Translate this page into:
Propranolol Followed by a Foam Sclerotherapy for Treatment of Tufted Angioma over Neck: A Novel Therapeutic Approach
Address for correspondence: Dr. Manoj Pawar, Flat Number 11, Manomay Apartment, Savata Nagar, CIDCO, Nashik 422008, Maharashtra, India. E-mail: manojpawar624@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Tufted angioma is a rare vascular tumor with cutaneous angiomatous proliferation, commonly localized in the skin and subcutaneous tissues. Most cases are usually acquired in childhood, having protracted course with minimal tendency for spontaneous regression. Various treatment modalities have been described in the literature in the management of tufted angioma with variable response. Thus, there is an urge for simple yet effective and less invasive procedure for tufted angioma, particularly involving aesthetically important areas such as face, head, and neck. We report a case of a large tufted angioma over the neck of a young girl, successfully treated with a combined approach of oral propranolol and foam sclerotherapy.
Keywords
Foam sclerotherapy
propranolol
tufted angioma
INTRODUCTION
Tufted angioma (TA) is a rare vascular tumor with cutaneous angiomatous proliferation, which has protracted course with minimal tendency for spontaneous regression.[12] There is an urge for simple yet effective and less invasive procedure for TA, particularly involving aesthetically important areas such as face, head, and neck.
CASE REPORT
A 20-year-old female presented with asymptomatic dusky red-purple plaques over anterior neck for more than 15 years duration [Figure 1A]. On palpation, no bruit or thrill was present. Skin biopsy confirmed the diagnosis of TA [Figure 1B]. Color Doppler ultrasound and magnetic resonance imaging (MRI) revealed superficial location of TA, without any deep invasion [Figure 2]. After routine laboratory investigations and electrocardiogram (ECG), which did not reveal any abnormality, we started her on oral propranolol therapy initially with 1 mg/kg/day, and later escalated to and maintained on 2 mg/kg/day after 2 weeks. There was a significant improvement of the lesions after 3 months, but the regression was incomplete and static at the end of 6 months [Figure 1C]. As the patient could not afford laser therapy, we decided to try foam sclerotherapy with sodium tetradecyl sulfate (STS). Preprocedural consent, counseling, topical eutectic mixture of local anesthetic (EMLA) cream application, and local antiseptic measures were carried out before the procedure. An intradermal test dose of STS was administered to rule out allergy. A total of 1 mL of 3% STS (diluted 1:4 in normal saline) was loaded in a 5-cc syringe and connected to another 5-cc syringe (having 4-cc room air) through a three-way stopcock. STS was pumped to-and-fro into the connected syringe, and this process was repeated several times until whitish frothy foam was formed, and it was injected slowly into each lesion (0.05–0.1 mL). Blanching of the lesion was considered as the end point. This procedure was repeated every 3 week for five sessions. Local antisepsis and oral antibiotic and anti-inflammatory drugs were started for the next 5 days. Mild transient erythema, edema, and discomfort were the immediate postoperative complications [Figure 3A]. Few lesions showed crusting, which later healed without any sequelae. After first two sittings, there was a slight regression of most lesions, and at the end of fifth sitting, most of the lesions nearly flattened with slight residual pigmentation [Figure 3B]. There was no recurrence at 6 months of follow-up.
