Physical (social) distancing helps limit contact with infected people and contaminated surfaces. New study, published in the journal Science, documents that for every confirmed case of COVID-19 there are likely another five to 10 people with undetected infections.[14]
To practice social or physical distancing stay at least 1 m (3 feet) from other people.[15]
Physical (social) distancing practice at different places of clinic is mentioned as following:
Appointments
It is generally advisable to see patients only by appointments, and walk-ins are avoided, except in cases of urgent situations. Reduce the frequency of visits for the chronic patients, the elderly patients, small children, or patients with comorbidities, and offer them teledermatology. Restrict other attendants and visitors accompanying the patients. Every effort should be made to screen patients while giving appointments. History of COVID 19 symptoms, travel to COVID 19 containment areas and contact with COVID 19 patients should be asked for. Such patients are to be advised by teleconsultation. Patients are advised to compulsorily wear a mask when attending the clinic.
On arrival to clinic
It is advised to create a special area at the entrance to screen patients, check temperature with infrared thermometer, and also to control entry. It is also advisable that this person who mans at the entry wear PPE. Hand sanitizers need to be given to patients at the entry. Patients who turn up without masks may be provided mask at the entry.
At reception area
In the reception area, a closed cubicle with window is preferred. If it is open area with a table, the table should be of minimum 3 feet width separating the patient from the receptionist. Additional physical separation and protection can be created by having a vertical transparent partition put along the outer edge of the table. Further separation can be enforced by putting a chain or a mechanical obstacle between patient and the front office desk.
Patient waiting area
A minimum number of appointments need to be given to avoid crowding. If feasible, patients can even be seen in the car, with window raised. If you have individual chairs in the waiting area, a minimum distance of 3 feet between the chairs has to be maintained. It has to be maintained on all sides of the chairs. All chairs with soft, porous surfaces such as cloth, leather, and leatherette must be replaced with metal or plastic chairs, as it is difficult to disinfect soft and porous surfaces. If the existing facility has benches, then depending on the length, patient seating area has to be marked with red adhesive tapes. Even while seating the patients, odd and even number chairs should be assigned to the patient batchwise. Because after every batch of patients, there is a need to disinfect the chairs occupied earlier. Patients’ attendants are not allowed, except in cases of small children and the elderly. Patients and their attendants can wait in car or a separate area, coming into the reception only when there is adequate space.
Inside examination cubicle
If the executive table of the physician is of sufficient width to practice social distancing by 1 m then that would be adequate. Otherwise it is advisable to place the patient’s and attender’s chair at sufficient distance of at least 1 m. Most of the time, patients can be examined in sitting or standing position, hence avoiding examination couch is ideal. In case needed, the examination couch with paper roll holder is better. Noncontact dermoscopy is better if need arises. The surface of the dermoscope has to be cleaned with alcohol swab after each patient, or a cling film can be used to cover the plate.
Handling of files
Avoiding handling of files is advised. Your clinical note can be in the computer data sheet for future references. If that facility is not available, then case paper may be given in a single-page plastic folder, and the receptionist be instructed to clean the outer surface with alcohol-based sanitizers and sent directly to the physician chamber.
Prescription
E-prescription is preferred, but if such facility is not available, small prescription paper may be written and given in a plastic transparent pouch, which can be read by the pharmacist also to supply the necessary medicine. A fresh prescription should be used for each visit.
Recommendations for payment
Ideal option is digital payment. Otherwise a cashbox to drop the necessary fees can be kept. Patient should be told to provide the exact amount needed. The receptionist is required to keep necessary paper currency and coins to transact instead of picking from the cash box. The cash is sealed in a cover to be opened after 3–5 days. Ironing the notes can also be done.
Laboratory area and pharmacy should follow the same precautions and physical distancing norms.
SANITIZATION AND DISINFECTION
Clinic or hospital rooms should be cleaned at the end of the session/every evening after office hours. If contact surface is visibly dirty, it should be cleaned with soap and water before disinfection. Before cleaning, the worker should wear disposable rubber boots, gloves (heavy duty), and a triple layer mask.
Start cleaning from cleaner areas and proceed toward dirtier areas.
All indoor areas such as reception consortium, patient waiting area and staircases, elevators, office/examination chamber rooms, and dispensing area should be mopped with a disinfectant such as 1% sodium hypochlorite or phenolic disinfectants. Box 3 lists the approved disinfectants.[16]
Box 3: List of disinfectants approved for use for COVID-19
70% ethyl alcohol
Isopropyl alcohol
Sodium hypochlorite solution, 0.5%–1% (5000ppm to disinfect surfaces)
Hydrogen peroxide
Quaternary ammonium
Citric acid
Chlorine dioxide
Peroxyacetic acid
-
Glutaraldehyde
High contact surfaces such as elevator buttons, handrails/handles and call buttons, public counters, intercom systems, equipment such as telephone, printers/scanners, and other office machines should be cleaned twice daily by mopping with a linen/absorbable cloth soaked in 1% sodium hypochlorite. Frequently touched areas such as tabletops, chair handles, pens, diary files, keyboards, mouse, mouse pad, and tea/coffee dispensing machines should specially be cleaned.
For metallic surfaces such as door handles, security locks, and keys, 70% alcohol can be used to wipe down the surfaces where the use of bleach is not suitable.
Carefully clean the equipment used in cleaning at the end of the cleaning process.
If available or feasible, it is preferable to fumigate all patient contact areas, like it is done for operation theater.
Disposal of biomedical waste
The disposal of biomedical waste should be strictly followed as per the Biomedical Waste Management Rules 2016.[17] The bags used for storing and transporting biomedical waste shall be in compliance with the Bureau of Indian Standards. Yellow, blue, red, and translucent bags/bins/containers are marked with biohazard symbol, hospital logo, and with bar coding to be supplied by common biomedical waste treatment and disposal facility. Chemical disinfection of the waste bins using hypochlorite solution (1%–2%) should be done frequently at a separate washing facility in the clinic, daily preferably, at least once a week.
Sanitary (housekeeping) workers must use separate set of cleaning equipment for toilets (mops and nylon scrubber) and separate set for sink and commode. They should always wear disposable protective gloves while cleaning a toilet. It is advisable to use sodium hypochlorite 1% and detergent soap powder with long handle angular brush for cleaning the toilet area. Always use freshly prepared 1% sodium hypochlorite as it becomes almost ineffective 24h after preparation.
Daily all the clothes, cloth masks should be soaked in 0.5% sodium hypochlorite solution for 15 min, and then immediately washed with soap and water. They should be dried in open terrace. Face shield should be dipped in soap water for 10 min, and washed and dried for use on next day.
Sodium hypochlorite is available in the strength of 5% solution. To prepare 1% sodium hypochlorite solution, add 10 mL of 5% sodium hypochlorite solution to 1L of cold water. Do not expose the solution to sunlight as it is rendered ineffective. Do not mix sodium hypochlorite to soap water or detergent as toxic gases may be produced.
