Translate this page into:
A Comparative Study between Follicular Unit Transplantation and Autologous Non-cultured Non-trypsinized Epidermal Cells Grafting (Jodhpur Technique) in Stable Vitiligo
Address for correspondence: Dr. Dilip Kachhawa, Department of Skin and V.D., Mathura Das Mathur Hospital, Jodhpur 342003, Rajasthan, India. E-mail: drdilipkachhawa@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Introduction:
Several modalities are currently available for the treatment of vitiligo, but generally they do not result in complete cure of the disease. Despite the limitations and some side effects, surgical modalities appear to be the method of choice in recalcitrant stable vitiligo. Both Jodhpur technique (JT) and follicular unit transplantation (FUT) are simpler and cheaper methods, requiring minimal infrastructure.
Materials and Methods:
Hundred patches in 30 patients were divided into Group A and Group B, that is, hair follicle transplantation and autologous non-cultured non-trypsinized epidermal cell suspension grafting (JT), respectively. Fifty patches were included in each group. Efficacy of both the techniques, extent of pigmentation, and color match assessment were the main objectives.
Results:
Excellent repigmentation (>75%), at the end of 20 weeks post surgery, was observed in 70% lesions in FUT group and 72% of lesions in JT group. Good response (extent of repigmentation of 50%–75%) was seen in 18% of lesions in FUT group as compared to 26% in JT group. JT and FUT technique were almost equal in producing excellent repigmentation. Color match was same for both the groups, that is, 49 of 50 patches showed same color as surrounding in both groups at the end of 20 weeks. Repigmentation of the depigmented hairs occurred in 11 of 46 patients with associated leukotrichia.
Conclusion:
Our study indicates that both JT and FUT are safe and effective techniques in terms of repigmentation but JT is somewhat superior to FUT in producing excellent and good repigmentation, side effects, patient satisfaction, and dermatology life quality index reduction, while the color match was almost same with both techniques.
Keywords
Autologous non-cultured non-trypsinized epidermal cell suspension
hair follicle
transplantation
vitiligo surgery
INTRODUCTION
Vitiligo is a common autoimmune and acquired depigmentation of skin earmarked by well-circumscribed ivory-white asymptomatic macules.[1] Histologically, it is characterized by the absence of melanocytes in the affected area and hair follicles. Vitiligo patches, which are not responding to medical therapy and are stable in nature, are reserved for surgical methods of treatment.[2] Surgical methods work on the principle of transfer of melanocytes from uninvolved skin to the stable vitiligo patch in the form of either tissue graft or cellular graft.
Our study was a randomized study, which was planned to compare the outcome of two surgical modalities. One was “hair follicle unit transplantation”[3] and another was “autologous non-cultured non-trypsinized, epidermal cell grafting (Jodhpur technique)”[4] in patients with stable vitiligo in terms of change in patient’s psychosocial quality of life, extent of repigmentation, color matching of repigmented area, and any adverse events. Follicular unit transplantation (FUT) is tissue graft type of surgical technique that provides a reservoir of undifferentiated stem cells to the depigmented lesional skin. Autologous, non-cultured, non-trypsinized, melanocyte plus keratinocyte grafting is a simple method of melanocyte transfer and does not require special setup.
MATERIALS AND METHODS
Study design
A study of 1-year duration was carried out in 30 patients in the Department of Dermatology, Venereology, and Leprosy, Mathura Das Mathur Hospital, Dr. S.N. Medical College, Jodhpur, Rajasthan, India, by comparing hair follicle transplantation (Group A) and Jodhpur technique (JT) or autologous non-cultured non-trypsinized epidermal cell suspension grafting (Group B) techniques in 100 patches of vitiligo with 50 patches in each group.
Materials required
Dermabrader (manual or electric), straight forceps, electric motor, follicular unit extractor 1 mm punch, jeweler’s forceps were used.
