Translate this page into:
Fractional Carbon Dioxide Laser versus Combined Fractional Carbon Dioxide Laser with Platelet-rich Plasma in the Treatment of Atrophic Post-acne Scars: A Split-face Comparative Study
Address for correspondence: Dr. Tanreet Kaur, House No 22, Street No 2, Gopal Nagar, Majitha Road, Amritsar, 14001, Punjab. E-mail:tanreet.grewal@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Context:
Though many treatment options are available for treating post-acne scars, optimized treatment still does not exist. Till date, comparative split-face studies, analyzing the efficacy of combined treatment modalities for acne scars with adequate sample size and with statistically significant results, are still lacking.
Aim:
The aim of this study was to compare the effectiveness of the combined use of platelet-rich plasma (PRP) and fractional ablative CO2 laser (FACL) versus FACL in the management of acne scars and to study the safety of autologous PRP and FACL in the treatment of post-acne scars.
Settings and Design:
This was a randomized split-face trial study.
Materials and Methods:
This study was conducted in 30 patients having Goodman and Baron’s grade 3 and 4 acne scars. The efficacy of PRP in combination with FACL was compared to FACL alone in the treatment of post-acne scars. Right half of the patient’s face was taken as the study side where FACL was performed followed by PRP injections. The left half of the same patient’s face was taken as the control side where FACL was performed followed by normal saline injections.
Statistical Analysis:
Results were analyzed using Statistical Package for the Social Sciences (SPSS, Chicago).
Results:
At the time of enrollment, mean Goodman and Baron Acne Qualitative Grading Scale on study and control side was 3.80 with standard deviation (SD) of 0.40 at baseline. After completion of four treatment sessions, it was reduced to 2.43 (SD = 0.76) and 2.76 (SD = 0.49) on the study and control side, respectively. Improvement on both sides was statistically significant (P = 0.000).
Conclusion:
There is no single proven modality for the effective treatment of post-acne scars. Combination of FACL with newer adjuvants such as PRP has definitive role in managing post-acne scars with better safety profile than FACL alone.
Keywords
Acne scars
Goodman and Baron’s qualitative acne scar grading system
lasers
platelet-rich plasma
INTRODUCTION
Acne vulgaris can be defined as chronic, self-limiting, and an inflammatory disease of pilosebaceous unit, manifesting generally in adolescence with pleomorphic lesions such as comedones, papules, pustules, nodules, and cysts.[1] Untreated acne, especially the inflammatory type, results in often distressing scars.[2] It is difficult to treat all acne scar types satisfactorily with a single treatment option. Hence, combination therapy is better suited for managing post-acne scars. The potential role of platelet-rich plasma (PRP) in dermatology and aesthetic medicine is an exciting frontier that may eventually lead to superior therapies in the near future. Hence, this split-face study was conducted in 30 patients with an aim to evaluate the efficacy of PRP in combination with fractional ablative CO2 laser (FACL) versus FACL alone.
MATERIALS AND METHODS
For this study, a total of 30 patients with Goodman and Baron’s acne scar of grade 3 and 4 who presented to the outpatient department of dermatology, venereology, and leprosy at Sri Guru Ram Das Institute of Medical Sciences and Research, Sri Amritsar, Punjab, India, were enrolled. It was a split-face study in which the right half of patient’s face was taken as the study side where FACL (Sellas Cis F1-Fractional CO2 Laser) was performed followed by PRP injections. Parameters of FACL used were, pattern, scatter; mode, stamping; PPA, 49; fluence, 25–45 mJ/cm2; and number of passes, single. Double-spin method was used to prepare PRP. A total of 20 mL of patient’s blood was collected in a sterile vacutainer tube containing an anticoagulant acid citrate dextrose-A. First, slow spin was performed at 1000 revolution per minute for 10 min at room temperature. After the first spin, plasma was gently aspirated and transferred to the second set of vacutainers. Second spin (heavy spin) was performed at room temperature at the rate of 2000 RPM for 5 min. The upper two-third of this double-spinned plasma was collected as platelet-poor plasma, and the bottom one-third was used as PRP. PRP was injected intradermally through a 30 G needle. The amount injected was sufficient to elevate and blanch the scar. Injection sites were located within 2-cm interval to receive 0.2 mL PRP or normal saline. The total amount injected was 1–2 mL depending on the number of scars. The left half of the same patient was taken as the control side, where FACL was performed followed by normal saline injections. The procedure was performed under topical anesthesia (combination of prilocaine 2.5% and lignocaine 2.5%) under occlusion for approximately 45 min before the procedure. In addition, while injecting PRP injections, ice pack was applied to reduce pain when required. A total of four such treatment sessions were performed at an interval of 4 weeks. Intermittent treatment in the form of topical sunscreen and strict photoprotection was advised. Follow-up was performed for 2 months after the last session. Outcomes and side effects were documented after each session and on follow-up.