Hand hygiene
Contact transmission occurs when contaminated hands touch the mucosa of the mouth, nose, or eyes; the virus can also be transferred from one surface to another by contaminated hands, which facilitates indirect contact transmission. Consequently, hand hygiene is extremely important to prevent the spread of the COVID-19 virus. It also interrupts the transmission of other viruses and bacteria causing common cold, flu, and pneumonia, thus reducing the general burden of disease. Hand hygiene is the most effective single measure to reduce the spread of infections through multimodal strategies. HCWs should perform hand hygiene using the proper technique and according to the instructions known as “My 5 moments for hand hygiene,” in particular,
Before putting on PPE and after removing it
When changing gloves
After any contact with a patient with suspected or confirmed COVID-19 virus, their waste, or the environment in the patients’ immediate surroundings, after contact with any respiratory secretions
Before food preparation and eating
After using the toilet[18]
Hand sanitizers
Centers for Disease Control and Prevention (CDC) recommends the use of alcohol-based hand sanitizers with greater than 60% ethanol or 70% isopropanol as the preferred form of hand hygiene in HCWs.[19] Apply the label-recommended amount of the product into the palm of your hand and rub your hands together, covering all surfaces, as you would do normally when washing. Allow the sanitizer to dry completely before you touch anything [Figure 1]. Hand sanitizing stations should be installed in reception area (especially at the entry) and near high contact surfaces.

- Hand sanitizing method with sanitizer. (Image adopted from https://www.who.int/gpsc/5may/hh-relay-procedure.pdf?ua=1)
Hand washbasin
Hands should be washed for at least 20s with soap and water. In clinics, a mobile unit of hand washbasin can be provided at the entry, preferably an elbow or foot operated.
PPE
PPE are protective clothing and equipment designed to protect both HCWs and patients from exposure to infectious agents, and to reduce the transmission of infectious microorganisms in healthcare facilities. PPE should be South India Textile Research Association (SITRA) tested and certified.
Components of PPE
Components of PPE from top to bottom are head cover, goggles, face shield, masks or respirators, gloves, coverall/gowns (with or without aprons), and shoe cover or boots. It also includes drapes for covering the patients.
Masks: They are the most important component of PPE because SARS-CoV2 targets the upper and lower respiratory tract. Triple-layer fluid-resistant medical mask and N95 respirator mask are the recommended masks. To provide the requisite air seal to the wearer, such masks are designed to achieve a very close facial fit. The use of cotton cloth masks as an alternative is not considered appropriate for protection of HCWs as the quality differs widely.[20] CDC[21] and Government of India[22] advise even homemade cloth face coverings to overcome shortages. Hence, patients attending the clinic or hospital should be advised or instructed to wear them before entering the healthcare facility. There is no uniform opinion as to what kind of masks are to be used and how long they can be used. N95 masks are recommended, but are in short supply; hence, an additional cheaper mask can be used on top of the N95 mask so that N95 mask can be reused. Figure 2 presents the right way to wear and remove N95 masks.
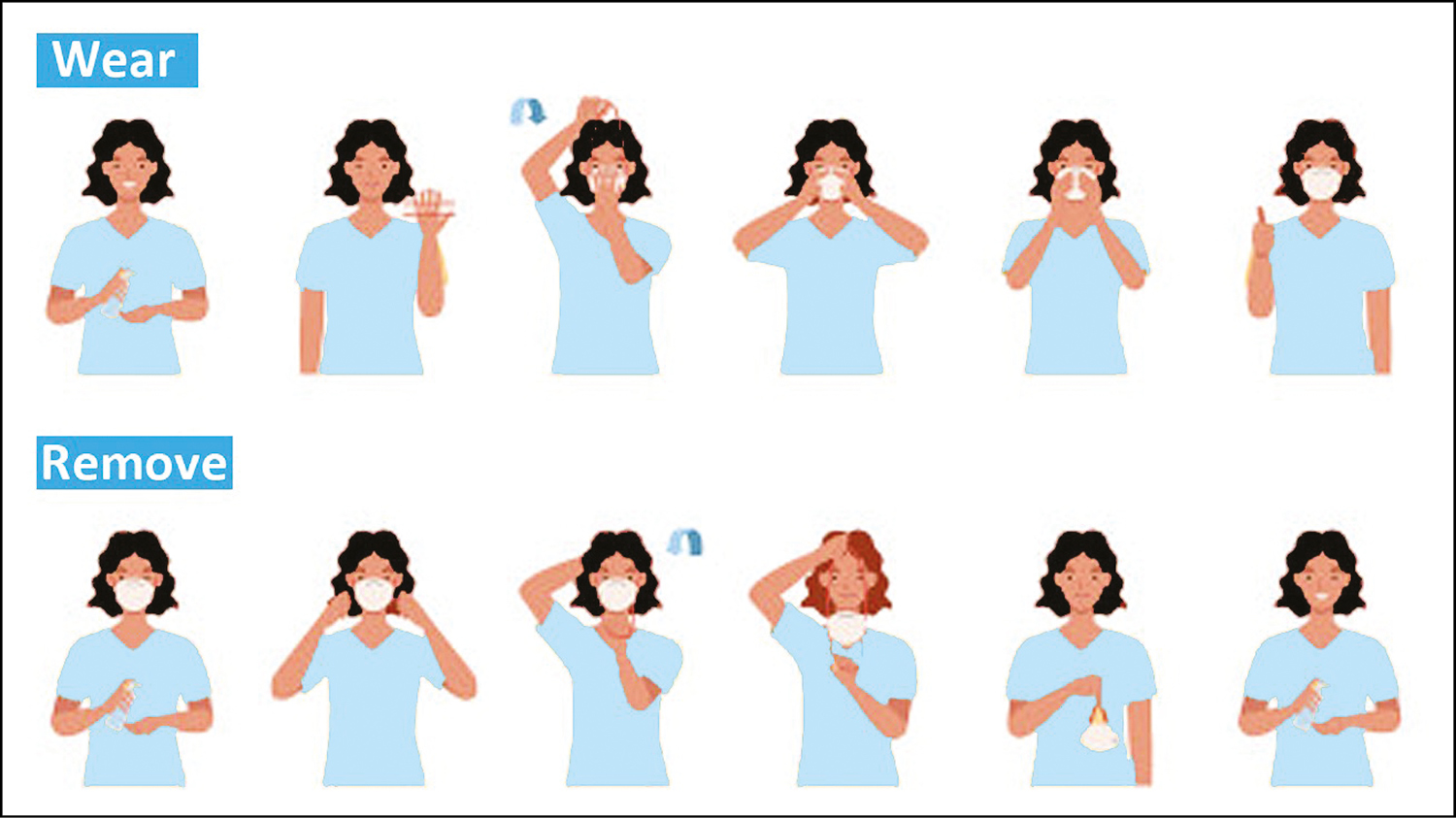
- How to wear and remove N95 masks
Gloves: Latex gloves are adequate for examination and performance of procedures. Nitrile gloves are preferred for housekeeping staff, over latex gloves, as they are resistant to damage by chemicals such as chlorine, which may be used as disinfectants, and are hypoallergenic. Avoid powdered gloves.
Face shield and goggles: Aerosol-generating procedures in dermatology such as dermabrasion, RF ablation, and ablative laser surgery can cause contamination of mucous membranes of the eyes, nose, and mouth of the HCW, and transmit infection. A full-face shield or visor or a surgical mask with integrated visor should be used in such a scenario. However, inadvertently touching the eyes/nose/mouth with a contaminated hand is a likely scenario. Hence, protection of the mucous membranes of the eyes/nose/mouth by using face shields/goggles is recommended as an integral part of standard and contact precautions.
Coverall gowns: They are to be used if there is a risk of fluids or blood from the patient splashing onto the HCW’s body, and hence they are not routinely needed. A plastic apron can also be worn over the gown for the entire time the health worker is in the treatment area if splashes are expected. In dermatology clinics, gowns/overall may be used for aerosol-generating procedures.
Head covers: Coveralls usually cover the head. Hair and hair extensions should fit inside the head cover. This is needed only if a COVID-19-positive patient is being treated.
Shoe covers/boots: Shoe covers should be made up of impermeable fabric and should be used over shoes to facilitate personal protection and decontamination.
