Translate this page into:
Dermatoses Occurring after Parlor Procedures
Address for correspondence: Dr. Sravanthi Kotha, Department of DVL, GSL Medical College, Rajahmahendravaram 533296, Andhra Pradesh, India. E-mail: dvlgsl20@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Cosmetic procedures are on the rise and practiced by all age groups, especially by teenagers. These procedures enhance the individual appearance and confidence levels, but they are not without side effects.
Aims and Objectives:
The aim of this study was to evaluate the side effects occurring after various parlor procedures such as facials, threading, waxing, and laser hair reduction.
Setting and Design:
A prospective study for 12 months in a tertiary hospital.
Materials and Methods:
Patients attending the department of dermatology at a tertiary care hospital for 12 months (July 2018–June 2019) were evaluated for any skin lesions, developed after one of the above parlor procedures. Detailed history, clinical examination, and correlation with the parlor procedure were noted.
Results:
A total of 102 patients were found to have dermatoses after various parlor procedures during the 1-year study period (81 F and 21 M). Acneiform eruptions 26 (25.4%), followed by post-waxing folliculitis 17(16.7%), and hyperpigmentation of face 15 (14.7%) were the most common dermatoses. Molluscum contagiosum, verrucae plana, and tinea faciei were observed in 11, 6, and 3 patients, respectively.
Conclusion:
Side effects are not uncommon after parlor procedures. Awareness of these is necessary and educating the patients is extremely important to avoid these unwanted complications.
Keywords
Dermatoses
facials
parlor procedures
threading
waxing
INTRODUCTION
Cosmetic procedures are frequently practiced by all age groups of people, especially by teenagers. Increased awareness, beauty consciousness, increased living standards, and life-style modification are leading to more cosmetic practices. A lot of dermatoses arise due to these parlor procedures; thus, it is very important to know about them, and to be cautious.[12]
SUBJECTS AND METHODS
Patients attending the department of dermatology at a tertiary care hospital for 12 months (July 2018 to June 2019) were evaluated for any skin lesions, developed after parlor procedures, such as facials, threading, waxing, and laser hair reductions. Though laser hair reduction is not a parlor procedure, it was included here because hair reduction was done in many parlors and we observed few people developing one or other complications after that. Patients, developed dermatoses within 8 weeks following a parlor procedure were included in the study. Institutional ethical committee approval was obtained. Detailed history, clinical examination, and correlation with parlor procedure were noted. The site of involvement, morphology of lesions, and association with the procedure done in the parlor were recorded.
RESULTS
One hundred and two patients were found to have dermatoses after parlor procedures during the one year study period. Eighty one were females and 21 were males. The age-wise distribution is shown in Table 1. Sixty one (59.8%) were in the age group 21–40 years. The mean duration after which the lesions developed was found to be 2.3 weeks after the parlor procedure. The details of dermatoses occurred, after the parlor procedures are shown in Table 2.
| Age | Number | Percentage (%) |
|---|---|---|
| 10–20 | 11 | 10.8 |
| 21–30 | 35 | 34.3 |
| 31–40 | 26 | 25.5 |
| 41–50 | 16 | 15.7 |
| >50 | 14 | 13.7 |
| Females (total 81) | Males (21) | ||
|---|---|---|---|
| Acneiform eruptions | 18 | Acneiform eruptions | 8 |
| Exacerbation of acne | 12 | Exacerbation of acne | 4 |
| Waxing folliculitis | 17 | Folliculitis | 1 |
| Hyperpigmentation | 11 | Hyperpigmentation | 4 |
| Contact dermatitis | 8 | Contact dermatitis | 1 |
| Molluscum contagiosum | 8 | Molluscum contagiosum | 3 |
| Verrucae | 6 | ||
| Tinea faciei | 3 |
Acneiform eruptions 26 (25.4%), or exacerbation of existing acne 16 (15.7%) were the most common presenting dermatoses, followed by post-waxing folliculitis and hyperpigmentation of face. Acneiform eruptions were seen with gold facial (12), herbal (8), and 3 each with de-tan facial and fruit facial. Facial hyperpigmentation was seen in 15 (11 F and 4 M) and developed as early as within 7 days of the parlor procedure, the longest presentation being after 3 weeks. Three patients developed hyperpigmented patches over upper lip and chin after laser hair reduction [Figure 1]. Folliculitis after waxing developed in 17 women. Thirteen of them had waxing only on the upper limbs, both forearms and arms and 4 had waxing on both upper and lower limbs. Folliculitis was more severe on upper limbs than legs. Lesions were predominantly follicular papules, sometimes surmounted by pustules.

