Translate this page into:
Comparative Evaluation of Efficacy of Non-cultured Epidermal Cell Suspension and Epidermal Curettage in Stable Vitiligo
Address for correspondence: Dr. Suresh Kumar Malhotra, H. No. 943, Sector 3, Housing Board Colony, Amritsar 143001, Punjab, India. E-mail: dskm50@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Context:
Vitiligo is a common primary acquired pigmentary disorder due to loss of epidermal functioning melanocytes. Many surgical techniques have evolved over the years for its treatment and the need of a cost-effective modality has always been put forward.
Aim:
The aim of the study was to compare the efficacy of non-cultured epidermal cell suspension with that of epidermal curettage in repigmentation of stable vitiligo.
Settings and Design:
It was a prospective randomized non-controlled study.
Subjects and Methods:
Forty lesions were selected in patients of stable, recalcitrant vitiligo belonging to different age-groups and genders. After histopathological confirmation, the patients were taken up for surgery after obtaining written consent and were divided into two groups for two different procedures, that is, non-cultured epidermal cell suspension (Group A) and epidermal curettage (Group B). Follow-up was carried out at 2, 4, 8, and 12 weeks of procedure to assess the repigmentation achieved.
Statistical Analysis:
Statistical Package for Social Sciences (SPSS) software, version 21.0, was used.
Results:
At the end of the study, >50% repigmentation was achieved in 95% (19 of 20) lesions of Group A and 85% (17 of 20) lesions in Group B, whereas >75% repigmentation was achieved in 60% (12 of 20) in both Groups A and B. The color matching with surrounding skin and yield of graft was better in epidermal cell suspension technique than that in epidermal curettage. The difference was not statistically significant.
Conclusion:
Though both the surgical techniques of melanocyte transplantation are effective in achieving uniform pigmentation, epidermal curettage has an extra edge of being simpler and more cost-effective.
Keywords
Epidermal cell suspension
epidermal curettage
mupirocin ointment
stable vitiligo
Epidermal curettage is a simple and cost-effective surgical technique for achieving uniform pigmentation and suitable for beginners in dermatosurgery.

INTRODUCTION
Vitiligo is a common, acquired, primary progressive depigmenting disorder of obscure etiology, which manifests clinically as well-defined achromic macules and patches.[1] It is characterized by immune-mediated destruction of melanocytes, leading to well-circumscribed areas of depigmentation. Vitiligo occurs in 0.5%–2% of the world population.[23] It has been reported in monozygotic twins.[4]
Numerous medical therapies are available including phototherapy but surgical transplantation remains the last resort for recalcitrant stable lesions.[5] There are two forms of surgical techniques: cellular and tissue grafting. Autologous non-cultured epidermal cell suspension (NCES) and epidermal curettage (EC) are two subtypes of cellular and tissue grafting, respectively.
NCES is a novel addition to the therapeutic armamentarium for vitiligo. It was introduced in 1992 by Gauthier and Surleve-Bazeille.[6] It yields cosmetically acceptable results within a short period and has become more practitioner friendly.[7]
In EC, epidermal curettes are obtained following the dermabrasion of the donor area.[8] Epidermal curettes can be used as grafting material because of the abundance of melanocytes in them.[9] A study with modification of the procedure was conducted in which 2% mupirocin ointment was applied over the donor area and epidermal curettes were obtained from the donor area. This technique is also known as Jodhpur Technique, and the use of ointment helped in better entanglement of the separated epidermal curettes and thus prevented the loss of graft material.[9]
This study was aimed to compare these two surgical modalities in terms of repigmentation so that a dermatologist even in remote settings can opt for the best technique and help in mitigating the stigma associated with this depressing disorder.
SUBJECTS AND METHODS
After taking the approval from Institutional Ethics Committee, 40 lesions in 20 histologically proven cases of localized, stable, recalcitrant vitiligo were selected at random from the OPD of the Department of Dermatology, Venereology, and Leprosy of a tertiary care hospital in North India between April 2018 and June 2019. The selected patients fulfilled the following criteria:
Inclusion criteria
Stable lesions of vitiligo with no progression in the form of appearance of new lesions or enlargement in the existing lesions for at least 12 months preceding the study, only emotionally stable patients with age more than 12 years without any active infections were included.
Exclusion criteria
Patients with active disease, age less than 12 years, infection at the site of transplantation or on any other part the body, keloidal diathesis, hypopigmentation as a result of minor trauma, positive Koebner phenomenon, bleeding diathesis, pregnancy, lesions occurring over mucosa, palms and soles, patients with a history of autoimmune disease, especially autoimmune thyroiditis, diabetes mellitus, or pernicious anemia comprised the exclusion criteria.
Written consent was obtained, and the selected lesions were divided into two groups, that is, A and B. In Group A, 20 lesions were subjected to NCES, whereas in Group B, 20 lesions were subjected to EC.
To measure the area of each lesion, a flexible transparent plastic sheet was placed over each lesion and boundaries of the lesion were outlined. The same outlined sheet was fixed over a graph paper with centimeter scaling to count the total number of complete and incomplete boxes of graph paper, and the final value was recorded after the addition of all the boxes.
