Translate this page into:
Papillary Eccrine Adenoma in a 5-year-old Girl Altered by Application of Thuja Ointment
Address for correspondence: Dr. Betsy Ambooken, Additional Professor, Department of Dermatology & Venereology Govt. Medical College, Thrissur, Kerala. Pin: 680596. E-mail: joebetsy123@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Papillary eccrine adenoma (PEA) usually presents in adults on the extremities. We report an unusual presentation of PEA in a child who was initially misdiagnosed and treated with Thuja ointment that led to the peripheral extension of the lesion.
A 5-year-old girl presented with an asymptomatic solitary nodule on the face just lateral to the right eyebrow of 6-month duration. On examination, there was a well-circumscribed globoid pink nodule of size 0.75 cm diameter with an irregular surface [Figure 1A]. She was advised excision biopsy of the lesion considering the possibilities of benign appendageal tumor or spitz nevus. Her parents were worried about the scar that could result with excision of the lesion. Hence, they resorted to homeopathic treatment and were advised an ointment named Thuja, which contains the botanical agent Thuja occidentalis. After 6 months, child was brought again with peripheral extension of the lesion. On examination there was an annular plaque of size 2 cm × 2 cm with a slightly depressed center and periphery studded with milia-like papules [Figure 1B]. A complete excision was done which however resulted in an irregular scar greater in size than the initial tumor. As the lesion was on the face and clinically appeared benign, excision was done close to the edge of the lesion. We followed up the patient for 1 year with no signs of recurrence.
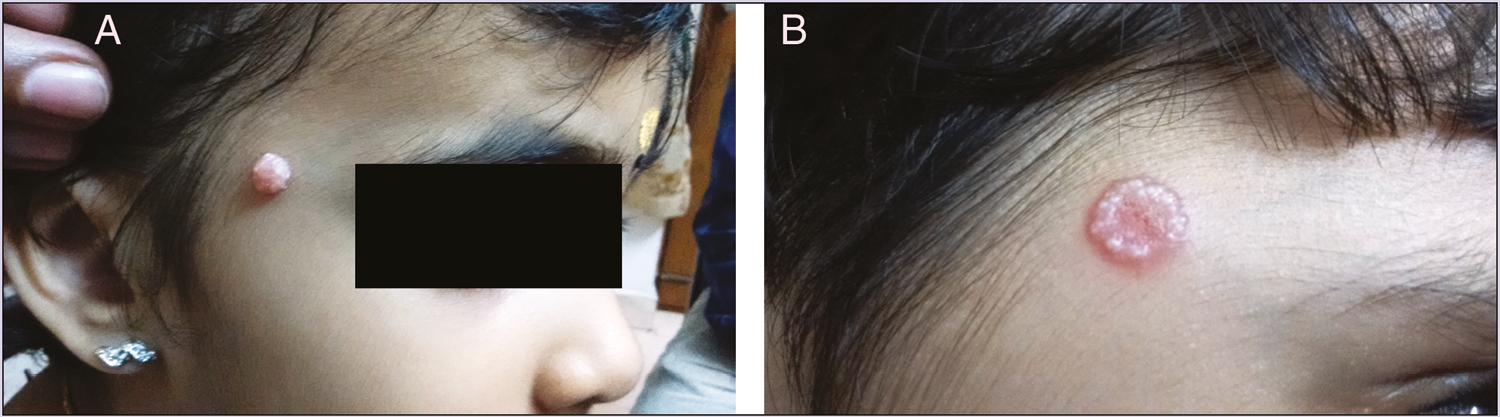
- (A) A well-circumscribed globoid pink nodule of size 0.75 cm diameter with an irregular surface. (B) An annular plaque of 2 cm x 2 cm with a slightly depressed centre and periphery studded with milia-like papules
The excision biopsy was initially reported as syringoma. As clinically it was not suggestive of syringoma, we reviewed the slide. Mid and lower dermis showed multiple dilated ducts of varying size. Few horn cysts were also seen in the upper dermis [Figure 2A]. The ducts were lined with double layer of cuboidal cells with intraluminal papillary extensions [Figure 2B]. Lining cells did not show any features of atypia. Lumen of most of the ducts were filled with eosinophilic amorphous material. Luminal cells did not show any decapitation secretion. There was dense collection of inflammatory cells surrounding the ducts. Immunohistochemistry was not done for confirming the eccrine origin of the tumor due to financial constraints. However, the absence of columnar cells showing decapitation secretion lining the lumen of ducts favored an eccrine origin. The cuboidal cells lining the dilated ducts together with intraluminal papillary extensions confirmed the diagnosis of PEA.