- Hyperpigmentation occurring after laser hair reduction
Nine patients developed contact dermatitis, and it was due to hair dye in 6 and to creams given by the parlor in 3 [Figure 2]. Patch test was done with the respective cosmetics, patients have brought and all of them showed patch test positivity to the respective allergens. Molluscum contagiosum, verrucae, and tinea faciei were seen in 8, 6, and 3 female patients, respectively, on eye brows after threading [Figure 3].

- Contact dermatitis to postfacial cream given in parlor
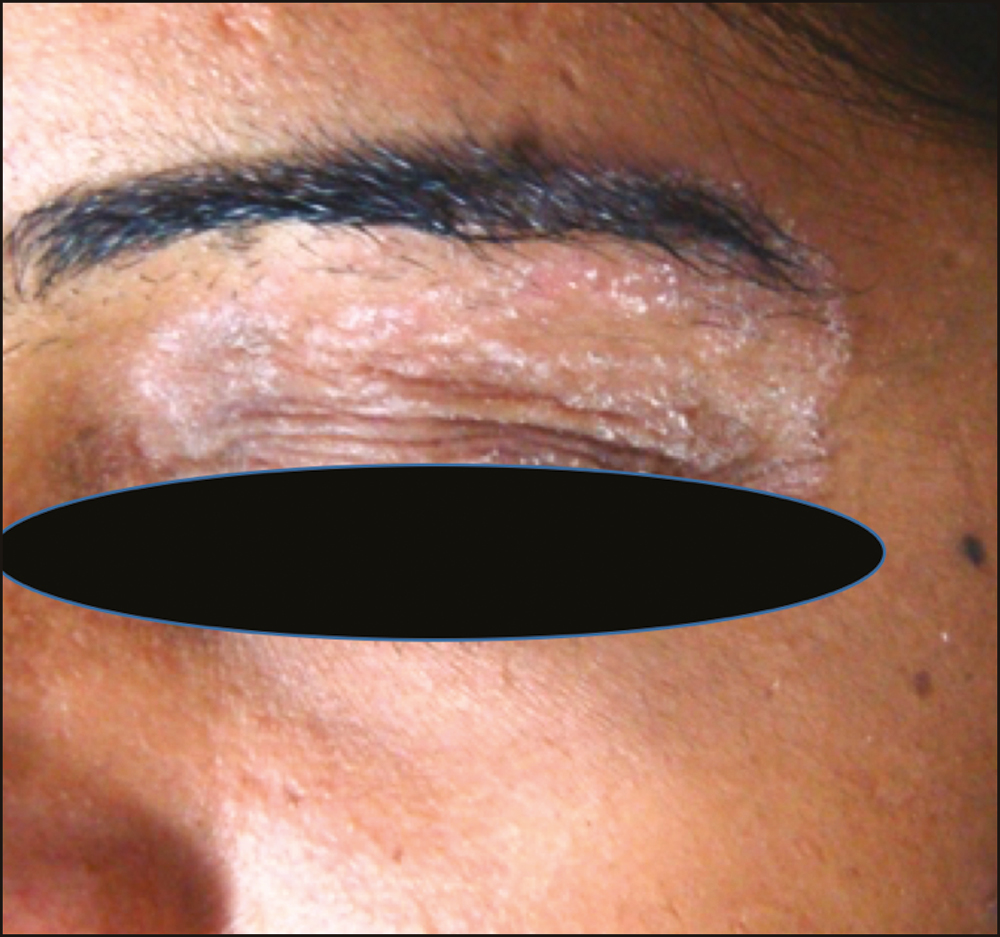
- Tinea faciei on left eye brow after threading
DISCUSSION
Parlor procedures are increasing and so the adverse effects. Facials, threading of eye brows, waxing of hair on body, and hair dyeing are some of the commonly practiced parlor procedures. Over a period of 1 year 102 patients presented with different adverse effects after parlor activity [Table 2]. Gupta and Thappa[3] had brought out the dermatoses occurring after various Indian cultural practices, such as contact dermatitis to henna, bindi stickers, alta, and follicular keratotic papules over pinna and nape of neck after modichood. Warts, molluscum, and vitiligo were reported after threading.[456]
Acneiform eruptions were seen in 26 (25.4%) and acne was exacerbated in 16 (15.7%) in this study. George and Sridharan.[7] reported exacerbation of acne in 40% of their series after cosmetic use. Facials also can induce or exacerbate acne. Khanna and Gupta[1] had reported acneiform eruptions in 33.1% of participants after facials. In our study 26 developed acneiform eruptions, 12 with gold facial, 8 with herbal, 3 each with de-tan facial and fruit facial. George and Sridharan[7] noted acne exacerbation in 14.5% of their study and we observed in 15.7%. The lesions were mild to moderate, consisting of comedones, papules, and/or few pustules. Five patients had itching, but the potassium hydroxide (KOH) smears did not reveal any Pityrosporum ovale or Demodex. Acneiform eruptions generally develop 2–4 weeks after facials, but it can occur as long as 10 weeks later also. Nine (37.5%) developed after the first facial and the rest developed each time they undergo facial. Khanna et al.[1] have reported 27.7% after first facial and 72.3% after every facial. The vigorous massage practiced during the procedure could cause obstruction or breakage of pilosebaceous duct and the inflammatory response.