Procedure for autologous NCES
The surgical site was shaved off of any hairs before, and surgical preparation was done with Cetavlon (Cetavlon-Conc, ICI Healthcare Pvt. Ltd., Scottish Mall, Gurugram, Haryana), povidone-iodine, and surgical spirit. Local anesthesia was achieved with Emla (Prilox, Uttaranchal Biotech Limited, Dineshpur Road, Rudrapur Uttarakhand) (2.5% lignocaine and 2.5% prilocaine) patch applied 60 min preoperatively or with 1% Xylocaine and adrenaline infiltration. For harvesting thin split-thickness graft, the skin was held flat and made taut by stretching. By holding the cutting edge of a razor blade with artery forceps parallel to skin surface, it was advanced to cut tangentially through the upper papillary dermis to obtain split skin graft of thinnest possible thickness. A good quality graft is the one that floats on the saline without curling on the sides. The graft was placed in a petri dish containing normal saline (NS). The thin split skin graft specimen was transferred under aseptic conditions to the petri dish containing 0.25% trypsin ethylenediaminetetraacetic acid (EDTA) solution. Then the specimen was incubated at 37°C using an incubator for 50 min with the epidermal side upward. After incubation, the trypsin-EDTA solution was pipetted out, and the grafts were washed in phosphate buffer saline to neutralize the trypsin. Dermis was separated from the epidermis. The dermal side of the epidermal layer was scraped using a blunt forceps to release cells from the basal layer of the epidermis into the saline. The solid waste of tissue was removed. The suspension thus obtained was centrifuged at 1000rpm for 5 min. The supernatant was discarded, and the pellet containing melanocytes and basal keratinocytes was transferred to the recipient site after dermabrasion.
Procedure for EC
After applying mupirocin 2% ointment, the donor site was dermabraded by mechanical or electrical dermabrader up to the dermo-epidermal junction. The ideal level was when pinpoint bleeding spots appeared. The epidermal curettes obtained by this procedure were collected by a spatula and placed on a glass slide containing NS and subsequently transferred to the recipient site after dermabrasion.
At both sites, caution was taken to cover the periphery of the lesion carefully to achieve uniform repigmentation. After washing with NS, a meshed collagen sheet (Kollagen M, Eucare Pharmaceuticals Pvt. Ltd., SIDCO Industrial Estate, Thirumudivakkam, Chennai, Tamil Naidu) was put over both grafts, which was further covered with sterile gauge pieces moistened with phosphate buffer saline. Dressing was done uniquely so that it did not stick to the graft. The patients were observed for 1h after the procedure. They were strictly immobilized for approximately 6h and hospitalized with instruction to take complete rest and avoid vigorous activities. They were advised to perform only restricted movements for the next 10 days, after which the dressing was opened.
Postoperative follow-up
The patients of both groups were assessed postoperatively after 2, 4, 8, and 12 weeks to (1) assess the progress of repigmentation, (2) evaluate donor area recovery, and (3) observe the complications both at recipient and donor sites, if any.
Repigmentation in both the treated areas was matched with the surrounding normal skin at the end of 3 months and the grading of repigmentation was done [Table 1], followed by statistical analysis using Statistical Package for Social Sciences (SPSS IBM Corp., Armonk, NY, USA) software, version 21.0.
| Percentage of repigmentation | Grade | Repigmentation |
|---|---|---|
| No repigmentation | Grade 0 | Nil |
| <25% | Grade I | Poor |
| 26%–50% | Grade II | Fair |
| 51%–75% | Grade III | Good |
| >75% | Grade IV | Excellent |
RESULTS
Of 20 cases in our study, the maximum number, that is, 10 (50%) cases were in the age-group of 21–25 years, followed by 7 (35%) cases in the age-group of 26–30 years, and 3 cases were younger than 20 years of age. The mean age in all the 20 patients was 23.50 years. Of the total patients, 11 (55%) cases were females and the remaining 9 (45%) cases were males. The total duration varied from 3.5 to 18 years, and the mean duration of disease in 20 study cases was 8.80 ± 4.05 years. Maximum number, that is, 15 (75%) cases had non-segmental vitiligo, followed by 3 (15%) cases of localized focal type, and 2 (10%) cases had segmental vitiligo. The duration of the stability of the disease process in 20 study cases varied between 1 and 7 years. The disease was stable for 1–2 years in 8 (40%) cases and for 2–4 years in 6 (30%) cases. It was stable for more than 4 years in 3 (15%) cases, whereas 3 (15%) patients had disease stable for 1 year. Vitiligo lesions present over different sites were taken up for surgery in Group A and B [Table 2].
| Site of operation | Group A | Group B | ||
|---|---|---|---|---|
| Number | Percentage | Number | Percentage | |
| Chin | 1 | 5.00 | 0 | 0.00 |
| Left cheek | 0 | 0.00 | 1 | 5.00 |
| Left elbow | 1 | 5.00 | 1 | 5.00 |
| Left foot | 6 | 30.00 | 4 | 20.00 |
| Left forearm | 2 | 10.00 | 4 | 20.00 |
| Left knee | 1 | 5.00 | 0 | 0.00 |
| Left leg | 2 | 10.00 | 2 | 10.00 |
| Left shoulder | 3 | 15.00 | 0 | 0.00 |
| Left side chest | 1 | 5.00 | 2 | 10.00 |
| Neck | 1 | 5.00 | 1 | 5.00 |
| Right cheek | 1 | 5.00 | 1 | 5.00 |
| Right leg | 1 | 5.00 | 4 | 20.00 |
| Total | 20 | 100.00 | 20 | 100.00 |
In Group A, repigmentation improved with subsequent follow-ups, and at the end of 12th week, 19 (95%) lesions showed >50% repigmentation and 12 (60%) lesions attained excellent repigmentation [Figure 1]. Likewise in Group B, 17 (85%) lesions achieved >50% repigmentation and 12 (60%) lesions had achieved Grade IV repigmentation at the 12th week of follow-up [Figure 2].