General principles of PPE
The PPE should pass through stringent quality control and be adequately available.[23] Hand hygiene should always be performed before PPE use. If at any time PPE is damaged, it should be replaced. After duty, the PPE should be removed carefully avoiding contamination of the environment and coworkers. The type of PPE worn should be determined by evaluating risks.[24]
How to put on PPE—donning
Before donning, the HCW should have eaten, should be well hydrated, and should have gone to the washroom.[2526] All jewelry should be removed. The hair should be tied back. Check if the correct size of PPE is available. The donning should be done before entering the patient’s room. The order for putting on is gown/coverall followed by mask/respirator, eye protection, and gloves [Figure 3]. When the gown/coverall is put on, no skin should be exposed. If the respirator is not a good fit, DO NOT PROCEED.
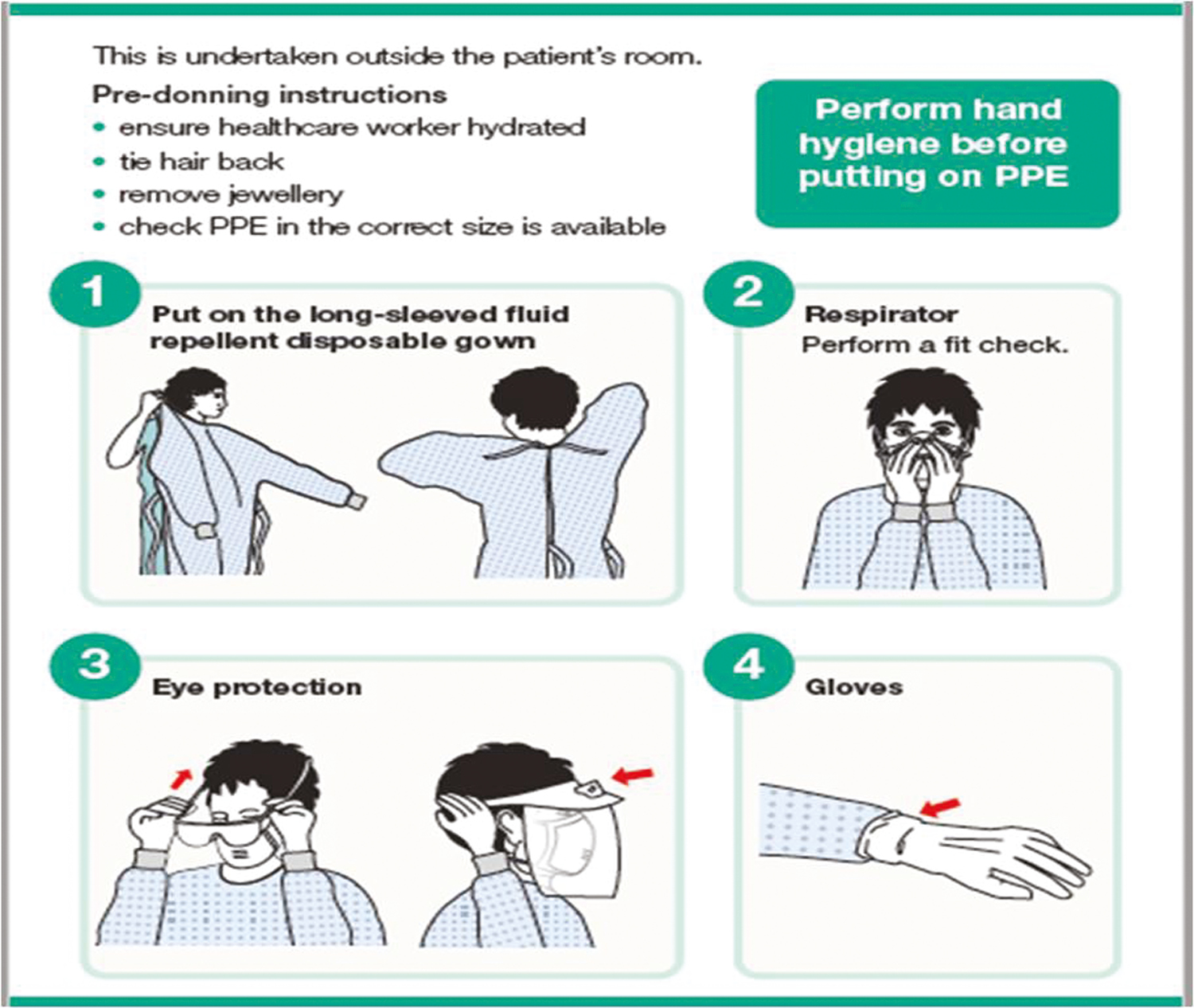
- Donning of PPE. (Adapted from www.gov.uk/government/publications/covid-19-personal-protective-equipment-use-for-aerosol-generating-procedures.)
How to remove PPE—doffing
The PPE should be removed in such a way that contamination is minimized.[2526] It should be done either before exiting the patient’s room or in a dedicated room for doffing. Remove plastic apron, if worn. The order is to remove gloves, followed by hand hygiene with alcohol rub, followed by removal of gown, eye protection, respirator/mask, and followed by hand hygiene again with soap and water [Figure 4]. Discard disposable items in a closed rubbish bin; put reusable items in a dry closed container.
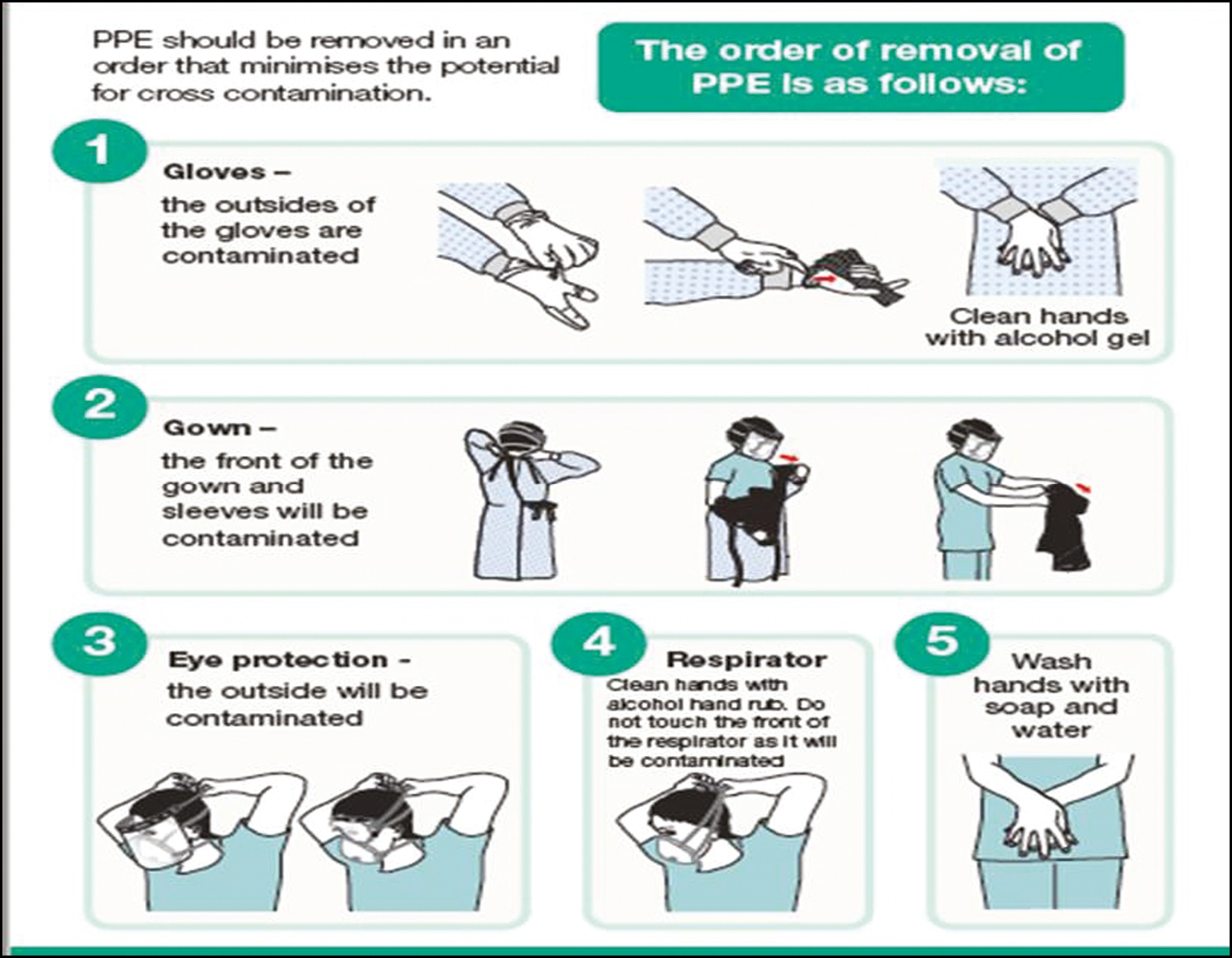
- Doffing of PPE. (Adapted from www.gov.uk/government/publications/covid-19-personal-protective-equipment-use-for-aerosol-generating-procedures)
Complications with PPE use
There can also be adverse reactions to the PPE,[27] particularly with extended use. Allergic contact dermatitis to gloves is more common with latex and powdered gloves. Overtight masks can cause skin indentations and abrasions. The filters may get clogged creating difficulty in breathing. Medical mask can cause throat irritation, folliculitis on the cheeks, aggravation of rosacea, and seborrheic dermatitis. The gowns can cause hyperhidrosis, folliculitis, and loss of barrier function due to irritation on extended use for more than 6h.