Written informed consent was obtained from the vitiligo patient who participated in the study.
Patients were selected in the study by applying the following inclusion and exclusion criteria
Inclusion criteria
Subjects with clinical diagnosis of focal, segmental, or generalized vitiligo
Stable for more than 1 year
Not responding to medical treatment or residual patches of vitiligo vulgaris after medical therapy
Maximum size of vitiligo patches will be equal or less than 30% of body surface area
Exclusion criteria
Age less than 10 years
Pregnancy and lactation
Patient with actively spreading vitiligo
History of Koebnerization
History of hypertrophic scars or keloidal tendency
Bleeding disorders
Patients with unrealistic expectation
Patients who were immunocompromised
Patients with autoimmune disease such as autoimmune thyroid disease, diabetes mellitus 1, and systemic lupus erythematosus
TECHNIQUE OF TRANSPLANTATION
Harvesting the graft
Follicular unit grafting was done in the vitiliginous lesion, and the hair was transplanted 3–5 mm apart.[34] The donor follicles were extracted using 1-mm biopsy punch (follicular unit extraction [FUE] technique) after giving tumescent anesthesia (lignocaine with 1:100,000 adrenaline diluted in the ratio of 1:10 with normal saline).
Donor area was shaved, cleaned with betadine and surgical spirit, and was anesthetized with a mixture of 2% lignocaine and normal saline (1:1). For non-cultured, non-trypsinized cellular grafting (JT), an antibiotic ointment (2% mupirocin) was applied over the donor site. Dermabrasion was continued till the area appeared whitish (i.e., upper dermis), then the epidermal material entangled in ointment will be collected with the help of spatula or graft spreader. A paste-like material will be obtained. Hemostasis was established, and the area was dressed with Bactigras gauze. Suitable antibiotic and analgesics were prescribed. The three layers of dressing with collagen strips, Bactigras, and elastic plaster (from inside to out, respectively) was done over donor area.
Transplantation procedure
The recipient site was shaved, cleaned with betadine and surgical spirit, and anesthetized with a mixture of 2% lignocaine and normal saline (1:1).
In FUT, the hair follicles were transplanted intact as follicular units. After infiltrative anesthesia at the recipient site, transplantation was done using 18-G needle to create slits in the recipient area, and the hair follicle was gently inserted using a jeweler’s forceps into the created slits.
In JT, dermabrasion was done until tiny pinpoint bleeding spots were seen, which implies that the dermo-epidermal junction has been reached. Dermabrasion was extended 5 mm beyond margins to prevent halo phenomenon. The denuded area was washed with normal saline and covered with normal saline moistened gauze piece. A paste-like ointment containing melanocytes and keratinocytes was spread over recipient site. Dressing was kept in place with the help of osteoplast or bandages. The patient was asked to lie down for 30 min after procedure, and then allowed to go home. The dressing was removed at first follow-up visit after 7 days.
We measure the severity of vitiligo by VIDA (Vitiligo Disease Activity Score) and VASI (Vitiligo Area Scoring Index) scores.
Follow-up
Patients were asked to follow up at the dermatology outpatient department (OPD) at day 8, week 4, 8, 16, and 20, after the transplantation procedure, and repigmentation was assessed subjectively by digital photography. Psoralen and ultraviolet A therapy was given after 3 weeks in both groups.
Extent of repigmentation was assigned as follows:
<25%—Poor repigmentation
25%–50%—Fair repigmentation
50%–75%—Good repigmentation
75%–100%—Excellent repigmentation
Also, the repigmentation pattern was noted as “diffuse,” “perifollicular,” or “dotted,” marginal. A note was also made of the color matching of the repigmented skin as “same as” or “somewhat darker than” normal skin.
After healing with secondary intention, minimal superficial scarring was expected. Scabs usually fall off from the recipient site within 7–14 days, though in many instances there may not be any scab formation.