People are overly conscious about body hair and use waxing to remove cosmetically unacceptable hair, especially if large areas are to be treated. Waxing could be either hot waxing or cold waxing. Though waxing was done more in females, Richards et al.[8] reported that 3.3% males in their study used waxing for hair removal. In our study 17 (16.7%) cases developed folliculitis after hot waxing and all were females. Follicular and nonfollicular pustules were seen in the waxed area. Arms and thighs were more involved than the forearms and legs. Two of them had itching and others were asymptomatic. Khanna et al.[9] reported follicular papules in all 28 cases they studied, nonfollicular in 50% of the cases, with foreign body granulomas or periappendageal and perivascular inflammatory infiltrate, mainly of neutrophils, suggesting pseudofolliculitis. Nodules were uncommon, but Amado et al.[10] reported painful nodules as a part of post-waxing Pseudomonas folliculitis. Nodules were not seen in our group.
Facial hyperpigmentation, seen in 15 (14.7%), occurred mainly after gold facial, which contains aloe vera, sandalwood, turmeric, gold Oxide, xantham gum, dimethicone, and triclosan. Some preparations add extracts of Galnut, wheatgerm and rose petals. Though the exact cause and mechanism of this hyperpigmentation is not clear, the sandalwood is known to cause photoallergy and it could have been caused the hyperpigmentation in these cases.[1112] Three females developed patchy hyperpigmentation on lips after laser reduction of hair. The laser used was Diode 800 and the parameters were not known. Hyperpigmentation developed after second sitting in all 3 cases from the same parlor. Laser hair reduction may cause, burning, erythema, purpura, scarring, and pigmentary changes.[13] Hyperpigmentation can occur after laser hair reduction as a post-inflammatory change, which may be caused by high fluence, short pulse duration, and insufficient cooling. It may take longer time to disappear and it took 18–24 months in our patients.