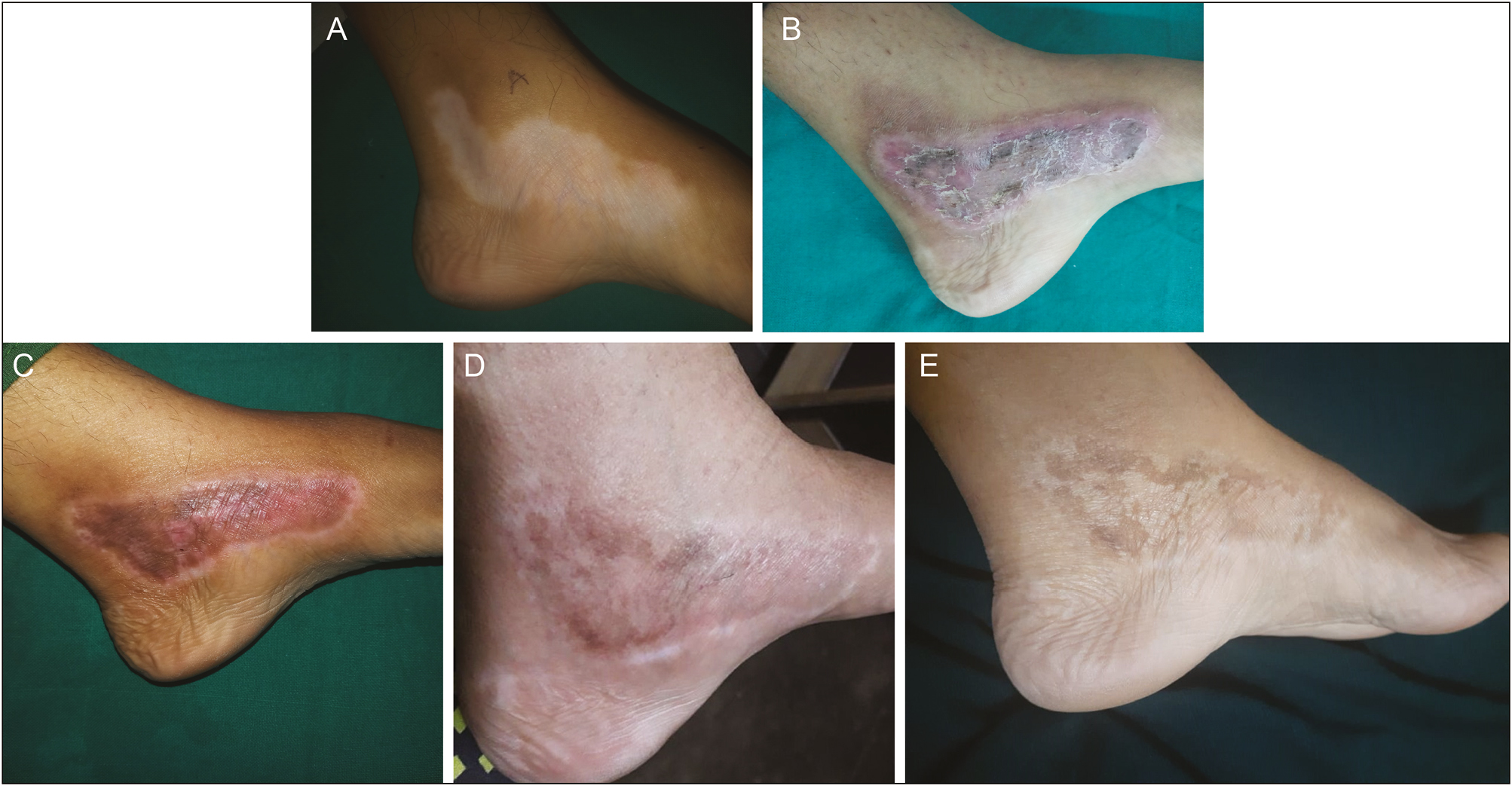
- A 28-year-old woman with vitiligo patch on left foot showing excellent pigmentation (92%) after treatment with NCES. (A) Preoperative. (B) After 2 weeks. (C) After 4 weeks. (D) After 8 weeks. (E) After 12 weeks
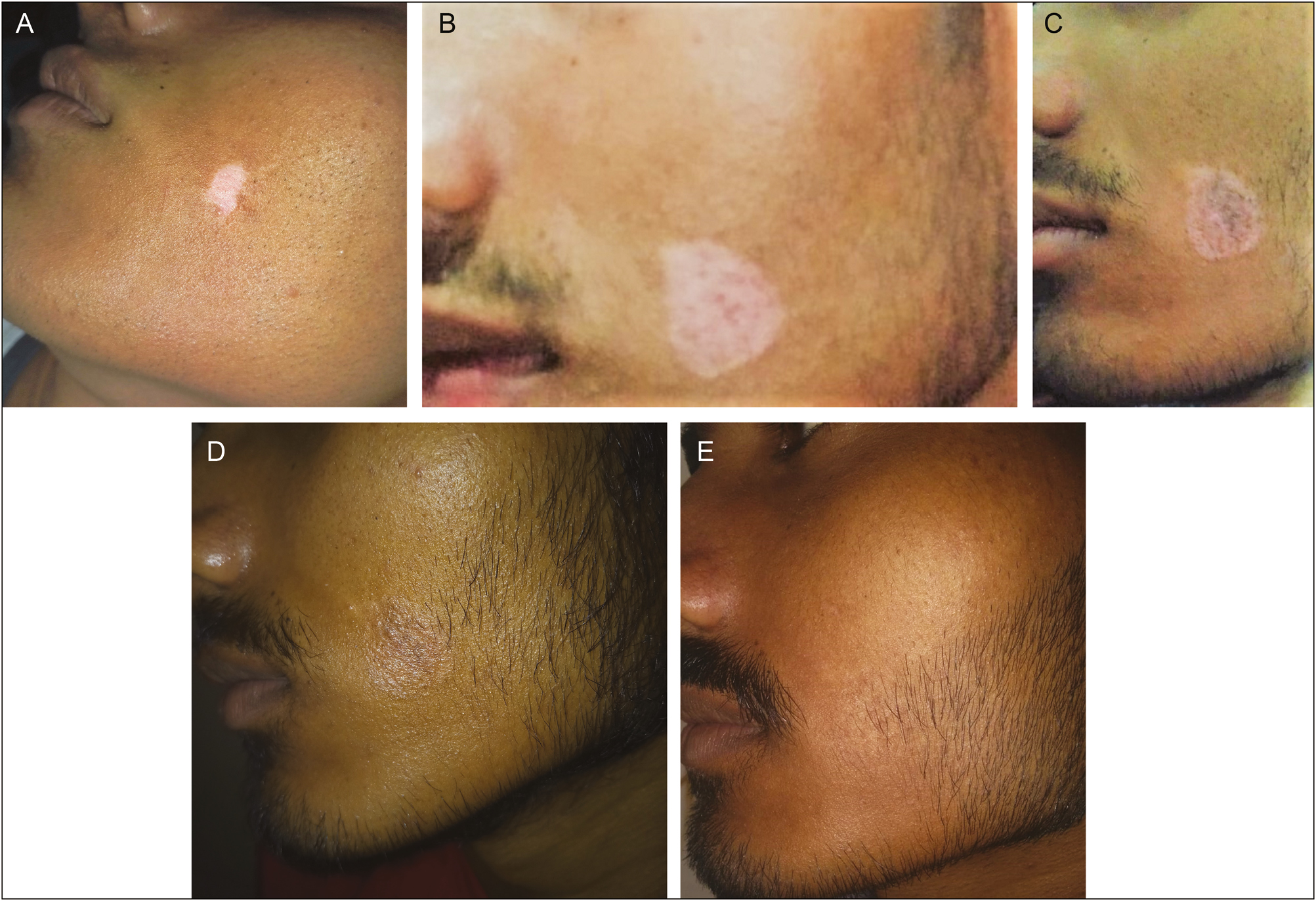
- A 18-year-old man with vitiligo patch on left cheek showing excellent pigmentation (100%) after treatment with EC. (A) Preoperative. (B) After 2 weeks. (C) After 4 weeks. (D) After 8 weeks. (E) After 12 weeks
When differences in results of repigmentation were analyzed in Group A itself (at 2nd, 4th, 8th, and 12th week), it was found to be statistically highly significant [Table 3]. On similar analysis in Group B, results were found to be statistically highly significant [Table 4], indicating that appreciable degree of repigmentation had started from 2 weeks onward of follow-up in both the groups. On comparing the degree of repigmentation in Group A with Group B at 2nd, 4th, 8th, and 12th week, the result was found to be statistically insignificant [Table 5, Figures 3 and 4, and Graph 1].