Rational use of PPE
It should be noted that full PPE kit is not necessary for routine dermatosurgical practice, except for high-risk procedures.[2324] The PPEs are to be used based on the risk profile of the HCW, settings, and type of activity [Table 2]. In case of aerosol-generating procedures, HCWs should use respirators, eye protection, gloves, and gowns. Others may use surgical masks.
| Setting | Target personnel or patients | Activity | Risk | Type of PPE or procedure | Remarks |
|---|---|---|---|---|---|
| Point of entry | Reception | Provide information/registration | Low | If there is a physical barrier—no PPE | Ideally, build transparent partition to create a barrier (no PPE required) or minimum distance of 1 m needs to be maintained. |
| If there is no physical barrier—Triple-layer medical mask | |||||
| Temperature recording station | Record temperature with handheld thermal recorder | Low | Triple-layer medical mask gloves | ||
| Healthcare facility—Outpatient. All hospitals should identify a separate triage and holding area for patients with influenza-like illness. If there is no triage area/holding area for patients due to resource constraints, such hospitals will follow the above guidance for general OPD. | Screening | Preliminary screening not involving direct contact | Moderate | N95 mask, gloves, provide triple-layer mask to patient | To maintain physical distance of at least 1 m. Patient to be masked |
| Waiting area | Nurses/paramedic interacting with patients | Moderate | N95 mask gloves | Minimum distance of 1 m needs to be maintained | |
| Doctor’s chamber | Clinical management (doctors, nurses) | Moderate | N95 mask, gloves | No aerosol-generating procedures should be allowed | |
| Waiting area | Visitors accompanying young children and elderly | Low | Triple-layer medical mask | No other visitors should be allowed to accompany patients in OPD settings. Those allowed should practice hand hygiene | |
| Patients with influenza-like illness | Any care activity | Moderate | N95 mask, gloves, eye protection | Maintain physical distance of at least 1 m. Provide medical mask to the patient. Immediately move the patient to a separate room away from others. Perform hand hygiene and have the patient perform hand hygiene | |
| Patients with no symptoms suggestive of COVID-19 | Any care activity | Low | Triple-layer surgical mask | Perform hand hygiene and have the patient perform hand hygiene | |
| Patient room/ward | HCWs | Not providing direct care to COVID-19 patients, or not attending aerosol-generating procedure | Moderate | Medical mask, gown, gloves, eye protection (goggles or face shield) | Perform hand hygiene |
| HCWs | Providing direct care to COVID-19 patients, or attending aerosol-generating procedure | High | N95 mask or equivalent, gown, gloves, eye protection, apron | Perform hand hygiene | |
| Sanitary staff | Cleaning frequently touched surfaces/floor/cleaning linen | Moderate | N95 mask, gloves | ||
| Cleaners | Entering the room of COVID-19 patients | Moderate | Medical mask, gown, heavy-duty gloves, eye protection (if risk of splash from organic material or chemicals is anticipated), closed work shoes | Perform hand hygiene | |
| Visitors | Entering the room of a COVID-19 patient | Moderate | Medical mask, gown, gloves | Maintain physical distance of at least 1 m, perform hand hygiene | |
| Laboratory | Lab technician | Manipulation of respiratory samples. Specimen handling for molecular testing would require BSL-2 or equivalent facilities. Handling and processing of specimens from cases with suspected or confirmed COVID-19 infection that are intended for additional laboratory tests, such as hematology or blood gas analysis, should apply standard precaution | Medical mask, eye protection, gown, gloves | Maintain physical distance of at least 1 m, perform hand hygiene |
Disinfection of instruments
Use disposable equipment wherever and whenever feasible such as disposable biopsy punches and ear buds for the application of peels or for chemical cautery. Table 3 enumerates the preferred disinfection methods of various instruments used in dermatology clinic.
| Instruments used for procedures | Disinfection method |
|---|---|
| Comedone extractors, electrosurgery tips, microdermabrasion (MDA) tips, cryosurgery equipment, microdermabrasion tips, dermabrasion brushes, hair transplant instruments | Isopropyl alcohol, glutaraldehyde, Ethylene oxide (ETO) |
| Chemical peels, sterile cotton balls, container, brushes (should be avoided) | UV disinfection, ETO, UV sterilization |
| Microdermabrader body | Hypochlorite mist spray between cases |
| LED devices | Face piece for contact with isopropyl alcohol |
| Dermapen and cartridges, microneedles | Isopropyl alcohol between sessions, ETO, glutaraldehyde |
| Mirrors | Isopropyl alcohol |
| Botulinum toxin and fillers | Materials are often prefilled sterile syringes; cannulas and needles are disposable |
| Cooling methods—gel pads | Cleaned with isopropyl alcohol/ice cubes in sterile gloves, avoid direct cooling with gel pads if possible |
| Platelet-rich plasma (PRP) blood collection, injection syringes, and needles | Better to use presterilized disposable material and avoid indigenous methods |
| Thread lifts and suture suspension | Are often presterilized and prepackaged material |
| Autologous micrografts for hair regeneration or skin rejuvenation | Trays should be autoclaved, punches and cups are already presterilized and prepacked |
| Phototherapy chambers | Spray with isopropyl alcohol |
Training the clinic staff
Educate the staff about COVID-19, and why it is important to contain the outbreak. They have to be trained on the policies and practices to minimize the spread of infection. A task-specific training can be given to them on preventing spread of infectious agents. Educate staff on how to advise patients about changes in office procedures (e.g., calling before arrival if the patient has any signs of a respiratory infection and taking appropriate preventive actions). Ensure that the clinical assistants know the right way to use and take off PPE safely.