Follow-ups were done at day 8, then week 4, 8, 16, and 20. Patient assessment was carried out by photography and questionnaire, and it was decided which surgical modality was more efficacious in fulfilling our study criteria.
RESULTS
Table 1 shows of the total 30 patients, 21 were males and 9 were females. Mean duration of disease was 9.26 ± 5.10 years with 4.08 ± 2.67 years of disease stability.
| Characteristics | |
|---|---|
| No. of patients | 30 |
| Gender (male:female) | 21:9 |
| Age in years | 21–25 years |
| Mean duration of disease | 9.26 ± 5.10 years |
| Mean duration of disease stability | 4.08 ± 2.67 years |
| Distribution of lesions (unilateral vs. bilateral) | 11:19 patients |
| Leukotrichia | 20 patients |
Table 2 shows anatomical distribution of vitiligo patches.
| Site of patches | FUT | JT | P value | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Abdomen | 0 | 0.00 | 3 | 6.00 | 0.242 |
| Back | 0 | 0.00 | 4 | 8.00 | 0.117 |
| Breast | 0 | 0.00 | 2 | 4.00 | 1.000 |
| Cheek | 4 | 8.00 | 0 | 0.00 | 0.117 |
| Chest | 8 | 16.00 | 3 | 6.00 | 0.318 |
| Chin | 6 | 12.00 | 0 | 0.00 | 0.026 |
| Eyebrow | 6 | 12.00 | 0 | 0.00 | 0.026 |
| Face | 6 | 12.00 | 0 | 0.00 | 0.026 |
| Finger | 0 | 0.00 | 3 | 6.00 | 0.242 |
| Ankle | 0 | 0.00 | 7 | 14.00 | 0.012 |
| Arm/Forearm | 1 | 2.00 | 11 | 22.00 | 0.003 |
| Foot | 0 | 0.00 | 3 | 6.00 | 0.242 |
| Hand | 0 | 0.00 | 1 | 2.00 | 1.000 |
| Knee | 0 | 0.00 | 2 | 4.00 | 0.494 |
| Leg | 6 | 12.00 | 3 | 6.00 | 0.487 |
| Wrist | 0 | 0.00 | 3 | 6.00 | 0.242 |
| Neck | 7 | 14.00 | 2 | 4.00 | 0.159 |
| Right elbow | 0 | 0.00 | 3 | 6.00 | 0.242 |
| Scalp | 6 | 12.00 | 0 | 0.00 | 0.026 |
The bold fonts signify P < 0.05
At 4 weeks, no patient showed >75% extent of repigmentation in both FUT and JT group; 0%–25% extent of repigmentation was shown by 26 (52%) patches in FUT and 13 (26%) patches in JT with a significant P value (0.013).
However at the end of study, that is, at 20 weeks of follow-up, 35 of 50 (70%) patches in FUT group [Figure 1] and 36 (72%) of 50 patches in JT group [Figure 2] showed >75% extent of repigmentation but the P value was insignificant.