| WRS test comparative time group | Negative | Positive | Tie | Z value | P value | Significance |
|---|---|---|---|---|---|---|
| From 2 weeks to 4 weeks | 0 | 18 | 2 | -3.947 | 0.001 | Highly significant |
| From 2 weeks to 8 weeks | 0 | 20 | 0 | -3.982 | 0.001 | Highly significant |
| From 2 weeks to 12 weeks | 0 | 20 | 0 | -4.089 | 0.001 | Highly significant |
| From 4 weeks to 8 weeks | 0 | 17 | 3 | -3.787 | 0.001 | Highly significant |
| From 4 weeks to 12 weeks | 0 | 20 | 0 | -4.038 | 0.001 | Highly significant |
| From 8 weeks to 12 weeks | 0 | 8 | 12 | -2.828 | 0.005 | Significant |
| WRS test comparative time Group B | Negative | Positive | Tie | Z value | P value | Significance |
|---|---|---|---|---|---|---|
| From 2 weeks to 4 weeks | 0 | 14 | 6 | -3.638 | 0.001 | Highly significant |
| From 2 weeks to 8 weeks | 0 | 19 | 1 | -3.873 | 0.001 | Highly significant |
| From 2 weeks to 12 weeks | 0 | 19 | 1 | -3.903 | 0.001 | Highly significant |
| From 4 weeks to 8 weeks | 0 | 17 | 3 | -3.758 | 0.001 | Highly significant |
| From 4 weeks to 12 weeks | 0 | 19 | 1 | -3.977 | 0.001 | Highly significant |
| From 8 weeks to 12 weeks | 0 | 12 | 8 | -3.357 | 0.001 | Highly significant |
| Follow-up | Grade of repigmentation | No. of lesions % | χ2 | P value | Significance | |||
|---|---|---|---|---|---|---|---|---|
| Group A | Group B | |||||||
| No. | % | No. | % | |||||
| 2nd week | Grade 0 | 3 | 15 | 4 | 20 | 0.476 | 0.788 | Not significant |
| Grade I | 15 | 75 | 15 | 75 | ||||
| Grade II | 2 | 10 | 1 | 5 | ||||
| Grade III | 0 | 0 | 0 | 0 | ||||
| Grade IV | 0 | 0 | 0 | 0 | ||||
| 4th week | Grade 0 | 0 | 0 | 1 | 5 | 4.485 | 0.214 | Not significant |
| Grade I | 4 | 20 | 7 | 35 | ||||
| Grade II | 11 | 55 | 11 | 55 | ||||