Staff should be made aware about them being quarantined if they are exposed to COVID-19.
RECOMMENDATIONS FOR PROCEDURES
As stated earlier, the choice of procedure and timing of procedure should consider the following:
Risk of SARS-CoV2 transmission
Urgency/need of the procedure
Risk of aerosol generation during the procedure
Risk of SARS-CoV2 transmission
Below is the general risk stratification for different cutaneous procedures and surgeries. It has to be stated here that all cutaneous procedures are of considerably low risk as compared to surgeries in other specialties such as dental, ENT, and general surgery, so the categories mentioned below are not comparable to the terminologies used in other specialties, and this should be taken in this context. This categorization is specific only for cutaneous surgeries.
Low-risk procedure
These are procedures of shorter duration, without risk of aerosol or plume generation, and procedures on limbs or lower torso of short duration.
The examples of such procedures include all bedside investigations such as KOH mount or smear preparation, injections such as intralesional injections, nonfacial injectables and fillers, contact cryotherapy, and peels.
Require regular surgical mask. Patient to wear mask
Medium-risk procedure
These are the procedures that are associated with minimal invasiveness and bleeding, invasive procedures on head, neck, and upper torso of any duration, and any procedure on any part of the body for long duration (e.g., liposuction, scalp biopsy, treatment of growths on scalp, microneedling, face fillers and toxin injections, simple excision, and closure, which can be finished quickly, and fat graft for nonfacial areas).
These procedures would require face shield and N95 respirator. Patient needs to wear mask.
High-risk procedures
All procedures in a COVID-19-positive patient are high risk.
High-risk procedures are any procedure that necessitates an open nasal or oral airway of the patient (e.g., intraoral or intranasal procedures such as mucosal biopsy, treatment of intraoral or intranasal warts, skin cancer surgeries, plasties, procedures involving aerosol generation, ablative lasers, and hair transplantation.
These procedures require full PPE.[28]
Low-risk procedures are less invasive procedures requiring minimal exposure time. These can be resumed first after the restrictions are lifted. Medium-risk procedures should be performed based on the need and significance. For example, biopsy should be done only if it carries important potential contribution in treatment decision-making. Excision and closure for benign lesions should be done on discretion basis. Surgeries that provide significant immediate relief should be taken up, such as draining the abscess, procedures for hidradenitis suppurativa, draining acute paronychia and severe ingrown nail causing pain or severe discomfort, painful skin and nail tumors (such as glomus tumors), and premalignant and malignant skin tumors.
High-risk procedures are to be avoided in containment zones and in areas or states where the governmental regulations disallow such procedures. They are to be undertaken only in areas where governmental has allowed routine surgical work to be performed.
Elective cosmetic surgeries requiring prolonged exposure time should be postponed in a given state or area till governmental agencies permit elective surgeries.
An important consideration should be the age of the patient and also of the HCW, including the treating doctor. COVID-19 affects the elderly and those with low immunity more severely. Hence, the elderly patients and the elderly healthcare staff above the age of 60 years should be handled carefully. Offer teledermatology to a patient older than 60 years, and postpone procedures unless it is life saving. If any of the staff is older than 60 years, ask him/her to stay at home. Younger staff with comorbidities such as diabetes and hypertension, likewise, if the treating doctor is older than 60 years, it is preferable for him to let a younger colleague perform the procedure.
Urgency of the procedures
Surgery for minimally symptomatic or asymptomatic benign lesions, such as cysts, lipomas, acrochordons, scars, and keloids, should be deferred till governmental agencies state that elective surgeries can be performed.[29]
Non-life-threatening skin cancers (e.g., BCC, DFSP), which are slowly progressive and are not likely to cause severe functioning impairments, may be either treated by cryosurgery or noninvasive means or postponed if feasible based on the individual situation.
Skin cancers needing urgent intervention include squamous cell carcinoma and melanoma. These should be taken up as early as possible with all protective measures and protocols.
Risk of aerosol generation during the procedure
The procedures, which generate aerosol in the minor operating room, should be performed with appropriate PPE. These procedures include RF ablation, dermabrasion, microdermabrasion, and ablative lasers. Wherever feasible, these procedures can be replaced by cryosurgery or scalpel excision or nonablative procedures. Where minor aerosol is generated, such as a small wart, a smoke evacuator should be used and the treating doctor should wear a shield. The power setting of RF machine should be as low as possible.[30]
Patient selection
All patients symptomatic for flu symptoms should not be taken for surgery even if negative for SARS-CoV2.
All the patients taken up for procedures should be screened for SARS-CoV2. Patient will have to be screened for:
COVID-19 symptoms[31]
Exposure to a proven case of COVID-19
Travel to a hotspot of COVID-19
Any patient having a positive history to any of the aforementioned would have to have their procedure deferred for 3 weeks. Negative patients can be considered for the procedure and be taken for testing. Aarogya Setu app has also been recommended by the Government of India as a method of screening.
Testing options
As stated earlier, dermatosurgical practice has to adapt to the challenge like it did in the Hepatitis B and HIV scenarios. One way to do is to perform proper testing before conducting the procedure. However, rapid testing is either not available freely or is expensive. However, in the near future, it is expected that rapid testing becomes more easily available and accessible. In such a scenario, it would be possible to perform procedures after appropriate testing. Testing is subject to governmental regulations and are subject to changes. Surgeons are advised to follow their concerned state governmental guidelines.
Polymerase chain reaction testing: PCR tests the antigen or viral load. It is taken from a nasal swab or cough expectorant. It is positive in the first week of the illness and then becomes negative as the patient recovers. It is a sign of active infection. In one study, asymptomatic patients had swab positivity for a total duration of 18 days.[32] Diagnostic test sensitivity was shown to be 54% at 8–14 days by PCR technique [Table 4].[33] Strategy for COVID-19 testing in India recommended by ICMR[34]:
| DAYS AFTER SYMPTOM ONSET | |||
|---|---|---|---|
| SARS-CoV 2 test | 1-7 | 7-14 | 15-39 |
| RNA by RT PCR | 67% | 54% | 45% |
| Total antibody | 38% | 90% | 100% |
| Ig M | 29% | 73% | 94% |
| Ig G | 19% | 54% | 80% |
All symptomatic (ILI symptoms) individuals with history of international travel in the last 14 days.
All symptomatic (ILI symptoms) contacts of laboratory confirmed cases.
All symptomatic (ILI symptoms) health care workers/frontline workers involved in containment and mitigation of COVID-19.
All patients of Severe Acute Respiratory Infection (SARI).
Asymptomatic direct and high-risk contacts of a confirmed case to be tested once between day 5 and day 10 of coming into contact.
All symptomatic ILI within hotspots/containment zones.
All hospitalised patients who develop ILI symptoms.
All symptomatic ILI among returnees and migrants within 7 days of illness.
No emergency procedure (including deliveries) should be delayed for lack of testing.
NB: ILI case is defined as one with acute respiratory infection with fever = 38°C AND cough. SARI case is defined as one with acute respiratory infection with fever = 38°C AND cough AND requiring hospitalization. All testing in the above categories is recommended by real time RT-PCR test only.
Once this test becomes available freely, PCR immediately before the procedure can be considered for taking up the patient for surgery. However, the current cost of this test precludes its use for minor surgeries where cost of testing may be more than or equal to the cost of the procedure itself. However, for procedures such as hair transplantation, vitiligo surgery, extensive body hair removal, and liposuction, such testing can be considered, in areas where governmental regulations allow nonessential procedures to be performed.
Special informed consent will have to be obtained both for surgery and for testing. Table 4 shows the sensitivities of different tests.