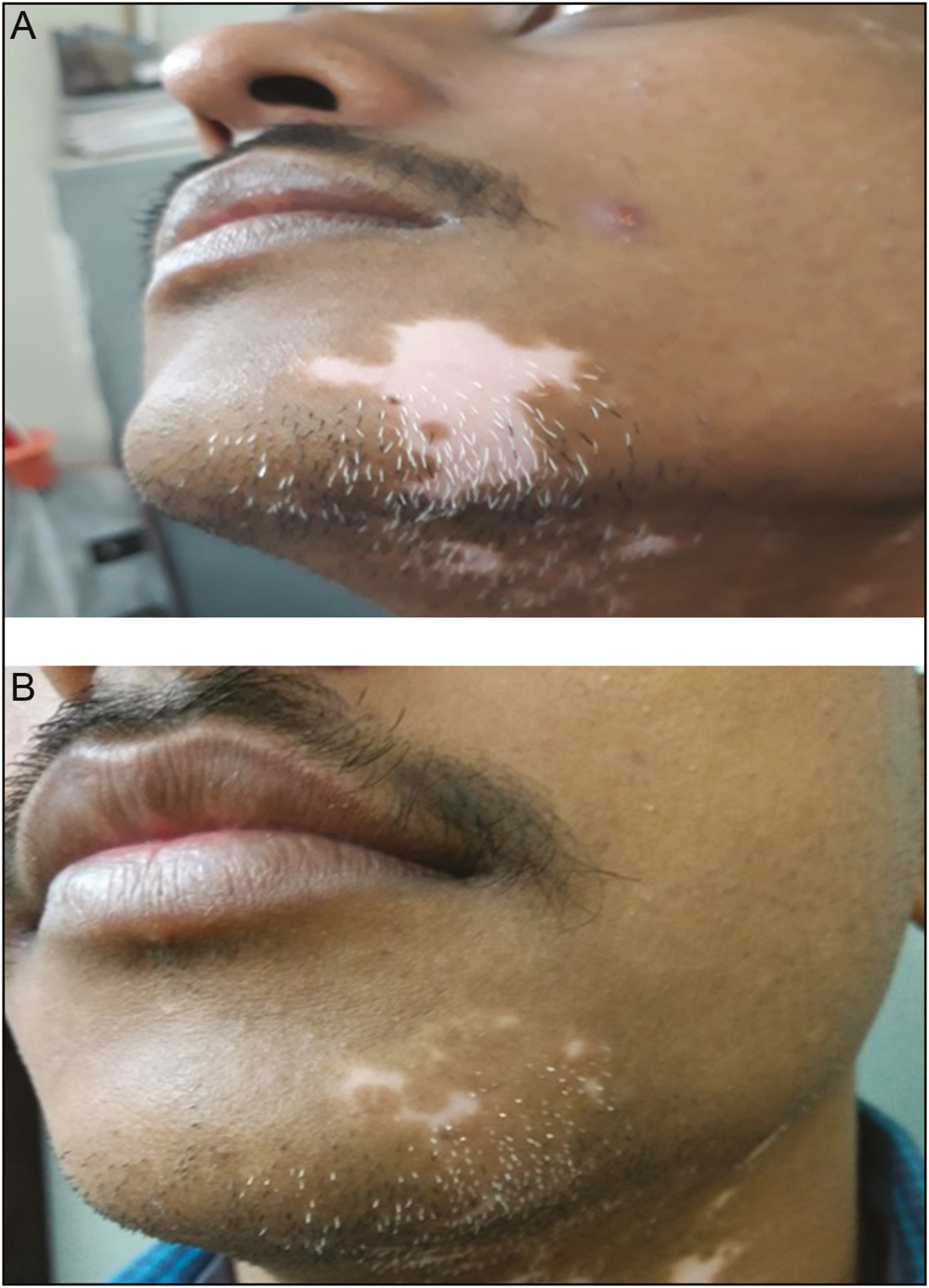
- (A) Vitiligo patch before FUT. (B) Vitiligo patch after FUT at 20 weeks
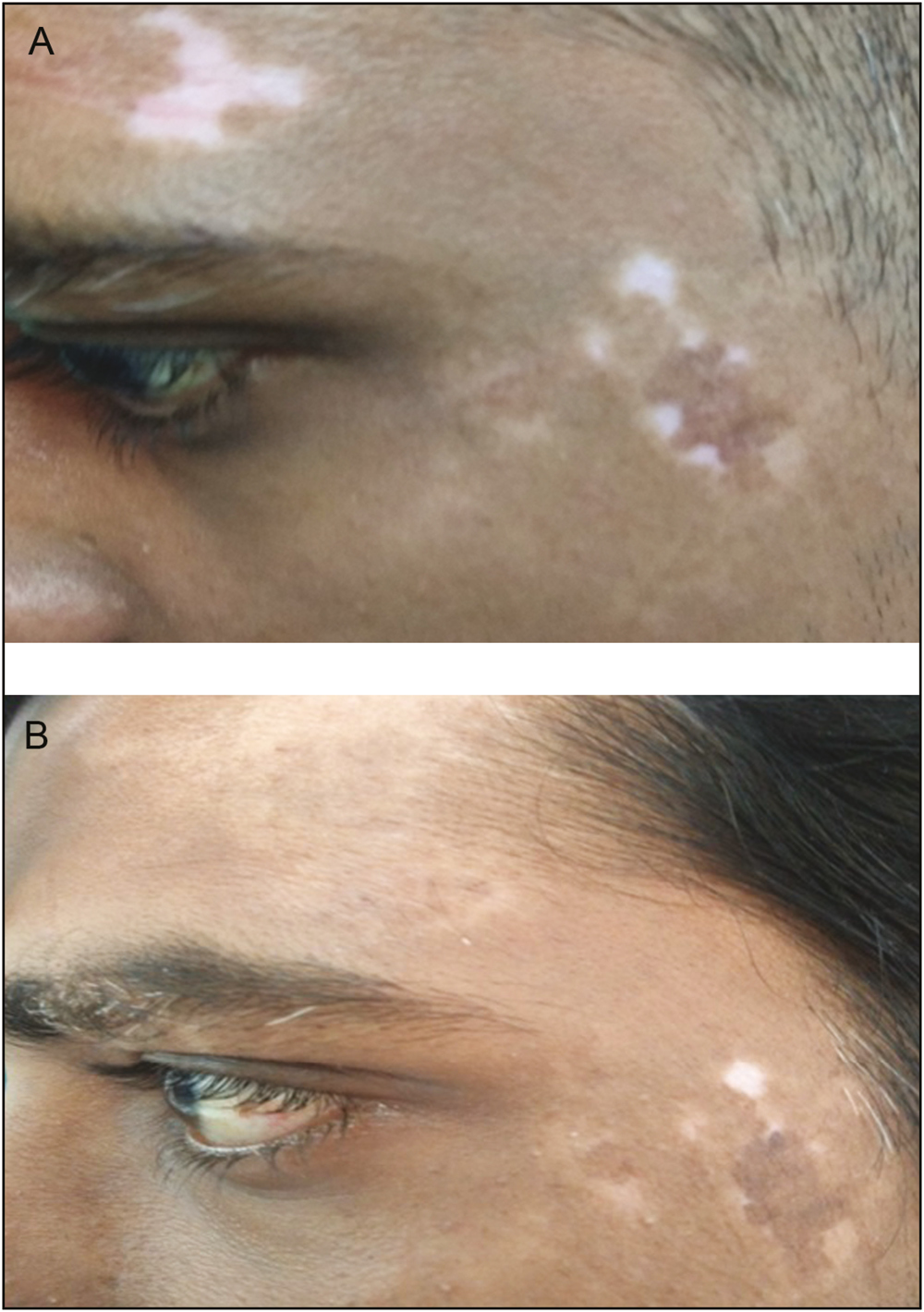
- (A) Vitiligo patch before JT. (B) Vitiligo patch after JT at 20 weeks
In 40 of 50 (80%) lesions in FUT group [Figures 1 and 3] and 34 of 50 (68%) lesions in JT group, the color of the repigmented area matched excellently with the normal surrounding skin. In 10 of 50 (20%) lesions in FUT group and 16 of 50 (32%) lesions in JT group, somewhat darker pigmentation at the end of study but with a tendency to match with normal skin color over passing time at 4 weeks was observed.

- (A) Leukotrichia before FUT. (B) Improvement in leukotrichia after FUT at 20 weeks
The color of the repigmented area matched excellently with the normal surrounding skin at 20 weeks in 49 of 50 (98%) lesions in both groups, One of 50 (2%) lesions in FUT group and JT group [Figure 4] showed somewhat darker pigmentation at the end of study but with a tendency to match with normal skin color over passing time with nonsignificant P value of 1.505.