| Grade III | 5 | 25 | 1 | 5 | ||||
| Grade IV | 0 | 0 | 0 | 0 | ||||
| 8th week | Grade 0 | 0 | 0 | 0 | 0 | 2.783 | 0.426 | Not significant |
| Grade I | 0 | 0 | 2 | 10 | ||||
| Grade II | 5 | 25 | 6 | 30 | ||||
| Grade III | 7 | 35 | 7 | 35 | ||||
| Grade IV | 8 | 40 | 5 | 25 | ||||
| 12th week | Grade 0 | 0 | 0 | 0 | 0 | 1.667 | 0.644 | Not significant |
| Grade I | 0 | 0 | 1 | 5 | ||||
| Grade II | 1 | 5 | 2 | 10 | ||||
| Grade III | 7 | 35 | 5 | 25 | ||||
| Grade IV | 12 | 60 | 12 | 60 | ||||

- Comparison of repigmentation in a 25-year-old man with vitiligo patch on both cheeks showing excellent pigmentation (100%) after treatment with NCES (A–E)
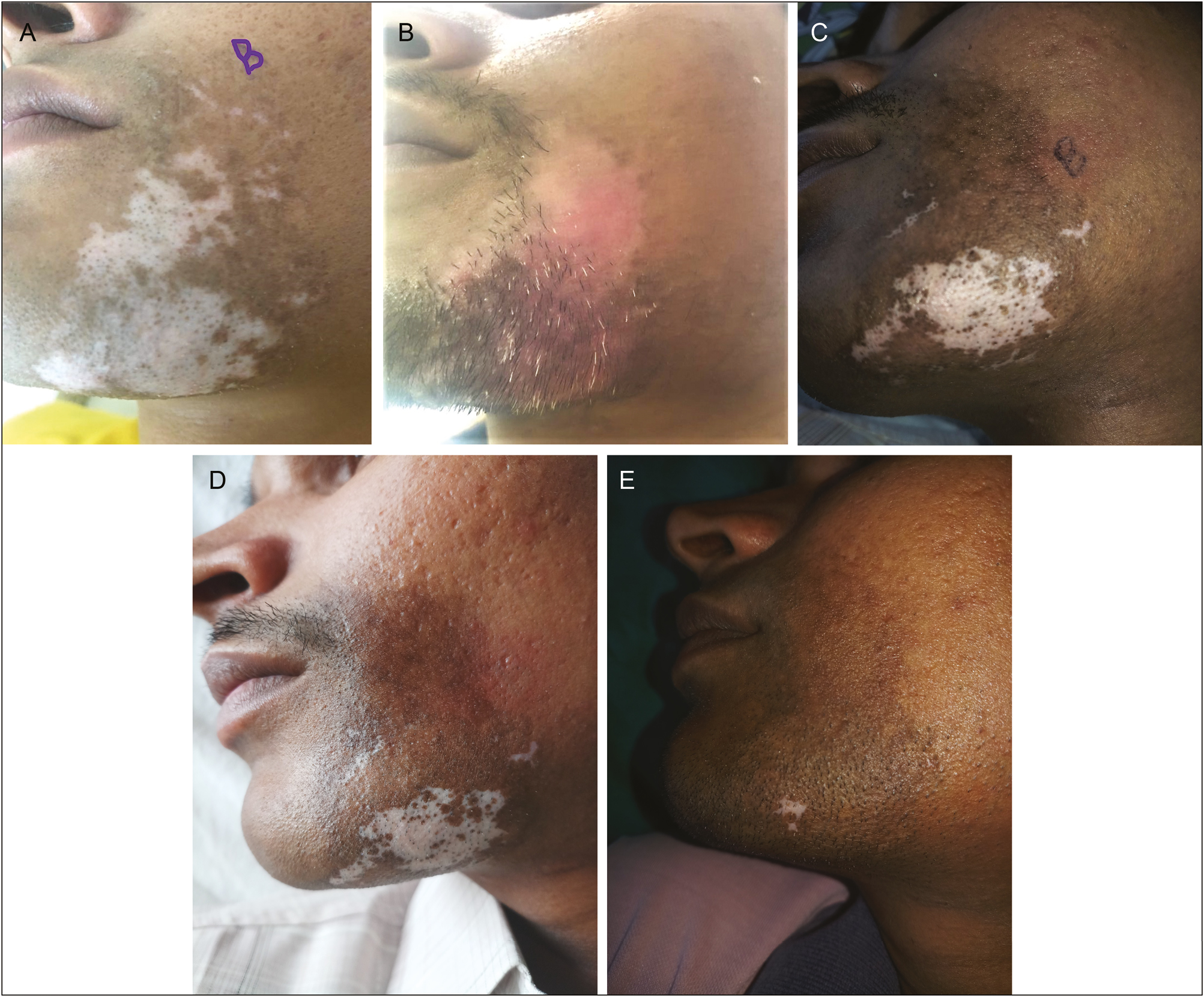
- Comparison of repigmentation in a 25-year-old man with vitiligo patch on both cheeks showing excellent pigmentation (90%) after treatment with EC (A–E)
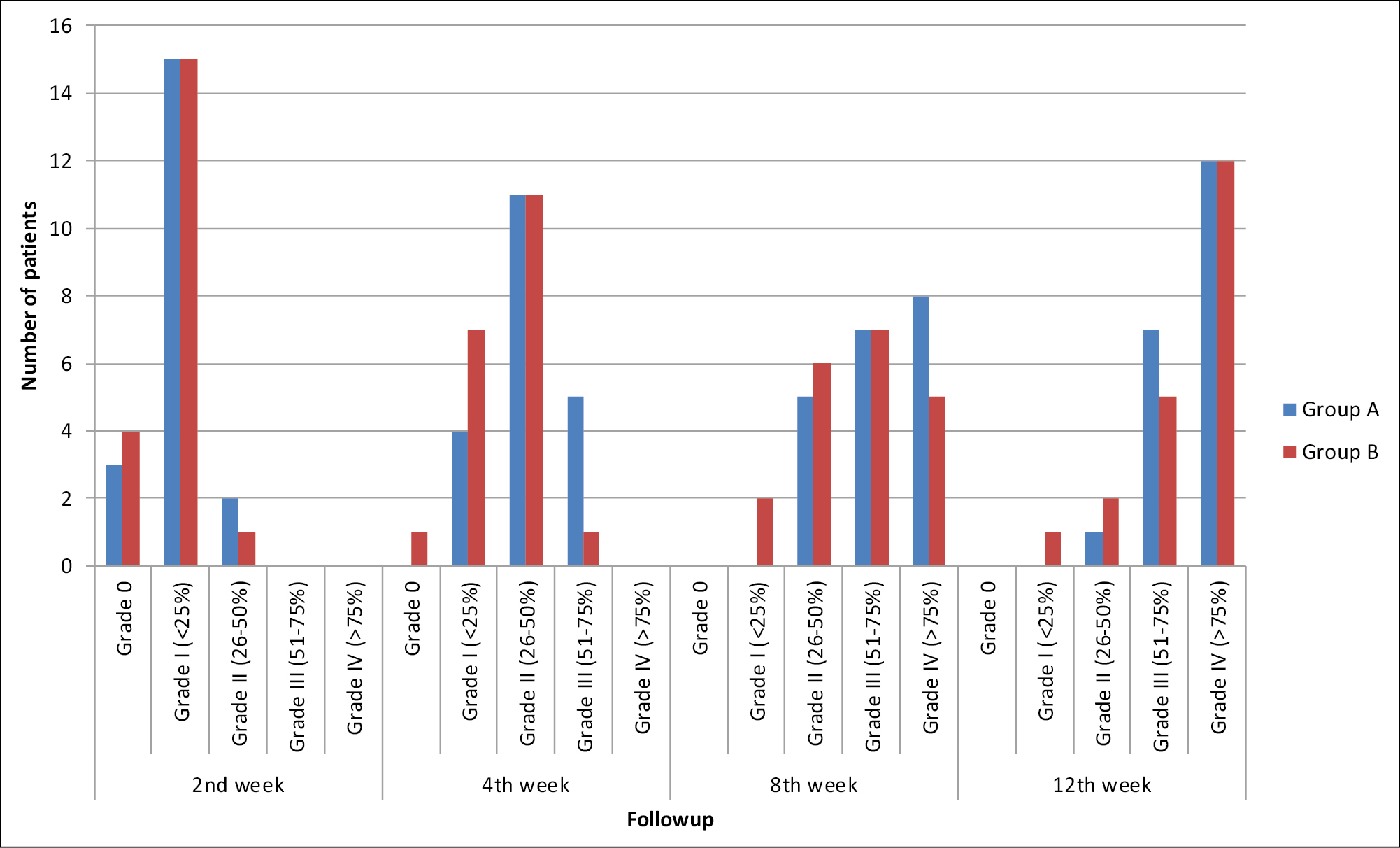
- Graph showing repigmentation in Group A and B after 2nd, 4th, 8th, and 12th week of follow-up
The complications at recipient sites in both groups were few. In Group A, 4 (20%) lesions presented with secondary infection on 2nd week of follow-up, which was managed by oral and topical antibiotics, 1 (5%), 2 (10%), and 4 (20%) lesions showed hyperpigmentation at 4th, 8th, and 12th week, respectively. No other complications in the form of atrophy, scarring keloids were noticed. In Group B, 1 (5%) lesion showed hyperpigmentation and 4 (20%) lesions presented with secondary infection, which was managed with oral and topical antibiotics at the 2nd week of follow-up. At the end of 4th, 8th, and 12th week, 1 (5%), 3 (15%), and 8 (40%) lesions developed hyperpigmentation, respectively. No other complications in the form of nausea, vomiting, and keloid formation were observed in both groups.