Contact dermatitis presenting as erythema, scaling, itching was observed in 9 cases, 8 female, and 1 male (8.8%). Three of them developed after the creams supplied by parlor, where the contents were not known and 6 developed to hair dye. Patch test was done with the materials used by the patients and paraphenylenediamine (PPD) in hair dye patients and all of them were positive to respective allergens. After hair dye the lesions were more concentrated around the hair margins and one developed edema of the forehead and periorbital area. All 6 patients with hair dye dermatitis showed positivity to PPD. Contact dermatitis to PPD has risen fourfold with a prevalence of 2%–12% in Asia.[14] It can occur in users as well as in hair dressers. All six in our group were users only. Contact depigmentation can occur with PPD and Ghosh and Mukhopadhyay[15] reported dye depigmentation in 27.4% of their 864 cases with chemical leukoderma. Five females in the present group did not develop contact depigmentation, but the one male had it on scalp, frontal area and moustache area.
The eyebrow shaping by threading is a common beauty parlor procedure practiced to enhance the aesthetic appeal and to get rid of unwanted hair. The common side effects of threading include erythema, folliculitis, pseudofolliculitis, bullous impetigo, verruca plana, molluscum, and secondary pigmentary changes.[5] In our study we encountered 8 (7.8%) molluscum contagiosum, 6(5.9%) verrucae, and 3 (2.9%) tinea faciei after threading of eye brows. Molluscum contagiosum and verrucae were reported after threading.[24,616] Tinea faciei developed on the eye brows after threading is uncommon. We noticed in three patients on the eye brows, developed after 3–4 weeks after threading. They did not have tinea at any other sites and denied of having it in any other family members. All of them showed hyphae on KOH smear and culture had grown Trichophyton mentagrophytes. All these viral and fungal infections after the threading could be because of improper sterilization procedures and reusing of threads at parlors.
CONCLUSION
Parlor procedures may enhance the beauty but one should be aware of the not uncommon side effects that follow these procedures. Educating the patients is extremely important to avoid unwanted complications or side effects after these procedures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Eyebrow threading: a popular hair-removal procedure and its seldom-discussed complications. Clin Exp Dermatol. 2009;34:363-5.
- [Google Scholar]
- Vitiligo koebnerised by eyebrow plucking by threading. J Cosmetic Dermatol. 2002;1:214-5.
- [Google Scholar]
- Threading warts: a beauty parlor dermatosis. J Cosmetic Dermatology. 2007;6:279-82.
- [Google Scholar]
- Factors aggravating or precipitating acne in Indian adults: a hospital-based study of 110 cases. Indian J Dermatol. 2018;63:328-31.
- [Google Scholar]
- Temporary hair removal in patients with hirsutism: a clinical study. Cutis. 1990;45:199-202.
- [Google Scholar]
- Post waxing folliculitis: a clinicopathological evaluation. Int J Dermatol. 2014;53:849-54.
- [Google Scholar]
- Folliculitis caused by pseudomonas aeruginosa after hair removal with wax. Rev Clin Esp. 1992;190:103-4.
- [Google Scholar]
- Complications of nonphysician-supervised laser hair removal: case report and literature review. Can Fam Physician. 2009;55:50-2.
- [Google Scholar]
- Contact dermatitis to hair dye: an update. Indian J Dermatol Venereol Leprol. 2012;78:583-90.
- [Google Scholar]
- Chemical leucoderma: a clinico-aetiological study of 864 cases in the perspective of a developing country. Br J Dermatol. 2009;160:40-7.
- [Google Scholar]
- Molluscum contagiosum after eyebrow shaping: a beauty salon hazard. Clin Exp Dermatol. 2009;34:e339-40.
- [Google Scholar]