HCWs
Testing for clinic staff has not been recommended by ICMR. Hence, proper screening as aforementioned should be done.
General safety recommendations
Paperwork should be minimized, and all forms should be preferably electronic.
Patient should be counseled and prepped for the procedure.
Minimum essential manpower should be inside the minor operating room. Trainee doctors should be in another room where a television set may be provided connected with Wi-Fi. The livestreaming of the procedure on television screen is possible using an ordinary smartphone.
Procedures to be performed in well-ventilated room, avoiding air-conditioned (AC) rooms. Procedures should be spaced out.
To minimize fomite transmission, the operating room should have only those equipment, which are needed for the patient. All other nonessential equipment and furniture should be removed.
All patients should be assumed to be asymptomatic COVID-19 patient and should be given masks even if tested negative for SARS-CoV2, to prevent them getting infection or vice versa if they are in incubation period.
HCW should wear goggles, mask, and gloves. Wear face shields while performing procedures on the face.
Both the patient and the doctor should minimize contact with surfaces. Both doctor and patient should avoid carrying wallets, mobile phones, watches, belts, rings, bangles, and bindis to procedure rooms.
Minimize the use of handheld mirrors and marking pens. Marking pens can be cleaned with spirit in between procedures.
Use plume evacuation systems, preferably with filters that remove particulates to 0.1 microns known as ultralow particulate air filters (HEPA or ULPA filter). Avoid nonmedical-grade fume evacuators and vacuum cleaners for fume evacuation.
Follow-up visit can be made infrequent and need-based, patient should be advised sufficiently with all precautions to prevent possible postsurgical complications such as gaping of the wound, wetting of the wound, and excessive use of the operated part. Unless the patient develops some warning signs of complications, such as excessive pain, oozing or pus discharge from surgical site, hematoma formation, bleeding, and excessive swelling, in the follow-up of excisional procedures, the patient can come directly on the day of suture removal.
All the used materials should be disposed properly according to recommendations.
In between procedures, examination beds, countertop, doorknobs, and examination light buttons/handles should be wiped with products, which are approved by World Health Organization (WHO) for disinfecting surfaces.
Special considerations for each type of procedure
Bedside procedures
Common bedside procedures performed include KOH mount, Tzanck smear, comedone extraction, needling, chemical cautery, and cryosurgery. Cryosurgery by spray has less risk as compared to electrocautery and RF, and hence may be preferred. Aerosol-generating procedures such as electrosurgery and radiosurgery need special precautions.
Major OT procedures
To rapidly reduce the viral load within the OT, a high frequency of air changes (25 per hour) is desirable.[35] In a major OT, the necessity for AC environment itself would be a risk factor, and a standard OT is generally designed to be at positive pressure relative to the surrounding air. To reduce dissemination of the virus beyond the OT, a negative-pressure environment is ideal. However, as stated earlier, most dermatological surgical procedures do not need a major OT.
Common cutaneous surgeries, such as hair transplantation and vitiligo surgery, need to be considered as high risk, for reasons already mentioned, and appropriate PPE for face and body need to be used. Risk stratification of dermatosurgical procedures is given in Table 5.
| Acne surgery | Subcision | Moderate risk |
| Punch grafting | ||
| Punch elevation | ||
| Nail surgery | Low risk | |
| Vitiligo surgery | Punch grafting | Low risk |
| Other types of vitiligo surgery including epidermal suspension methods needing dermabrasion of recipient area | HR, avoid surgery on lip, nose, chin | |
| Hair transplantation (HT) | HR, postpone HT to moustache, beard area | |
| Excisions of cysts, lipomas | Face | HR |
| Other body sites | Low risk |
HR = high risk
Before and after surgery, the following should be taken into consideration[36]:
Remove clothes worn from home and keep in garment bag
Wear scrub clothes after arrival at hospital
After separating from the patient, remove scrub clothes; consider showering before changing into a clean scrub suit or home clothes
Wash hands frequently and maintain safe social distancing
Consider removing clothes and washing them on arrival at home
Aesthetic procedures
Aesthetic procedures are generally for rejuvenation and cosmetic enhancement, though they are used for the treatment of diseases such as pigmentation and scarring. They include in office minimally invasive bedside techniques, usually of short duration between 15 and 40 min, such as microdermabrasion, microneedling or dermapen, chemical peels, platelet-rich plasma, laser- or energy-based device rejuvenation, and injectables such as toxin and fillers.
These procedures can be performed safely, using the following precautions:
Patients who are symptomatic or are COVID-19 positive should not undergo any aesthetic procedure. All procedures need to be postponed as stated earlier.
Patients who have recently recovered from the COVID-19 infection can undergo any procedure as they are likely to have developed antibodies and are expected to be of no risk to other patients or clinicians and staff. However, reinfection has been described in COVID-19, and hence appropriate PPE need to be used.
For specific procedures, following points need to be kept in mind:
Use of hypochlorous acid as antiseptic spray before dermal fillers is being recommended and may be used for other aesthetic procedures too.[37]
Chloroquine and hydroxychloroquine causes Botulinum toxin A to remain at site by inhibiting toxin binding and internalization.[38]
Patients on isotretinoin may have altered mucociliary clearance and lung function, and hence caution needs to be exerted.[39] Box 4 shows specific points to be considered while choosing a patient for aesthetic procedures. Table 6 lists all the different aesthetic procedures and their risk stratification.
| Procedure | Facial area | Nonfacial area |
|---|---|---|
| Chemical peel | MR | LR |
| Spot peels may be preferred | ||
| Botulinum toxin/filler injections | Mid and lower face—MR | For axillary and palmar hyperhidrosis, neck and hand rejuvenation—LR |
| Forehead—LR | ||
| Thread lifts | MR | LR |
| Microneedling with dermaroller | MR | LR |
| Platelet-rich plasma | MR | MR |
| Microdermabrasion | LR | LR |
| Sclerotherapy | MR | LR |
MR = moderate risk, LR = low risk
Box 4: Probable protocols for aesthetic procedures
There are four key factors that need to be addressed to conduct minimally invasive procedure conduction in COVID era, which are as follows:
Rule regarding proximity of patient with physician while conducting procedure: This can be addressed by the use of full body cover by physician for any procedure, especially aerosol-generating procedures. Full body cover for assistant in procedure room is also mandatory.
Contact of device to the patient: Here all the protocol regarding disinfection of the movable and immovable device to be undertaken as listed in Table 3.
Room/chair or bed of procedure has to be sanitized in between patients. Also having multiple procedure rooms would be an added advantage here, as it gives time and space between sanitization.
Patient undergoing the procedure: Once the proximity rules with full-body cover, device, and room sterility in between procedures are achieved, then the patient factor is crucial and at the discretion of physician and patient with proper consent to conduct procedures.
Laser procedures
Airborne contaminants are associated with certain lasers such as ablative fractional lasers, high-peak power ultrashort-pulsed lasers such as nano- and picosecond lasers.[40] Apart from airborne contaminants, one has to take care of lasers with contact cooling handpiece such as diode laser where the tip can come in contact near the mucosal areas such as upper lip and chin. It should be clarified here that risk due to aerosol after laser or RF procedures is considerably less than aerosol due to mechanical drilling procedure as the heat generated by the tissue interaction with these devices is likely to be inimical to the virus. Other devices such as excimer lamp and skin-tightening devices, all have probes that come in close contact with the skin. Thorough cleaning of the tip is mandatory in the setting of COVID-19. Microneedle radiofrequency (MNRF) devices do cause pinpoint bleeding, and they can increase the risk to medical personnel.[41]
It is best to postpone cosmetic laser surgery until the governmental agencies allow nonessential procedures to be performed.