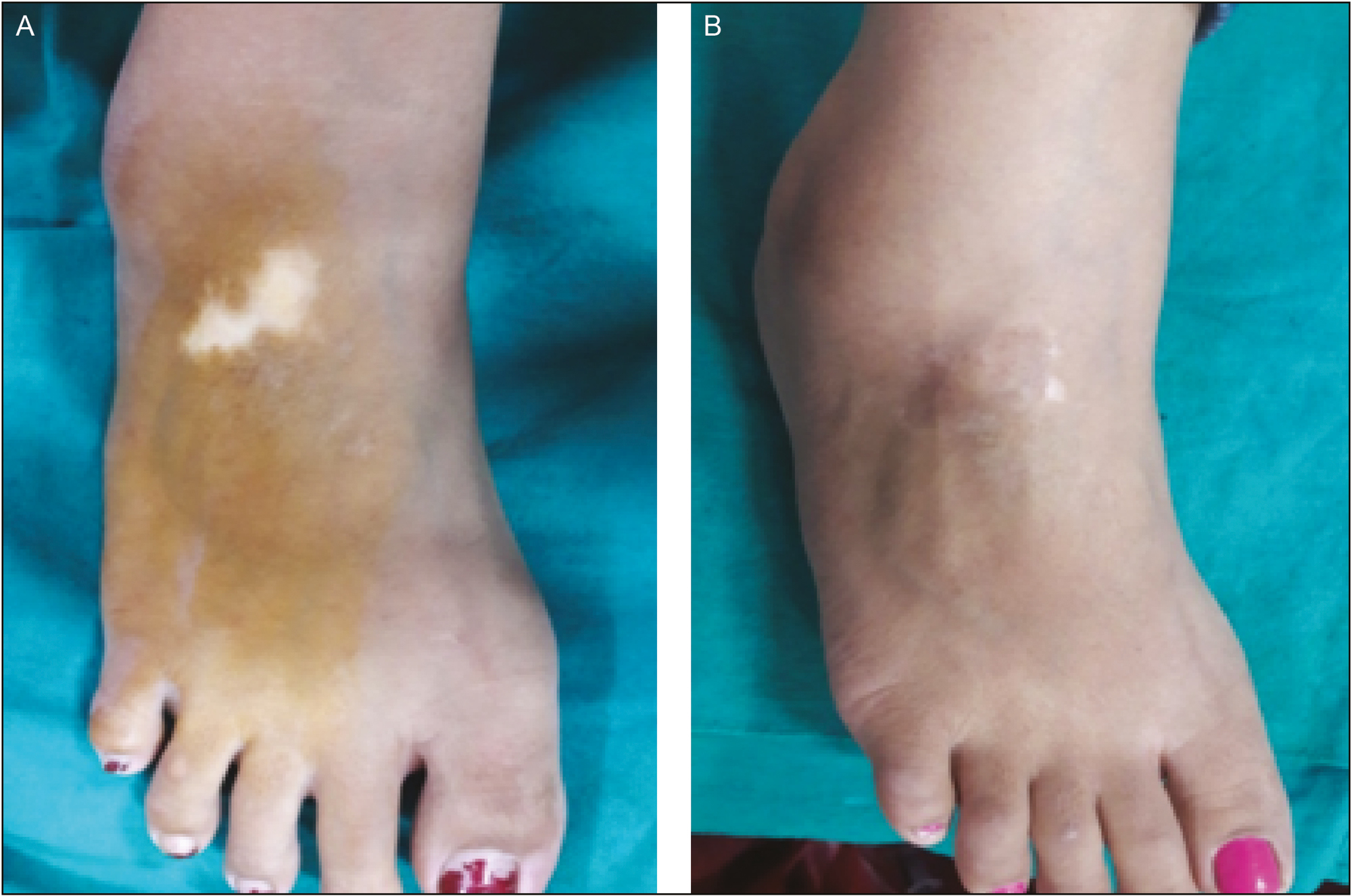
- (A) Vitiligo patch before JT at foot. (B) Vitiligo patch after JT at 20 weeks
While considering time taken for repigmentation, we found that 25%–50% and 50%–75% repigmentation was observed in 27 of 50 (54%) and 8 of 50 (16%) lesions in JT group and in 22 of 50 (44%) and 2 of 50 (4%) lesions in FUT group at 4 weeks, which suggests an earlier onset of repigmentation in JT group.