The donor sites presented with few complications in both the groups. In Group A, 2 (10%) lesions presented with infection after 2 weeks and 1 (5%) lesion developed hyperpigmentation at 4th week. No other complication was observed on subsequent follow-ups at 8th and 12th week. In Group B, 2 (10%) lesions each presented with hyperpigmentation and infection after 2 weeks of follow-up, whereas only 1 (5%) lesion presented with hyperpigmentation after 4 weeks. No complication was observed at the 8th and 12th week of follow-up.
DISCUSSION
There are many forms of medical treatment, and approximately 80% of patients respond to medical treatment. Surgical treatment of vitiligo is the final resort to regain the pigmentation if medical and light therapy fails.[5] Various surgical modalities for vitiligo are available now and have been tried with the variable outcome such as suction blister grafting, smash grafting, split-thickness grafting, and punch grafting. However, these procedures can treat only a limited area at a time.[101112] Although surgical methods have their limitations and side effects, they still appear to be the modality of choice in patients of stable vitiligo.
Being a pioneer study, not much has been reported in literature about the comparison of quality and degree of repigmentation achieved after NCES and EC. As variation in results has been observed by different authors and as such no comparative study has ever been undertaken in this part of our country to the best of our knowledge, we endeavored to assess these two different techniques in our patients of vitiligo regarding the outcome of results as far as repigmentation in vitiligo lesion is concerned with least possible complications.
Autologous melanocytic transplantation by NCES is a safe and effective technique.[13] In our study, after 12 weeks of follow-up, 12 (60%) lesions developed excellent repigmentation, 7 (35%) lesions attained good repigmentation, whereas 1 (5%) lesion developed fair repigmentation. Our results in Group A were found to be better than those reported by Van Geel et al.[14] who could achieve repigmentation in 3–12 months in their cases. Olsson and Juhlin[15] reported an 85% success rate after the application of basal cell layer epidermal cell suspension rich in melanocytes. The treated area in their study ranged from two to ten times the donor area, which was comparable to our study. Repigmentation of more than 90% was observed in 88.8% of people in a study conducted by Sahni and Parsad[16] on autologous melanocyte transplantation using patients’ serum after 16 weeks of surgery. This variation in our study could be attributed to the size of the study sample, short duration of follow-up, and involvement of different anatomic sites. According to Mulekar,[17] more than 50% of patients treated for difficult sites showed more than 65% repigmentation of the treated areas by the NCES. In a recent study, 35% of acral lesions (excluding those on fingertips and toes) showed excellent repigmentation with no difference in outcome found between difficult-to-treat sites and other sites.[18] In Group A, 4 (20%) lesions presented with secondary infection on the 2nd week of follow-up, and 1 (5%), 2 (10%), and 4 (20%) lesions showed hyperpigmentation at 4th, 8th, and 12th week, respectively. A recent study conducted by Hamza et al.[19] showed no complication at the recipient site. This difference could be due to exposure of sunlight during the postoperative period in our patients as compared to the controlled exposure of Narrow Band UVB used by Hamza et al.[19] At the donor site, 2 (10%) lesions presented with infection after 2 weeks and 1 (5%) lesion developed hyperpigmentation at 4th week. A study conducted by Leelavathy et al.[20] showed hyperpigmentation in 43% and scarring in 13% of their patients at the donor site. The fewer complications in our study could be due to the harvesting of a thin split-thickness graft that appeared translucent when kept in petri dish with NS.
EC is an easy and cost-effective surgical technique that does not require split-thickness grafting. Only a few studies have been reported in the literature regarding this procedure.[2122] Our results in Group B were better than those reported by Kachhawa et al.[23] in which after 6 months of follow-up, 83% lesions showed repigmentation with only 26% lesions showing excellent (>75%) repigmentation, whereas in our study, after 12 weeks of follow-up, all of the lesions achieved repigmentation with 12 (60%) lesions achieving excellent repigmentation. Hyperpigmentation was observed in 8 (40%) lesions as a complication at the end of follow-up in our study as compared to the study conducted by Kachhawa et al.,[23] in which no complication was seen. This disparity of results may be due to sunlight exposure during the postoperative period in our patients as compared to the controlled NB-UVB exposure used in the latter study. No donor site complications were recorded by the same authors as compared to our study, in which, secondary infection and hyperpigmentation were observed during the initial follow-ups of 2nd and 4th week, which later on resolved on subsequent follow-ups of 8th and 12th week.