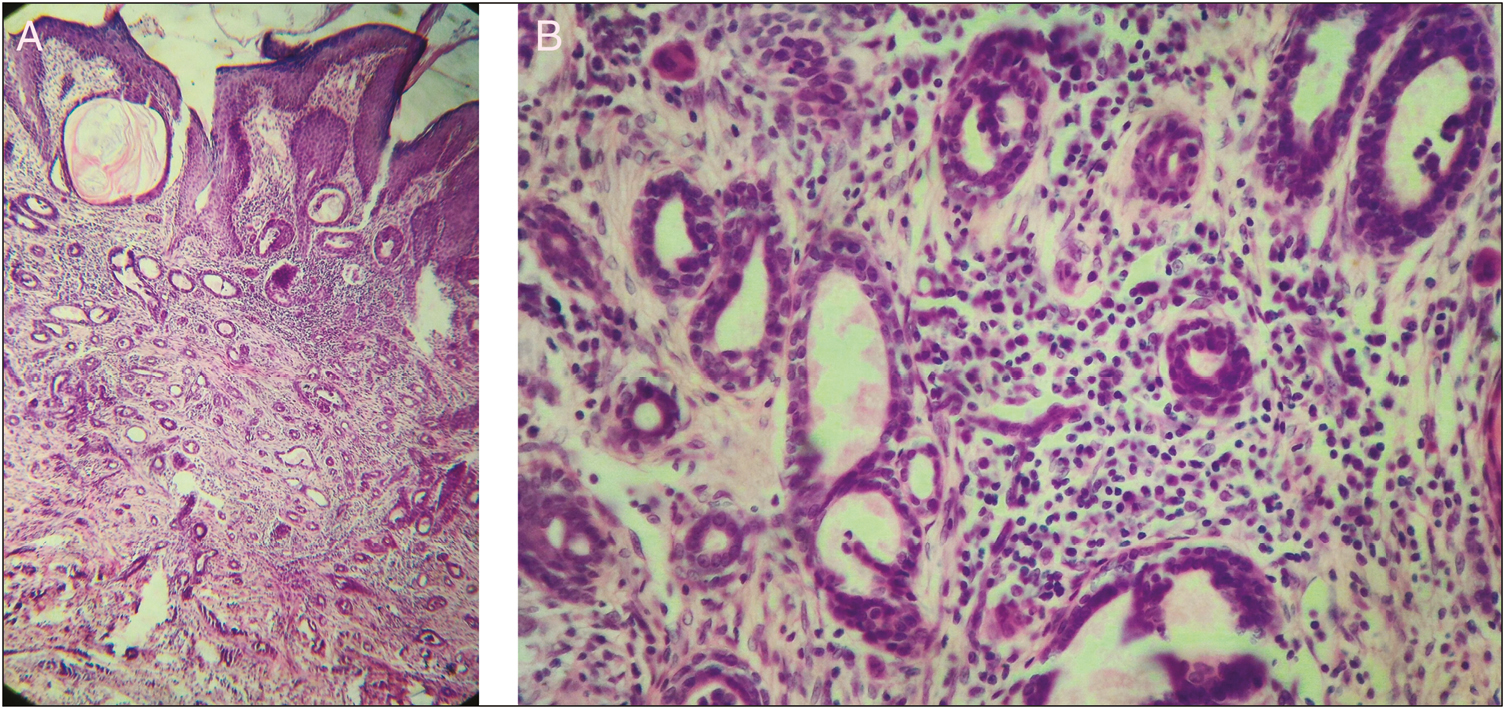
- (A) Multiple dilated ducts of varying sizes, lined by double layer of cuboidal cells located mostly in the mid and lower dermis. Few horn cysts seen in the upper dermis. H and E stain10 x 10X. (B) The ducts are lined with double layer of cuboidal cells with intraluminal papillary extensions. Lumen of most of the ducts show eosinophilic amorphous material. H and E stain 40 x 10X
PEA is a rare benign appendageal tumor involving eccrine sweat glands. It was first described by Rulon and Helwig.[1] It presents in a nondiagnostic manner as slow-growing well-circumscribed solitary nodule on the limbs of dark-skinned middle-aged females.[2] The histological differentials include tubular apocrine adenoma (TAA), basal cell carcinoma (BCC) of eccrine differentiation, and adenocarcinomas.[3] The absence of decapitation secretion of the luminal cells helped in differentiating it from TAA. Absence of dysplastic changes differentiated it from malignant tumors. Immunohistochemistry is helpful to confirm the diagnosis. A positive S-100 protein, carcinoembryonic antigen (CEA), and epithelial membrane antigen (EMA) usually favor differentiation toward secretory epithelium of the sweat glands. Markers such as actin (alpha-SMA), keratin 8, and keratin 14 are more reliable in suggesting an eccrine origin of the tumor.[4]
Thuja occidentalis, commonly known as arbor vitae or white cedar, is indigenous to eastern North America and is grown in Europe as an ornamental tree. The main component Thujone is mainly a neurotoxin and a skin irritant. Thuja is believed to upregulate interleukins and tumor necrosis factor and is used by homeopathic doctors and practitioners of Chinese medicine for the treatment of warts and molluscum contagiosum and several systemic disorders. It is neither FDA approved nor approved for the use in children and pregnant women.[5] In our case, the application of Thuja to the lesion had resulted in central necrosis and peripheral extension of the lesion.
There have been very few reports of PEA in children. In the recent review of 48 cases reported till 2016, there were only 4 childhood cases and all of them had lesion on the extremities.[4] In clinically atypical cases or when there exists a doubt in the diagnosis, blindly resorting to self destructive modalities such as electrosurgery, chemical cautery, or cryotherapy can be detrimental. Our case also highlights the need for developing good counseling skills as a fairly good number of our patients resort to alternative medicine and come late in the course of the disease. The current treatment of choice involves early complete surgical excision of the neoplasm, and confirmation of clear margins of the tissue to prevent recurrence.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Papillary eccrine adenoma. A tubulopapillary hidradenoma with eccrine differentiation. Am J Dermatopathol. 1986;8:64-72.
- [Google Scholar]
- Papillary Eccrine Adenoma: A Recent Review of Literature. Am J Med Case Rep. 2016;4:304-9.
- [Google Scholar]
- Thuja occidentalis (arbor vitae): A review of its pharmaceutical, pharmacological and clinical properties. Evid Based Complement Alternat Med. 2005;2:69-78.
- [Google Scholar]