Assessment parameters
Improvement of the patient was evaluated by using the following parameters:
Goodman and Baron’s qualitative acne scar grading system (Goodman and Baron Acne Qualitative Grading Scale [G and B AQGS]): Acne scars before and after treatment were graded using the aforementioned scale
Patient’s subjective score (PSS)
Patient was asked to score the severity of acne scars from 0 to 10, 10 representing maximum severity and 0 indicating no scars.
Inclusion criteria
All patients between the age-group 18–45 years presenting with G and B’s acne scars of grade 3 and 4
No history of prior dermatosurgical procedures for acne scars in past 6 months
Exclusion criteria
Active acne
Bleeding disorders
Active infection including herpes simplex virus infection
Human immunodeficiency virus (HIV) seropositivity
Facial scars due to causes apart from acne, for example, traumatic scars
Patients who were unwilling for follow-up and patients with unrealistic expectations
Platelet count less than 1 lakh/cm3 and hemoglobin less than 10 mg/dL
Patients with keloidal tendencies
RESULTS
The mean age of study population was 26.93 years (standard deviation [SD] = 4.77). Male to female ratio was 1.3:1. Of the total 30 patients, 6 patients (20%) had grade 3 acne scar and 24 (80%) had grade 4 acne scar [Table 1]. At the time of enrollment, patients with same acne scar grade on both sides were selected to ensure matching and to avoid bias [Figure 1]. Mean G and B AQGS on the study and control side was 3.80 with SD of 0.40 at baseline. After completion of four treatment sessions, it was reduced to 2.43 (SD = 0.76) and 2.76 (SD = 0.49) on the study and control side, respectively. Improvement on both sides was statistically significant (P = 0.000) [Table 2], [Figure 2]. Even though pretreatment G and B AQGS was equal on both the sides, pretreatment PSS differed on the study and control side because this score reflected patient’s self perception of their scarring. On the study side, pretreatment mean PSS was 8.56 (SD = 1.02), which was reduced to 4.07 (SD = 1.18) after completion of four treatment sessions, whereas on the control side, it was reduced to 6.30 (SD = 1.19) from baseline mean PSS of 8.46 (SD = 0.92) [Table 3]. Most common side effects reported were erythema and burning followed by edema, which was seen in 63.3% patients on the study side and in 90% patients on the control side. Other side effects reported were dryness, scabbing, persistent erythema, and postinflammatory hyperpigmentation as summarized in Table 4 [Figure 3].