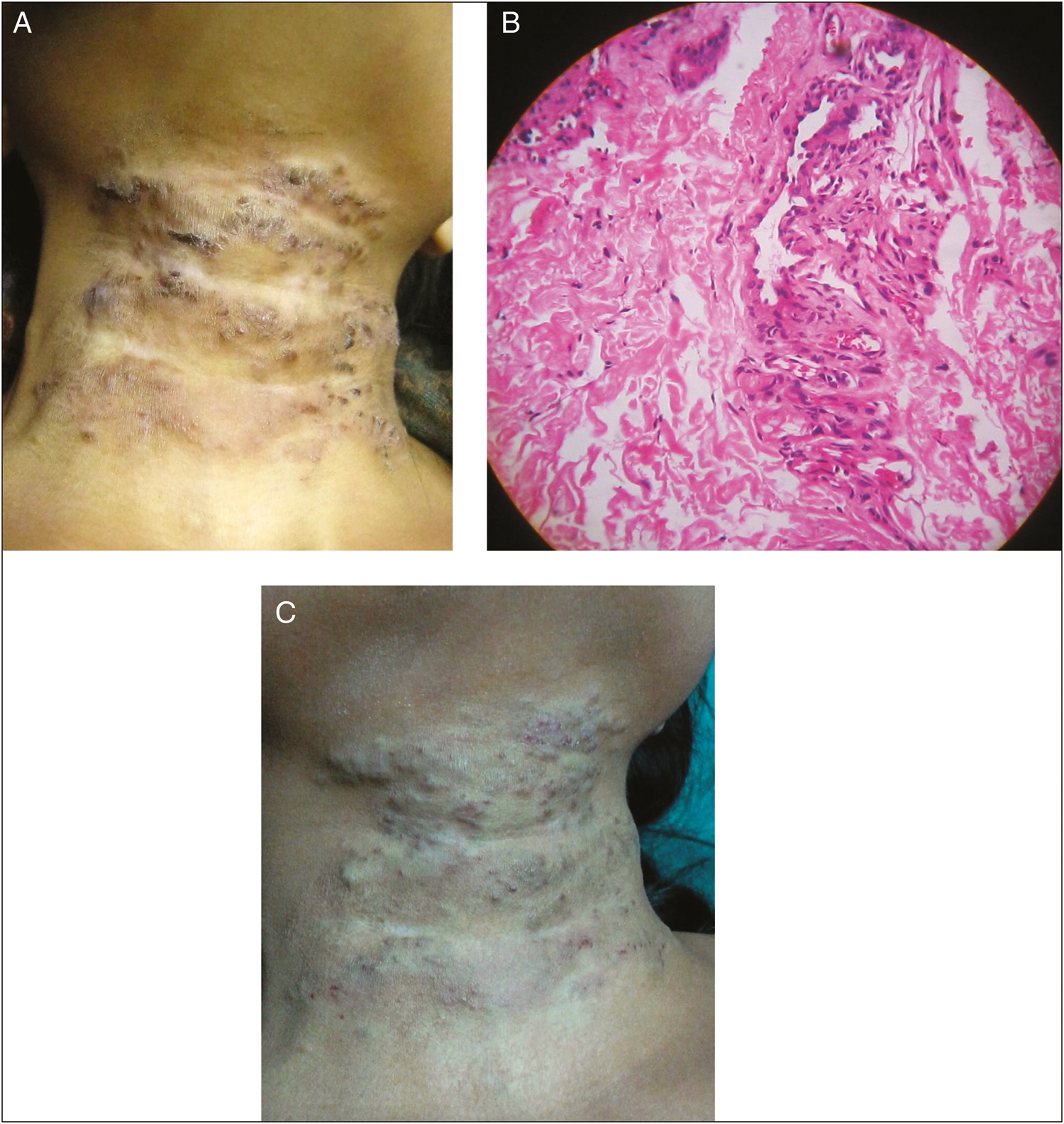
- Tufted angioma over neck before treatment (A), skin biopsy showing clusters of numerous dilated capillaries, which are lined by plump and elongated endothelial cells in the dermis (original magnification ×100, hematoxylin and eosin stain) (B), six months after propranolol therapy significant flattening of the lesions (C)
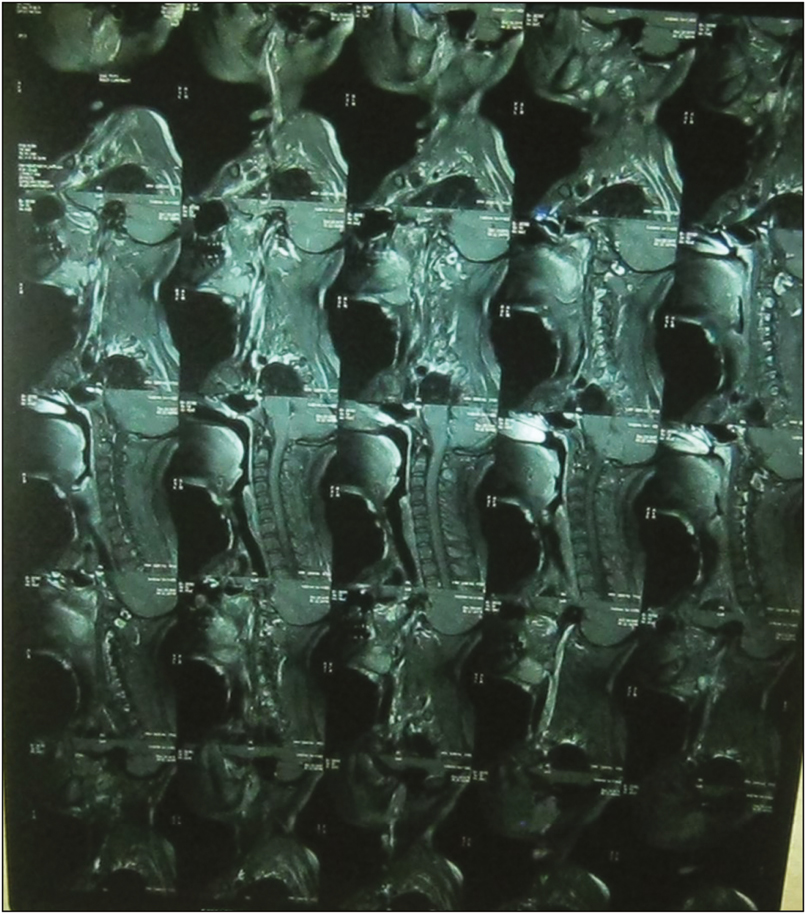
- MRI of the neck showing subcutaneous ill-defined lesion in the anterior triangle of neck suggestive of superficial hemangioma
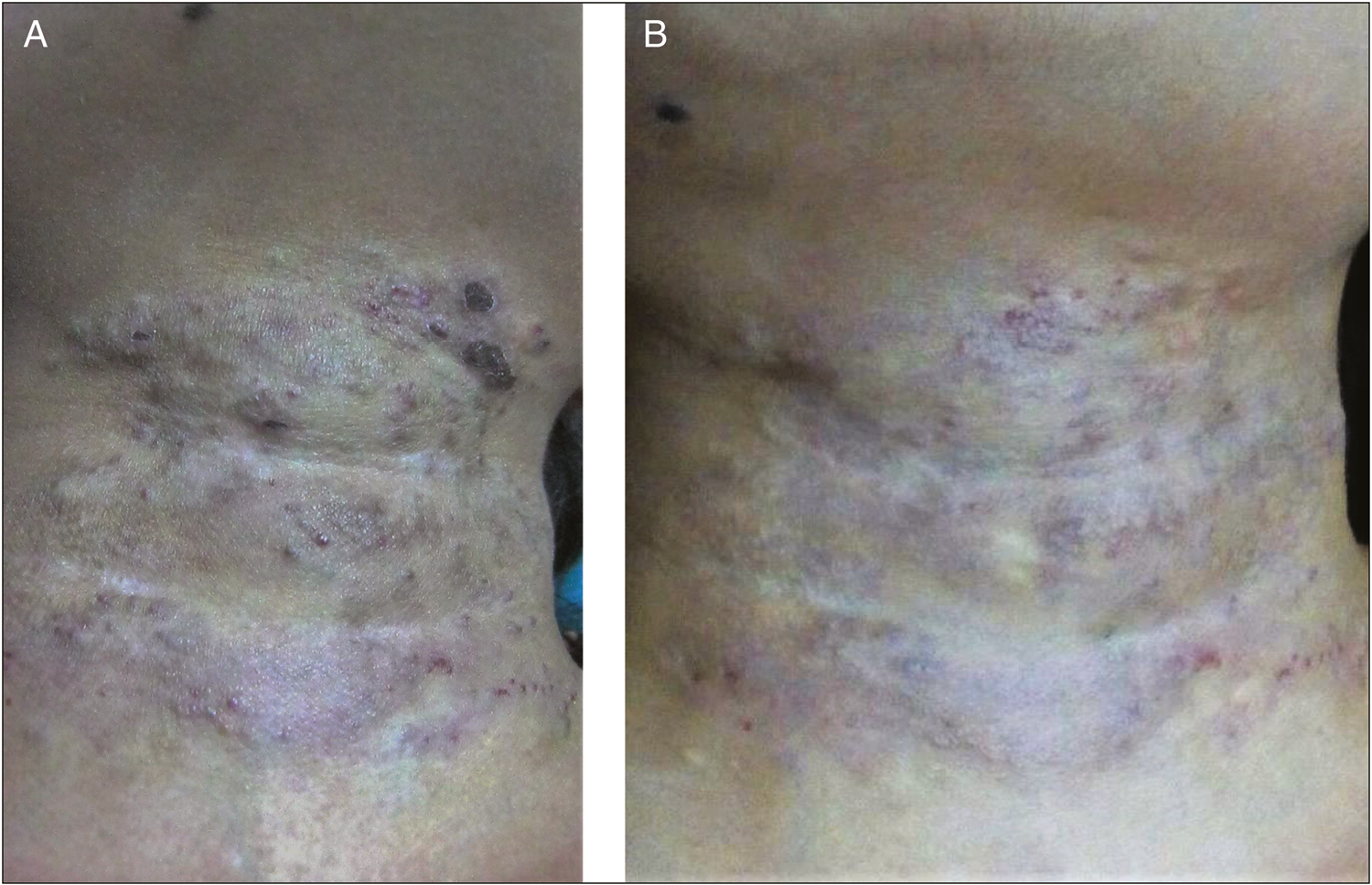
- Few crusts formed after few days of the foam sclerotherapy (A), near-complete resolution of lesions with residual pigmentation after the five sessions of foam sclerotherapy (B)
DISCUSSION
Systemic or intralesional corticosteroids, low doses of acetylsalicylic acid, interferon-α, radiotherapy, chemotherapy with vincristine, pulsed dye laser, and oral propranolol have been described in the literature in the management of TA with variable response.