Translate this page into:
Utilization of Nonabsorbable (Polyamide Black) Buried Subcutaneous Suture Material in Closure of Elliptical Excision in Various Indications for Better Aesthetic Outcome
Address for correspondence: Dr. Yogesh Manjibhai Bhingaradia, Shivani Skin Care and Cosmetic Clinic, Sarthi Doctor House, Fourth Floor, Hirabag, Varachha Road, Surat 395006, Gujarat, India. E-mail: yogeshbhingradia@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
The aim of this report was to study the effectiveness of nonabsorbable (polyamide black) subcutaneous buried suture (6-0) in elliptical excision of various indications for better outcome of the scar. Clinical data of 155 patients, who underwent nonabsorbable buried subcutaneous closure in elliptical excision for different indications, were collected randomly and analyzed retrospectively. By using a modified Vancouver Scar Scale, which includes an assessment of pliability, the height of scar, vascularity, and pigmentation, all postoperative scars were classified into five categories: excellent, good, moderate, hypertrophic scar, or keloid. A total of 155 patients of elliptical excision with different indications were included in the study. In this study, the male-to-female ratio was 1:2, and patients in the age-group between 10 and 70 years were involved. Of 155 patients, 72% of patients had excellent cosmetic outcome (0 score), 21.29% had good cosmetic outcome (1 score), and 2.58% had a moderate cosmetic outcome (2 score) without any hypertrophic scar or keloid by using a modified Vancouver Scar Scale. No complaints were reported during the study. Scar closure by nonabsorbable buried subcutaneous suture will reduce cutaneous tension, so there will be a better approximation of wound edges and thus better outcome of the scar.
Keywords
Better cosmetic outcome
elliptical excision
nonabsorbable subcutaneous closure
BRIEF REPORT
Once a scar is formed it may last forever; it cannot be removed totally, but it can be modified to look better both functionally and aesthetically with combination of therapeutic modalities. People with abnormal skin scarring may face physical, psychological, aesthetic, and social consequences that may be associated with substantial emotional and financial costs.[123456]
Clinical data from 155 patients of elliptical excision with different indications were collected randomly and analyzed retrospectively. This study was conducted among patients attending dermatology outpatient department from April 2016 to January 2019. Patients in the age-group between 10 and 70 years were involved regardless of gender bias. Notably, history, general physical examination, thorough dermatological survey, and preoperative investigations (complete blood count, urine routine microscopy, random blood sugar, human immunodeficiency virus [HIV], and Hepatitis B surface antigen [HbsAg]) were performed. Statistical data were presented as percentage.
Before the beginning of the study, patient’s consent and photographs were taken. Photographs were captured at the following visits: First visit, seventh day of the procedure after suture removal, and at the end of 1 month and 3 months for the assessment of scar. At the end of third month, scar assessment was carried out by using a modified Vancouver Scar Scale.
MODIFIED VANCOUVER SCAR SCALE
-
Pigmentation:
0 = normal
1 = hypopigmentation
2 = mixed pigmentation
3 = hyperpigmentation
-
Vascularity:
0 = normal
1 = pink
2 = red
3 = purple
-
Pliability:
0 = normal
1 = supple—flexible with minimal resistance
2 = yielding—giving way to pressure
3 = firm—inflexible, not easily moved, resistant to manual pressure
4 = banding—ropelike tissue that blanches with extension of scar
5 = contracture—permanent shortening of scar producing deformity or distortion
-
Height:
0 = normal–flat
1 = >0–1 mm
2 = >1–2 mm
3 = >2–4 mm
4 = >4–mm
Total score = 15
Figures 1–5 show pretreatment and posttreatment view of various dermatological indications. Total data of 163 patients were collected, who underwent elliptical excision for various indications, among which eight patients did not come for follow-up visit after 7 days owing to their residence in other city, and suture removal was carried out in their hometown. Male-to-female ratio was 1:2 in our study. Table 1 shows the distribution of cases as per the modified Vancouver Scar Scale scoring system at the end of third month.