| Age-group | Number of patients | Percentage |
|---|---|---|
| ≤20 years | 2 | 6.66 |
| 21–25 | 12 | 40.0 |
| 26–30 | 9 | 30.0 |
| ≥30 | 7 | 23.33 |
| Male | 17 | 56.66 |
| Female | 13 | 43.33 |

- Right half of patient’s face. (A) Baseline. (B) After four sessions. (C) On follow-up after 2 months
| Side of face | Before treatment | After 4th session | Wilcoxon signed-rank test | P value | ||
|---|---|---|---|---|---|---|
| Mean G and B AQGS | SD | Mean G and B AQGS | SD | |||
| Study | 3.80 | 0.40 | 2.43 | 0.76 | –4.702 | 0.000* |
| Control | 3.80 | 0.40 | 2.76 | 0.49 | –4.916 | 0.000* |
*denotes highly significant p value

- Left half of patient’s face. (A) Baseline. (B) After four sessions. (C) On follow-up after 2 months
| Side of face | Before treatment | After 4th session | Wilcoxon signed-rank test | P value | ||
|---|---|---|---|---|---|---|
| Mean PSS | SD | Mean PSS | SD | |||
| Study | 8.56 | 1.02 | 4.07 | 1.18 | –4.836 | 0.000* |
| Control | 8.46 | 0.92 | 6.30 | 1.19 | –4.751 | 0.000* |
*denotes highly significant p value
| Side effects | Study side | Control side | P value | Wilcoxon signed-rank test | |
|---|---|---|---|---|---|
| Erythema | Present (+) | 30 (100%) | 30 (100%) | 1*** | 0.00 |
| Absent (–) | - | - | |||
| Burning | + | 30 (100%) | 30 (100%) | 1*** | 0.00 |
| – | - | - | |||
| Edema | + | 19 (63.3%) | 27 (90%) | 0.033** | –2.138 |
| – | 11 (36.7%) | 3 (10%) | |||
| Scabbing | + | 22 (73.3%) | 24 (80%) | 0.317*** | –1.000 |
| – | 8 (26.7%) | 6 (20%) | |||
| Dryness | + | 19 (63.3%) | 27 (90%) | 0.005* | –2.828 |
| – | 11 (36.7%) | 3 (10%) | |||
| Persistent erythema | + | 4 (13.3%) | 8 (26.7%) | 0.04** | –2.000 |
| – | 26 (86.7%) | 22 (73.3%) | |||
| Postinflammatory hyperpigmentation | + | 6 (20%) | 10 (33.3%) | 0.04** | –2.000 |
| – | 24 (80%) | 20 (66.7%) | |||
| Acne aggravation | + | 5 (16.7%) | 8 (26.7%) | 0.083*** | –1.732 |
| – | 25 (83.3%) | 22 (73.3%) | |||
| Milia formation | + | 3 (10%) | 3 (10%) | 1*** | 0.000 |
| – | 27 (90%) | 27 (90%) |
*denotes highly significant p value; **significant p value; ***non significant p value
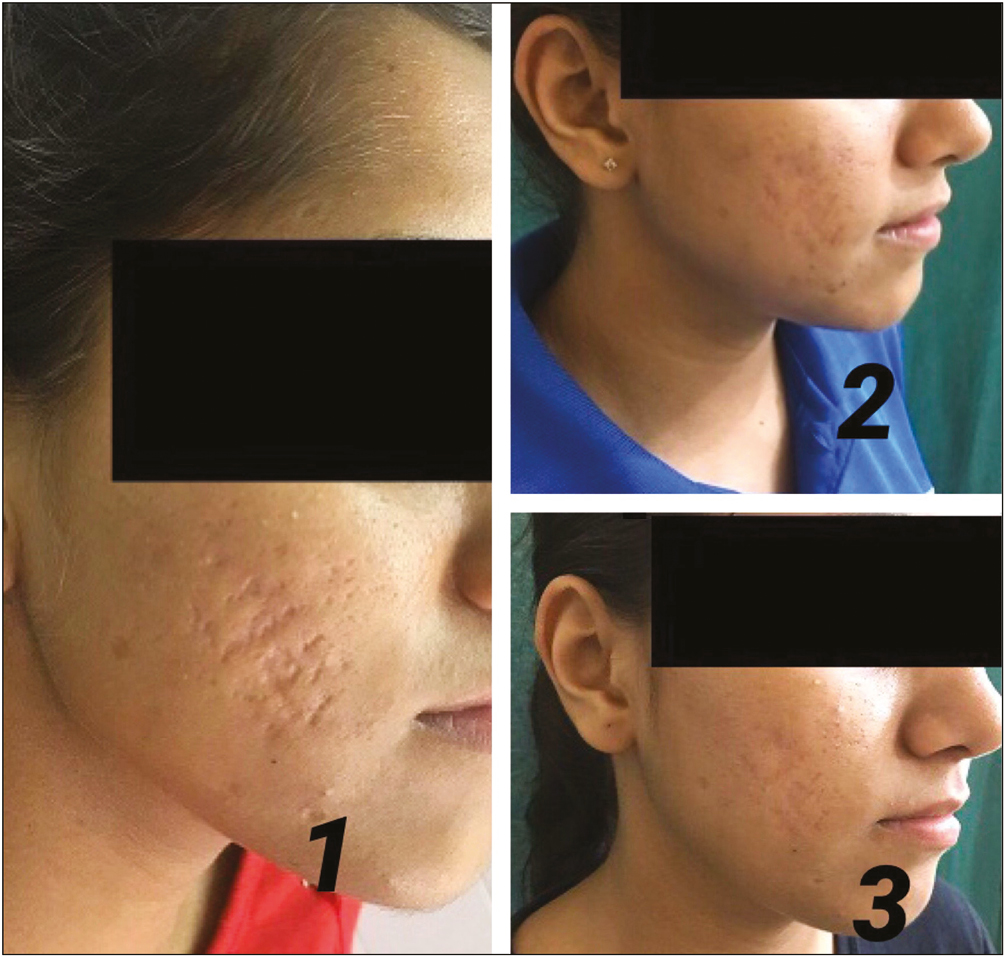
- Right half of patient’s face. (A) Baseline. (B) After four sessions. (C) On follow-up after 2 months
DISCUSSION
This study was conducted in an attempt to evaluate the role of adjuvant new therapies such as PRP along with time-tested established modalities such as FACL for managing post-acne scars.[3] In this study, mean G and B AQGS on the study and control side was 3.80 (SD = 0.40) at baseline. On the study side, after completion of four treatment sessions, the mean grade was reduced to 2.43 (SD = 0.76), whereas on the control side, it was reduced to 2.76 (SD = 0.49). The mean percentage improvement in G and B AQGS after four sessions on the study side (33.61%) was more as compared to the control side (26.94%). With Wilcoxon signed-rank test, this difference in improvement between the study and control side was statistically significant (P = 0.02). Similar results were obtained in a study conducted by Abdel Aal et al.,[4] in which excellent improvement was observed on right side where FACL was combined with intradermal PRP injections. In a split-face study by Shah et al.,[5] where outcomes after FACL with and without PRP injections were assessed using G and B quantitative scale, significant reduction was observed in acne scars on the study side (mean G and B quantitative grade was 14.83 at baseline and 4.2 at 4 months) and the control side (mean G and B grade was 15.23 at baseline and 7.5 at 4 months). Min et al.