While performing, modifications such as the use of shield and smoke evacuators need to be used.
Sterilize laser handpieces before and after every use. In case of contact lasers such as diode, excimer lamp, or RF, better to use disposable cling wrap for handpiece. The laser body can be sterilized with any one of the approved disinfectants. Considering the cost-effectiveness, sodium hypochlorite solution should be sprayed on laser equipment, but protecting the optics. The laser optics can be cleaned with isopropyl alcohol or 70% ethyl alcohol. Patient bed and laser room should be sprayed with sodium hypochlorite solution in between and after each procedure.
It is best to surgically prepare the area to be treated with proper disinfection such as ethyl alcohol. It is best to wait for 15 min after preparation, and clean the area again with water, so as to avoid potential burns because of disinfectants or sanitizers containing alcohol. Risk stratification for energy-based devices is given in Tables 7 and 8.
| Procedure | Technology | Risk on face, neck, and scalp | Risk on other parts | Explanation |
|---|---|---|---|---|
| Ablative and Ablative fractional resurfacing | CO2 laser and Er:YAG laser | HR (aerosol) | HR (aerosol) | Plume and aerosol generated. |
| Distance between operator and patient is less. | ||||
| Raw areas are created on patients. | ||||
| Ablative radiofrequency (RF) | HR (aerosol) | HR (aerosol) | ||
| Nonablative lasers and nonablative fractional lasers | Erbium glass | MR | LR | No or minimal fumes generated |
| Thulium | ||||
| IPL (nonhair removal), excimer | ||||
| Q-switched Nd:YAG except carbon peel. | MR | LR | ||
| Laser toning | ||||
| Tattoo removal | HR | MR | ||
| No wounds and usually less painful procedures | ||||
| Carbon peel | Q-switched Nd:YAG laser | HR | HR | A lot of laser plume are generated |
| Laser hair reduction | 810 diode, long-pulsed Nd:YAG, alexandrite, triple wavelength | HR | HR | Significant laser plume is generated |
| IPL | MR? | |||
| Vascular lasers | Pulse dye laser | HR | HR | Significant laser plume is generated |
| LLLT | LR | |||
| Energy-based devices for skin tightening | Monopolar and bipolar RF, HIFU, fractional RF, shockwaves, etc. | MR | LR | No or minimal laser plumes |
| No raw areas |
HR = high risk, MR = moderate risk, LR = low risk, LLLT = Low level laser therapy, HIFU = High intensity frequency ultrasound, IPL = Intense pulse light
| Risk category for laser procedure | Precautions for healthcare worker | Precautions for patients |
|---|---|---|
| High risk | Full body cover with surgical gown with head cover and N95 mask and face shield. | 1. Wash the area with soap and water before the procedure |
| Double gloves. | 2. Disinfect with surgical spirit before the procedure, wait for 10 min, clean again with distilled water. | |
| Smoke evacuator with HEPA or ULPA filter where needed. | 3. If area around the nose and mouth is not going to be treated, ask patient to wear a surgical mask and goggle. | |
| 4. As these procedures can create raw areas, the patient is advised to use a full facial mask till complete healing | ||
| 5. Full surgical washed gown | ||
| Moderate risks | Apron and N95 mask and face shield. | 1. Wash the area with soap and water before the procedure |
| Double gloves. Head cover where spillage is expected | 2. Disinfect with surgical spirit before the procedure, wait for 10 min, clean again with distilled water. | |
| Smoke evacuator with HEPA or ULPA filter where needed. | 3. If area around the nose and mouth is not going to be treated, ask patient to wear a surgical mask and goggle. | |
| 4. Ask patient not to touch the treated area. | ||
| 5. Full surgical washed gown | ||
| Low risk | Surgical mask, head cap, gloves. | 1. Wash the area with soap and water before the procedure |
| 2. Disinfect with surgical spirit before the procedure, wait for 10 min, clean again with distilled water. | ||
| Mask for the patient |
Phototherapy
Phototherapy using closed chamber poses special risks.
Phototherapy should be by appointment alone. Ask the patient to use mask while entering the chamber and use hand sanitizers before entering and at the time of leaving the cubicle. Patients are encouraged to buy their own protective goggles and use them. The staff should disinfect the high touch areas such as handles between the patients. Risk categorization for different types of phototherapy is enumerated in Table 9.
| Type of phototherapy | Risk | Comments |
|---|---|---|
| Phototherapy chamber | Moderate risk | Less ventilated closed space. |
| Hand and foot phototherapy | Low risk | Fomites if generated will be risk for next patients |
| Scalp phototherapy | Low risk | Scalp machine can be held by patient |
| Targeted phototherapy | Low risk on body | |
| Moderate risk on face |
MEDICOLEGAL IMPLICATIONS
There have been apprehensions in the minds of the dermatologists of legal implications of practice of procedural dermatology during the outbreak of COVID-19. Section 269 and Section 270 of the Indian Penal Code have also been in the limelight. There have also been directions and orders made by appropriate authorities under the Epidemic Diseases Act 1897 and Disaster Management Act 2005, to prevent the spread of the disease. Every citizen to whom it applies is bound to comply with the orders failing which, action against Section 188 of the Indian Penal Code for disobedience of order duly promulgated by public servant can be taken. One should be aware of such orders by the district or state authorities or the Central Government, which are issued from time to time.
It is necessary to examine if procedural dermatology has bearing on the risks of allegations of medical negligence. To that end it is important to note that every doctor owes one’s patient duty of care in deciding whether to undertake to treat a patient, duty of care in deciding what treatment to administer, and duty of care in the manner of administration of the treatment.
Except in a case of an emergency, no doctor is bound to treat every patient that presents to him/her. As a patient with COVID-19 infection could be asymptomatic at the time of presentation for the procedure, counseling of the patient should be done and explore the possibility of deferring the procedure. An important duty of care includes in deciding what treatment to administer to the patient. The options of treatment are to be discussed with the patient, and the risks involved with the procedure, especially the increased risk of transmission of COVID-19, should be discussed. The manner of administration is also an important duty of care. If the procedure is essential to be done, then the patient can be taken up for the procedure with all necessary precautions and as per the current recommendations.
For a patient (legal representatives of a patient in the event of death of the patient) to succeed in a claim for compensation, it must be proved that there was a failure of the doctor to exercise duty of care, and this failure was the proximate and direct cause of the loss or injury or death suffered by the patient.
The onus of proving negligence is on the person who alleges it, and it is on the patient or the legal representatives to prove that the doctor has failed in the duty to take care because of which the patient suffered any loss/injury/death due to COVID-19 infection.
The Section 269 of the Indian Penal Code applies when there has been negligence, which has led to the spread of the disease. If due care and caution has been taken as per current recommendations then there is no question of negligence, and therefore Section 269 cannot be made applicable. Section 270 of the Indian Penal Code will come into play only if there has been deliberate act to spread the infection. No doctor would deliberately spread the infection, and hence this would not apply to doctors.
To sum it up, it is reiterated that the question of negligence would not arise if the standard practices and protocols, which are currently acceptable, are adopted. However, it is important to go ahead with a procedure only if one’s professional judgment states that it would be prudent to do so.