[3] Various significant side effects limit the use of steroids and vincristine in TA, whereas radiotherapy and laser therapy may not be feasible for every patient. We thought of adding sclerotherapy in this patient because of its low cost, simple, easy, and pain-free application and yet effective with minimal adverse events, based on our previous experiences (unpublished).
STS is a sclerosant composed of sodium 1-isobutyl-4-ethyloctyl sulfate, benzoyl alcohol, and phosphate, which disrupts the intercellular cement between the endothelial cells, resulting in the desquamation of the cells in plaques. It also leads to thrombus formation inside the vessel, leading to endovascular obliteration.[4] The reason behind using STS in a foam form over liquid form is that foam displaces the blood and distributes more evenly over the endothelium, causing increased surface area, and thus allowing larger lesions to be treated.[5] Propranolol is a beta-blocker successfully used for various benign vascular tumors, because of its actions such as decreased expression of vascular endothelial growth factor (VEGF), basic fibroblast growth factor (bFGF), and matrix metalloproteinase (MMP), and induction of apoptosis in capillary endothelial cells.[6]
Thus, we believe that an approach of oral propranolol followed by foam sclerotherpy may be useful in patients with recalcitrant TA.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Tufted angioma associated with Kasabach-Merritt phenomenon: a therapeutic challenge. Acta Derm Venereol. 2010;90:535-7.
- [Google Scholar]
- Clinical spectrum of tufted angiomas in childhood: a report of 13 cases and a review of the literature. Arch Dermatol. 2010;146:758-63.
- [Google Scholar]
- Utility of sodium tetradecyl sulfate sclerotherapy from benign oral vascular lesion. Maxillofac Plast Reconstr Surg. 2016;38:44.
- [Google Scholar]
- The use of foam sclerotherapy to treat low-flow vascular malformations of the head and neck. J Surg Case Rep. 2014;2014:rju095.
- [Google Scholar]
- Successful treatment of tufted angioma with propranolol. J Dermatol. 2014;41:1120-2.
- [Google Scholar]