Patients in both groups were highly satisfied with the treatment outcomes. Patients in which patches treated with JT were more satisfied than patches treated with FUT according to the patient satisfaction questionnaire 1, 2 and 3. Overall PSQ-4 score was 93/7 (in 93 patches, patients want to choose this treatment again as yes and in 7 patches they chosen as no) with 46/4 in FUT group and 47/3 in JT group (P = 1.000).
DISCUSSION
Several modalities are currently available for the treatment of vitiligo, but they generally do not result in complete cure of the disease. Surgical modalities appear to be the method of choice in those stable vitiligo lesions, which do not respond to medical therapies. Both JT and FUT are simpler and cheaper methods, requiring minimal infrastructure, but the surface areas that can be covered using JT, is larger than those, which can be treated with FUT. FUT has an advantage that they permit the treatment of difficult to treat areas.
Follicular unit grafting is based on the transfer of the reservoir of melanocytes, which serve as a source of pigmentation for the depigmented vitiligo lesions. However, it is suitable only for small stable lesions affecting hairy part of body. After grafting, the vitiliginous skin heals slowly with this method because the grafted melanocytes require a long time to spread. Autologous, non-cultured non-trypsinized melanocytes plus keratinocyte grafting (JT) is a simple and new method of melanocytes transfer, which has not been standardized yet and is still in early phase of development.
JT and FUT technique were almost equal in producing excellent repigmentation. However, good extent of repigmentation was obtained more in JT group. This may be because in JT pigmentation, the treated areas gradually increased in size due to melanocyte proliferation and migration under the influence of cytokines secreted by surrounding keratinocytes. We used a very simplified method in vitiligo surgery in JT, as described by Kachhawa and Kallal,[4] who used the epidermal material entangled in ointment obtained by dermabrasion for non-cultured cellular suspension instead of melanocyte media or phosphate buffered saline (PBS). The results of this technique were comparable to the other surgical techniques, including non-cultured melanocyte and keratinocyte transfer. Pandya et al.[5] reported that an excellent response was observed in 52.17% cases with non-cultured epidermal suspension technique and in 50% with the melanocyte culture technique. Gupta et al.[6] developed a scoring system with an original approach, considering the extent of pigmentation, color match, and the complications of both the donor and the recipient area.
Gauthier and Surleve-Bazeille[7] had observed 70% repigmentation in 63.6% of the patients with vitiligo treated by non-cultured melanocyte transplantation. They had included only patients of focal and segmental vitiligo.
While considering time taken for repigmentation, we found that 25%–50% and 50%–75% repigmentation was seen in 27 of 50 and 8 of 50 lesions in JT group and in 22 of 50 and 2 of 50 in FUT group, which suggests an earlier onset of repigmentation in JT group. This is against the hypothesis suggested by Budania et al.,[8] according to which tissue grafts have an early onset of repigmentation as compared to cellular graft. Delayed proliferation of melanocytes and their upward migration from infundibulum to epidermis might explain the delayed onset of pigmentation in FUT technique.