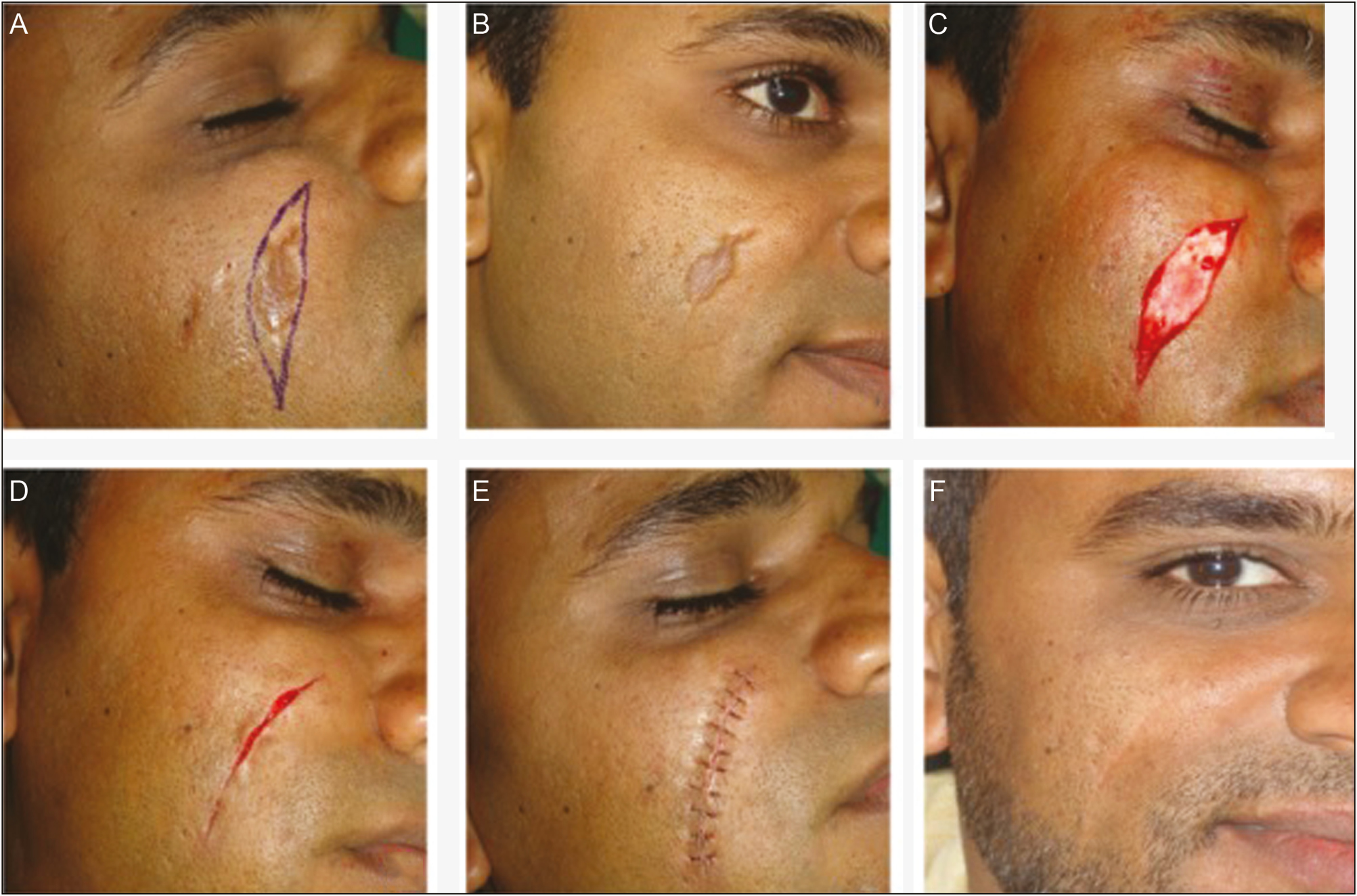
- (A) Pretreatment view of posttraumatic scar. (B) Planned direction of excision. (C) Excision of scar. (D) Subcutaneous nonabsorbable buried suture. (E) Cutaneous vertical