CONCLUSION
Importantly, it has been shown in studies that the surgical outcomes in the current COVID-19 situation are guarded, and could even be detrimental to the patient.[3] Hence, there is a need for optimal safety recommendations and/or protocols to be developed so as to assess the need of the procedure, fitness of the patient to undergo the procedure, risk to the dermatologist, paramedical staff and subsequent patients, and how soon the procedure needs to be performed. The patients need to be screened and assessed on the urgency of the procedure, and then classified into low-risk and high-risk categories.[42]
The aforementioned recommendations are based on the best available evidence at this time, and are subject to change. It is important to understand that even with following all of the aforementioned, the risk of contracting or transmitting COVID-19 cannot be quantified to be zero. Doctors are advised to make their own best judgment with respect to their practice and patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- CIRD-F: spread and influence of COVID-19 in China. J Shanghai Jiaotong Univ Sci. 2020;25:147-56.
- [Google Scholar]
- Risk factors for disease severity, unimprovement, and mortality of COVID-19 patients in Wuhan, China. Clin Microbiol Infect 2020 [Epub ahead of print] doi: 10.1016/j.cmi.2020.04.012
- [Google Scholar]
- COVID-19: guidance for triage of non-emergent surgical procedures. 2020. Available from: https://www.facs.org/covid-19/clinical-guidance/triage
- [Google Scholar]
- Community transmission of severe acute respiratory syndrome coronavirus 2, Shenzhen, China, 2020. Emerg Infect Dis. 2020;26 [Epub ahead of print] doi: 10.3201/eid2606.200239
- [Google Scholar]
- Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199-207.
- [Google Scholar]
- Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA 2020 [Epub ahead of print] doi 10.1001/jama.2020.3227
- [Google Scholar]
- Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564-7.
- [Google Scholar]
- Emergency management for preventing and controlling nosocomial infection of the 2019 novel coronavirus: implications for the dermatology department. Br J Dermatol 2020 [Epub ahead of print] doi 10.1111/bjd.19011
- [Google Scholar]
- Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104:246-51.
- [Google Scholar]
- Guidelines for environmental infection control in health-care facilities. 2003. Internet. Available from: https://www.cdc.gov/infectioncontrol/guidelines/environmental/background/air.html.
- [Google Scholar]
- Standard and transmission based precautions. (internet) Accessed from: https://www2.health.vic.gov.au/public-health/infectious-diseases/infection-control-guidelines/standard-additional-precautions.
- [Google Scholar]
- Social distancing, quarantine, and isolation. Keep your distance to slow the spread. [Internet]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html.
- [Google Scholar]
- To beat COVID-19, social distancing is a must. [Internet]. [19thMarch 2020,]. Available from: https://directorsblog.nih.gov/2020/03/19/to-beat-covid-19-social-distancing-is-a-must/.
- Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2) Science. 2020;368:489-93.
- [Google Scholar]
- Coronavirus disease (COVID-19) advice for the public. [Internet]. []. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
- [Google Scholar]
- List N: disinfectants for use against SARS-CoV-2. [Internet]. [Cited 2020 Apr 25]. Available from: https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2.
- [Google Scholar]
- Bio-medical waste management rules. New Delhi, India: Gazette of India, Extraordinary, Part II, Section 3, Sub-Section (i), Government of India Ministry of Environment, Forest and Climate Change; 2016.
- Obligatory hand hygiene against transmission of COVID-19. [Internet]. [Cited 2020 Apr 25]. Available from: https://www.who.int/docs/default-source/inaugural-who-partners-forum/who-interim-recommendation-on-obligatory-hand-hygiene-against-transmission-of-covid-19.pdf.
- [Google Scholar]
- Hand hygiene recommendations. Guidance for healthcare providers about hand hygiene and COVID-19. [Internet]. [April 27, 2020. cited 2020 Apr 30]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/hand-hygiene.html.
- [Google Scholar]
- A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015;5:e006577.
- [Google Scholar]
- Use of cloth face coverings to help slow the spread of COVID-19. [Internet]. [April 14, 2020. cited 2020 Apr 25]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/diy-cloth-face-coverings.html.
- [Google Scholar]
- Advisory on use of homemade protective cover for face & mouth. [Internet]. [April 14, 2020. cited 2020 Apr 25]. Available from: https://www.mohfw.gov.in/pdf/ Advisory&ManualonuseofHomemadeProtectiveCoverfor Face&Mouth.pdf.
- Guidelines on rational use of personal protective equipment. 2020. Ministry of Health and Family Welfare Directorate General of Health Services. [Internet]. [Cited 2020 Apr 25]. Available from: https://www.mohfw.gov.in/pdf/GuidelinesonrationaluseofPersonalProtectiveEquipment.pdf.
- [Google Scholar]
- Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19): interim guidance. Geneva, Switzerland: World Health Organization; Updated 8 April 2020. [Internet]. [Cited 2020 Apr 25]. Available from: https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nCoV-IPCPPE_use-2020.2-eng.pdf.
- [Google Scholar]
- Guide to donning and doffing standard personal protective equipment (PPE) Public Health England. [Internet]. [Cited 2020 Apr 25]. Available from: www.gov.uk/government/publications/covid-19-personal-protective-equipment-use-for-non-aerosol-generating-procedures.
- [Google Scholar]
- Guidance on the use of personal protective equipment (PPE) for aerosol generating procedures (AGPs) Last updated 10 April 2020. [Internet]. [Cited 2020 Apr 25]. Available from: www.gov.uk/government/publications/covid-19-personal-protective-equipment-use-for-aerosol-generating-procedures.
- [Google Scholar]
- Personal protective equipment (PPE) [Internet]. [Cited 2020 Apr 25]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/using-ppe.html.
- [Google Scholar]
- Precautions for operating room team members during the COVID-19 pandemic. J Am Coll Surg 2020 [Epub ahead of print] doi 10.1016/j.jamcollsurg.2020.03.030
- [Google Scholar]
- Recommendations on dermatologic surgery during the COVID-19 pandemic. J Am Acad Dermatol 2020 [Epub ahead of print] doi 10.1016/j.jaad.2020.04.034.
- [Google Scholar]
- SAGES and EAES recommendations regarding surgical response to COVID-19 crisis. [Internet]. []. Available from: https://www.sages.org/recommendations-surgical-response-covid-19.
- [Google Scholar]
- Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020 [Epub ahead of print] doi 10.1001/jama.2020.2648
- [Google Scholar]
- Different longitudinal patterns of nucleic acid and serology testing results based on disease severity of COVID-19 patients. Emerg Microbes Infect. 2020;9:833-6.
- [Google Scholar]
- Antibody responses to SARS-CoV-2 in patients of novel coronavirus disease 2019. Clin Infect Dis 2020 [Epub ahead of print] doi 10.1093/cid/ciaa344
- [Google Scholar]
- (internet) Available from: https://www.icmr.gov.in/cteststrat.html.
- Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can J Anaesth. 2020;67:732-45.
- [Google Scholar]
- Protecting surgical teams during the COVID-19 outbreak: a narrative review and clinical considerations. Ann Surg 2020 [Epub ahead of print] doi 10.1097/SLA.0000000000003926
- [Google Scholar]
- Use of hypochlorous acid as a preoperative antiseptic before placement of dermal fillers: an alternative to the standard options. Dermatol Surg. 2018;44:597-9.
- [Google Scholar]
- The interaction between aminoquinolines and presynaptically acting neurotoxins. J Pharmacol Exp Ther. 1982;222:43-8.
- [Google Scholar]
- Influence of isotretinoin on nasal mucociliary clearance and lung function in patients with acne vulgaris. Int J Dermatol. 2010;49:87-90.
- [Google Scholar]
- The safety of laser skin resurfacing with the microablative carbon dioxide laser and review of the literature. J Drugs Dermatol. 2018;17:1157-62.
- [Google Scholar]
- Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020;9:386-9.
- [Google Scholar]
- Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine 2020 [Epub ahead of print] doi 10.1016/j.eclinm.2020.100331
- [Google Scholar]