Color match was same for both the groups, that is, 49 of 50 patches showed same color as surrounding in both groups at the end of 20 weeks. The cause of acceptable color match in FUT could be related to the stem cell migration from the graft and then location-specific transient amplifying cell proliferation, and in JT, due to melanocyte proliferation and migration under the effect of cytokines released by keratinocytes.
Perifollicular repigmentation was the most common pattern of repigmentation observed in 49 of overall lesions with 47 (78%) of lesions in FUT group. Diffuse was the most common repigmentation pattern observed in JT group in 34 patches. This signifies that pigmentation in FUT is due to melanocytes from hair follicle itself, and that in JT is due to transplanted melanocytes.
We also carried out patient’s global assessment with the help of a patient satisfaction questionnaire, including three questions—“Grade the change in pigmentation in the transplanted area,” “Are you satisfied with the treatment?,” and “ do you find the treatment worthwhile?” Patients were asked to answer in terms of scoring from 0–10. The scores obtained by this patient satisfaction questionnaire were significantly higher in JT group than those in FUT group. The reasons why patients with JT group were more satisfied that FUT group were because of the exact color match and its ability to treat large areas with minimal complications.
We compared two simplified techniques of vitiligo surgery. Cellular transplantation techniques have been found to be sophisticated, costly, require laboratory and somewhat difficult to be performed at clinic. But we used a very cheaper technique of JT without any melanocyte culture media, trypsin inhibitor, hyaluronic acid, and PBS. We did not use any sophisticated or costly apparatus. We just used simple epidermal material entangled in ointment obtained by dermabrasion.
Our study indicates that both JT and FUT are safe and effective techniques in terms of repigmentation, but JT is somewhat superior to FUT in excellent and good repigmentation, side effects, and patient satisfaction, whereas the color match was almost same with both techniques.
CONCLUSION
This is the first study of this kind to compare a new cellular transplantation technique with an established tissue transplantation technique.
We found that JT was significantly better than FUT in terms of extent of repigmentation. Another benefit of JT described previously in literature is that it can cover larger body surface area with smaller grafts. JT is superior to FUT in difficult to treat areas such as finger, ankle foot, elbow. FUT is time-consuming as compared to JT. It is almost similar to JT in terms of color match. FUT is superior to JT when the lesions present with leukotrichia. Both FUT and JT have the advantage of not leaving any visible scar over the donor area.
Therefore, FUT can be preferred if small, hairy, and cosmetically important area has to be treated, whereas in case of treating large and difficult to treat sites, then JT is preferred.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The definition and assessment of vitiligo: a consensus report of the Vitiligo European Task Force. Pigment Cell Res. 2007;20:27-35.
- [Google Scholar]
- Standard guidelines of care for vitiligo surgery. Indian J Dermatol Venereol Leprol. 2008;74:S37-45.
- [Google Scholar]
- A study of hair follicular transplantation as a treatment option for vitiligo. J Cutan Aesthet Surg. 2015;8:211-7.
- [Google Scholar]
- Keratinocyte-melanocyte graft technique followed by PUVA therapy for stable vitiligo. Indian J Dermatol Venereol Leprol. 2008;74:622-4.
- [Google Scholar]
- A study of autologous melanocyte transfer in treatment of stable vitiligo. Indian J Dermatol Venerol Leprol. 2005;71:393-3.
- [Google Scholar]
- Surgical management of vitiligo and other leukodermas: evidence based practice guidelines. In: Gupta S, Olsson MJ, Kanwar AJ, Ortonne JP, eds. Surgical management of vitiligo (1st ed.). Oxford, UK: Blackwell Publishing; 2007. p. :69-79.
- [Google Scholar]
- Autologous grafting with noncultured melanocytes: a simplified method for treatment of depigmented lesions. J Am Acad Dermatol. 1992;26:191-4.
- [Google Scholar]
- Comparison of two surgical modalities in stable vitiligo: a randomized study. Br J Dermatol. 2012;167:1295-301.
- [Google Scholar]