[6] also concluded that combined treatment approach with FACL and PRP for acne scar management appeared to be safe and effective. There are several mechanisms that could explain the synergistic effects of PRP on overall clinical improvement. Activated platelets possess α-granules containing secretory proteins (e.g., platelet derived growth factors and transforming growth factors).[7] These proteins bind to the receptors of target cells (e.g., mesenchymal stem cells, fibroblasts, endothelial cells, and epidermal cells) and direct cellular proliferation, matrix formation, collagen synthesis, and so forth. PDGF, TGF-β, and insulin like growth factors also facilitate chemotaxis and mitogenesis of stem cells, angiogenesis for capillary ingrowth, and enhance collagen synthesis.[8] Combination of FACL along with PRP is synergistic in a manner that microthermal zones created after laser treatment facilitates better absorption of PRP, leading to enhanced collagen remodeling because of various growth factors released from platelets. Faghihi et al.[9] revealed that overall clinical improvement of acne scars was higher on the side where FACL was combined with PRP than on the side where FACL was performed alone. But the difference was not statistically significant (P = 0.15) after the completion of treatment sessions. This study concluded that adding PRP to FACL treatment did not produce any statistically significant synergistic effects.[9] In this study, on the study side, mean PSS was 8.56 (SD = 18.75), which was reduced to 4.07 (SD = 1.18) after the completion of four treatment sessions with combined intradermal PRP injections and FACL. On the control side, mean PSS score was 8.46 (SD = 0.92), which was reduced to 6.30 (SD = 1.19) after FACL. Reduction in mean percentage of PSS was statistically significant on both sides of the face (P = 0.000). The reduction in mean PSS on the study side (52.45%) was more than that on the control side (25.41%) after completion of four sessions. In a study by Manuskiatti et al.,[10] efficacy of FACL in acne scar was assessed using subjective ratings. They reported an improvement of at least 50% in 62% patients as per subjective ratings.[10] Our study also reported improvement of 52.54% on the right side where FACL was performed in combination with PRP. After thorough review of literature, comparison among various related studies conducted so far is summarized in Table 5. The difference in the outcomes could be attributed to variation in the number of treatment sessions, follow-up period, lack of objective measurement tools for assessing improvement in acne scars, assessor’s bias in assessment, variable sample size of study population, and variation in laser parameters. In this study, all the patients developed early side effects such as burning and erythema after the procedure on both sides of the face. Posttreatment scabbing was seen in 80% of our patients over the control side and in 73.3% of patients over the study side. Edema was significantly (P = 0.015) more on the control side (seen in 90% patients) than that on the study side (seen in 63.3% patients). In a study by Shah et al.,[5] 83.33% patients developed edema after the procedure, majority of them (60%) belonged to the control side where FACL was performed along with intradermal normal saline injections. Persistent erythema was seen in 26.6% patients on the control side incidence, which was slightly higher than that on the study side (13.3%) patients. The lower incidence of dryness and edema on the study side could be explained by the effects of various growth factors present in PRP, which modifies the wound-healing properties of acne scar after FACL. A study by Min et al.,[6] on the effect of PRP on collagen production and modulation of laser-induced inflammation, concluded that the PRP treatment increased the clinical efficacy with decreased severity of adverse effects such as erythema, edema, and dryness. Even after topical application of PRP following FACL, the redness, swelling, and pain experienced by each patient were significantly lesser on the side treated with FACL in combination with PRP than that on the side where FACL was performed alone (P < 0.05) as documented by Kar and Raj.[12]