CONCLUSION
To the best of our knowledge, ours is the first study comparing the NCES and EC. Both the techniques were found to be safe and effective with comparable efficacy for achieving even repigmentation in cases of stable vitiligo after 12 weeks of follow-up.
As repigmentation progresses gradually and may continue even beyond 12 months following the transplantation procedure, it is recommended that a further study comprising larger number of patients who are followed up for longer period (minimum 6 months) should be undertaken to arrive at any conclusion about the efficacy of these newer, safe, simple, and cost-effective surgical modalities with which refractory areas of vitiligo can also be treated without any complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Etiopathogenesis of vitiligo: are we dealing with an environmental disorder? Indian J Dermatol Venerol Leprol. 1999;64:161-5.
- [Google Scholar]
- Pigmentary disorders. In: Valia RG, Ameet V, eds. IADVL Text Book Dermatology (3rd ed). Mumbai, India: Bhalani Publishing House; 2008. p. :749-58.
- [Google Scholar]
- Disorders of skin colour. In: Burns T, Breathnach S, Cox N, Griffiths C, eds. Rook’s Text Book of Dermatology (7th ed). London, UK: Blackwell; 2004. p. :pp. 39-13.
- [Google Scholar]
- Segmental vitiligo. In: Lahiri K, Chatterjee M, Sarkar R, eds. Pigmentary Disorders. A Comprehensive Compendium. New Delhi, India: Jaypee Brothers; 2014. p. :167-80.
- [Google Scholar]
- Treatment of refractory and stable vitiligo by transplantation of in vitro cultured epidermal autografts bearing melanocytes. J Am Acad Dermatol. 1992;26:230-6.
- [Google Scholar]
- Direct melanocytes transplant from normal donor area into vitiliginous recipient area by dermabrasion technique. J Cosmet Dermatol Sci Appl. 2012;2:288.
- [Google Scholar]
- Keratinocyte-melanocyte graft technique followed by PUVA therapy for stable vitiligo. Indian J Dermatol Venereol Leprol. 2008;74:622-4.
- [Google Scholar]
- Miniature punch grafting. In: Savant SS, Gore D, Atal SR, Sarangi K, eds. Text Book of Dermatosurgery Cosmetology (2nd ed). Mumbai, India: ASCAD; 2005. p. :359-69.
- [Google Scholar]
- Suction blister technique. In: Savant SS, Gore D, Atal SR, Sarangi K, eds. Text Book of Dermatosurgery Cosmetology (2nd ed). Mumbai, India: ASCAD; 2005. p. :351-8.
- [Google Scholar]
- Thin Thiersch’s split thickness skin grafting. In: Savant SS, Gore D, Atal SR, Sarangi K, eds. Text Book of Dermatosurgery Cosmetology (2nd ed). Mumbai, India: ASCAD; 2005. p. :345-50.
- [Google Scholar]
- Four compartment method: a simplified and cost-effective method of noncultured epidermal cell suspension for the treatment of vitiligo. Br J Dermatol. 2014;170:581-5.
- [Google Scholar]
- Surgical technique for vitiligo: a review. Indian J Dermatol Venereol Leprol. 2001;202:162-6.
- [Google Scholar]
- Repigmentation of vitiligo by transplantation of autologous cultured melanocytes. Acad Dermatol. 1993;72:49-51.
- [Google Scholar]
- Stability in vitiligo: is there a perfect way to predict it? J Cutan Aesthet Surg. 2013;6:75-82.
- [Google Scholar]
- Long-term follow-up study of segmental and focal vitiligo treated by autologous, noncultured melanocyte-keratinocyte cell transplantation. Arch Dermatol. 2004;140:1211-5.
- [Google Scholar]
- Long-term follow-up of patients undergoing autologous noncultured melanocyte-keratinocyte transplantation for vitiligo and other leukodermas. J Am Acad Dermatol. 2017;77:318-27.
- [Google Scholar]
- Noncultured extracted hair follicle outer root sheath cell suspension versus noncultured epidermal cell suspension in the treatment of stable vitiligo. J Cutan Aesthet Surg. 2019;12:105-11.
- [Google Scholar]
- To evaluate the efficacy of non-cultured epidermal cell suspension in cases of stable vitiligo. Clin Surg. 2017;2:1527.
- [Google Scholar]
- Vitiligo: analysis of grafting versus curettage alone, using melanocyte morphology and reverse transcriptase polymerase chain reaction for tyrosinase mRNA. Sao Paulo Med J. 2005;123:187-91.
- [Google Scholar]
- Melanocytes and keratinocytes transfer using sandpaper technique combined with dermabrasion for stable vitiligo. Dermatol Surg. 2011;37:192-8.
- [Google Scholar]
- Simplified non-cultured non-trypsinised epidermal cell graft technique followed by psoralen and ultraviolet A light therapy for stable vitiligo. J Cutan Aesthet Surg. 2017;10:81-5.
- [Google Scholar]