| Study | Materials and methods | Results |
|---|---|---|
| Present study, split-face study, 30 patients, four sessions at monthly interval | FACL (Sellas Cis F1-Fractional CO2) along with intradermal PRP (study side) versus FACL along with intradermal saline injections (control side) | Statistically significant difference between two sides after fourth session. Mean percentage improvement in G and B AQGS after four sessions on the study side (33.61%) was more as compared to the control side (26.94%). Side effects such as edema, dryness, and PIH were less on study side |
| Abdel Aal et al.,[4] split-face trial, 30 patients | FACL + PRP injections versus FACL + normal saline injections | FACL + PRP treated side achieved excellent improvement in 13.3% of the patients, whereas there was no excellent improvement on the other side |
| Shah et al.,[5] split-face study, 30 patients, four sessions at 4-week interval | FACL (Unixel Geosmatic) + PRP injections versus FACL + normal saline injections | Better reduction in acne scars on the side treated with FACL in combination with PRP. Higher proportion of side effects such as pain, persistent erythema, and edema reported on the side treated with FACL alone |
| Faghihi et al.,[9] split-face trial, 16 patients, two sessions at 4-week interval | FACL (Q-ray, Diosis, Seoul, Korea) + PRP injections versus FACL + normal saline injections | No statistical significant difference was seen between two sides. Side effects (erythema and edema) lasted longer and were more severe when FACL was combined with PRP |
| Galal et al.,[11] split-face study, 30 patients | FACL versus FACL + PRP: Image analysis system evaluation | Skin analysis camera system revealed combination achieved better results |
| Kar and Raj[12] split-face trial, 30 patients, three sessions at 4-week interval | FACL (30-W FIRE-XEL ablative FCL device) and FACL + topical PRP on right and left sides of the face, respectively | Significant improvement on both sides of the face but the difference was not statistically significant (P = 0.2891). Lesser side effects such as pain, erythema, and edema on FACL + PRP (left) side as compared to the FACL-only (right) side |
Of 30 patients, post inflammatory hyperpigmentation was reported in 16 patients (53.33%). Incidence of PIH was more on the control side (33.3% patients) than that on the study side (20% patients), though the difference was not statistically significant (P = 0.243). In a study by Shah et al.,[5] PIH was seen in 10 (33.33%) patients with higher proportion of them belonging to the control side (20%) than that to the study side (13.3% patients). Incidence of PIH as high as 68% has been reported after laser resurfacing.[13] Other delayed side effect reported in this study was acne Figures 4 and 5 aggravation, which was seen in 26.6% patients on the control side and in 16.6% patients on the study side. In a study by Shah et al.,[5] acneiform eruptions were seen in 10% patients over the study side and in 26.6% patients over the control side. In none of the patients, acneiform eruptions were reported by Faghihi et al.[9] This study did not find any difference in the incidence of milia between the study and control side, over both sides, it was reported in 10% patients.

- Left half of patient’s face. (A) Baseline. (B) After four sessions. (C) On follow-up after 2 months

- (A) Left half of patient’s face showing erythema after FACL. (B) Right half of patient’s face showing scabbing after treatment
Study limitations: The limitations of our study include short follow-up, as scar improvement is better judged 6 months after treatment, single nonblinded assessor, and more objective methods to measure improvement in acne scars.
CONCLUSION
To conclude, there is no single proven modality for the effective treatment of post-acne scars. Combination of various modalities is often needed to meet the desired outcomes. Combination of FACL with newer adjuvants such as PRP has definitive role in managing post-acne scars with lesser side effects than FACL alone. Growth factors in PRP give favorable immediate results in terms of scar remodeling and facial rejuvenation. However, FACL has long-lasting effects on collagen remodeling even after completion of treatment sessions in patients with post-acne scars.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Hypertrophic scars and keloids: A review of their pathophysiology, risk factors, and therapeutic management. Dermatol Surg. 2009;35:171-81.
- [Google Scholar]
- Effective treatments of atrophic acne scars. J Clin Aesthet Dermatol. 2015;8:33-40.
- [Google Scholar]
- Evaluation of autologous platelet-rich plasma plus ablative carbon dioxide fractional laser in the treatment of acne scars. J Cosmet Laser Ther. 2018;20:106-13.
- [Google Scholar]
- Study of safety and efficacy of autologous platelet rich plasma combined with fractional CO2 laser in the treatment of post acne scars: A comparative simultaneous split-face study. Int J Res Med Sci. 2017;5:1344-51.
- [Google Scholar]
- Combination of platelet rich plasma in fractional carbon dioxide laser treatment increased clinical efficacy of for acne scar by enhancement of collagen production and modulation of laser-induced inflammation. Lasers Surg Med. 2018;50:302-10.
- [Google Scholar]
- The efficacy of autologous platelet rich plasma combined with ablative carbon dioxide fractional resurfacing for acne scars: A simultaneous split-face trial. Dermatol Surg. 2011;37:931-8.
- [Google Scholar]
- Can platelet-rich plasma be used for skin rejuvenation? Evaluation of effects of platelet-rich plasma on human dermal fibroblast. Ann Dermatol. 2011;23:424-31.
- [Google Scholar]
- Efficacy of autologous platelet-rich plasma combined with fractional ablative carbon dioxide resurfacing laser in treatment of facial atrophic acne scars: A split-face randomized clinical trial. Indian J Dermatol Venereol Leprol. 2016;82:162-8.
- [Google Scholar]
- Efficacy and safety of a carbon-dioxide ablative fractional resurfacing device for treatment of atrophic acne scars in Asians. J Am Acad Dermatol. 2010;63:274-83.
- [Google Scholar]
- Fractional CO2 laser versus combined platelet-rich plasma and fractional CO2 laser in treatment of acne scars: Image analysis system evaluation. J Cosmet Dermatol. 2019;18:1665-71.
- [Google Scholar]
- Fractional CO2 laser vs. fractional CO2 with topical platelet-rich plasma in the treatment of acne scars: A split-face comparison trial. J Cutan Aesthet Surg. 2017;10:136-44.
- [Google Scholar]
- Nonablative fractional laser resurfacing in skin of color: Evidence-based review. J Clin Aesthet Dermatol. 2017;10:51-67.
- [Google Scholar]