mattress suture. (F) Cosmetic improvement in after surgical view

- (A) Post chicken pox scar. (B) Vertical mattress suture after excision. (C) Suture removal on seventh day. (D) After surgical view
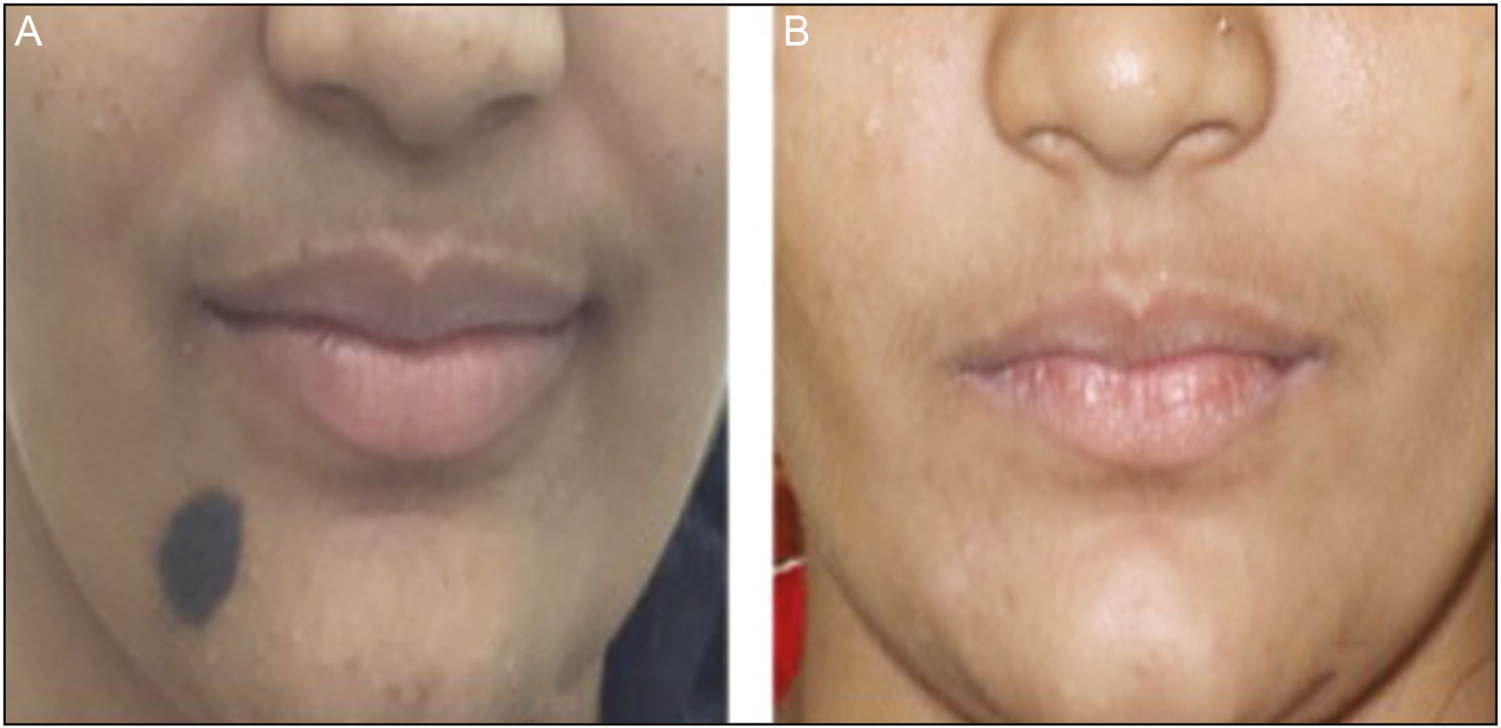
- (A) Congenital melanocytic nevus, pretreatment. (B) After surgical appearance
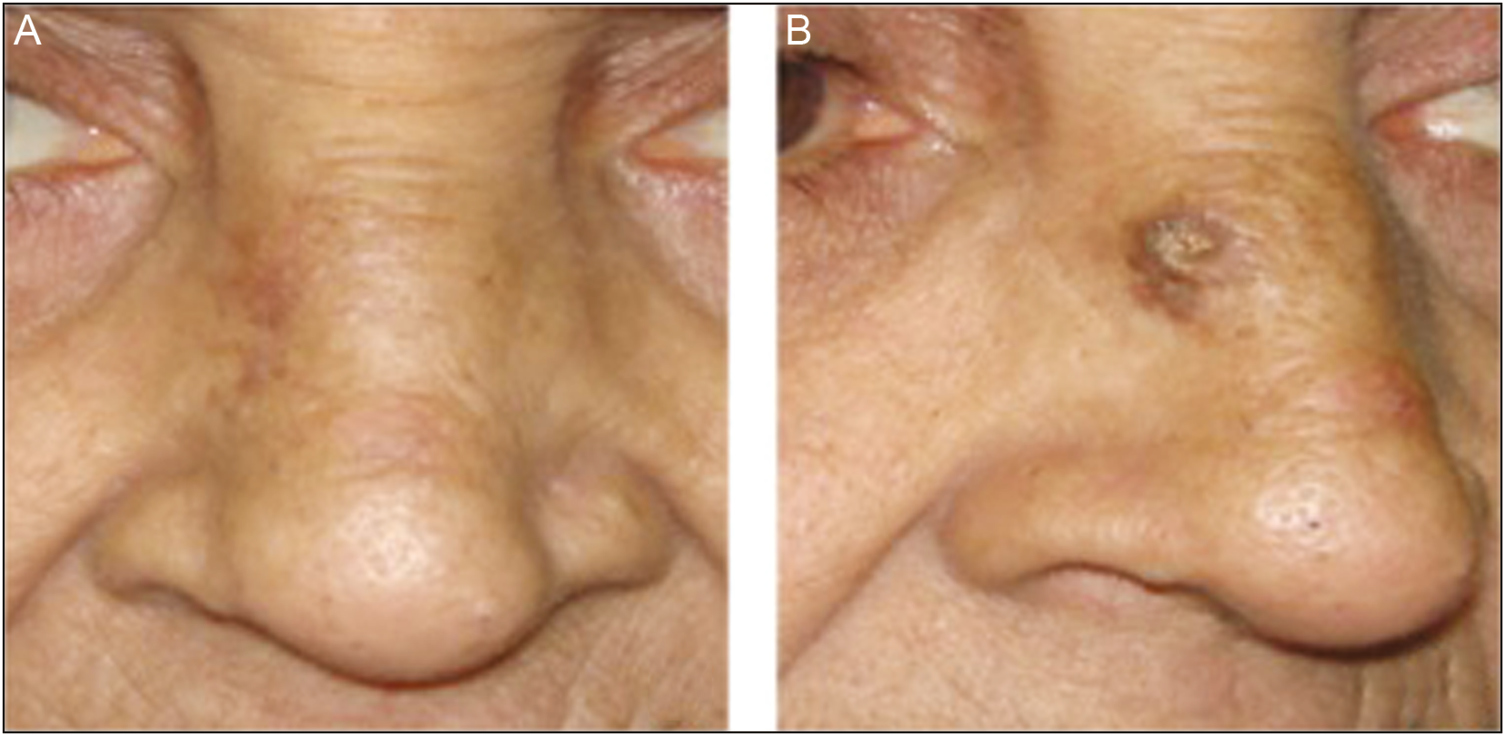
- (A) Before treatment, keratoacanthoma. (B) After surgery
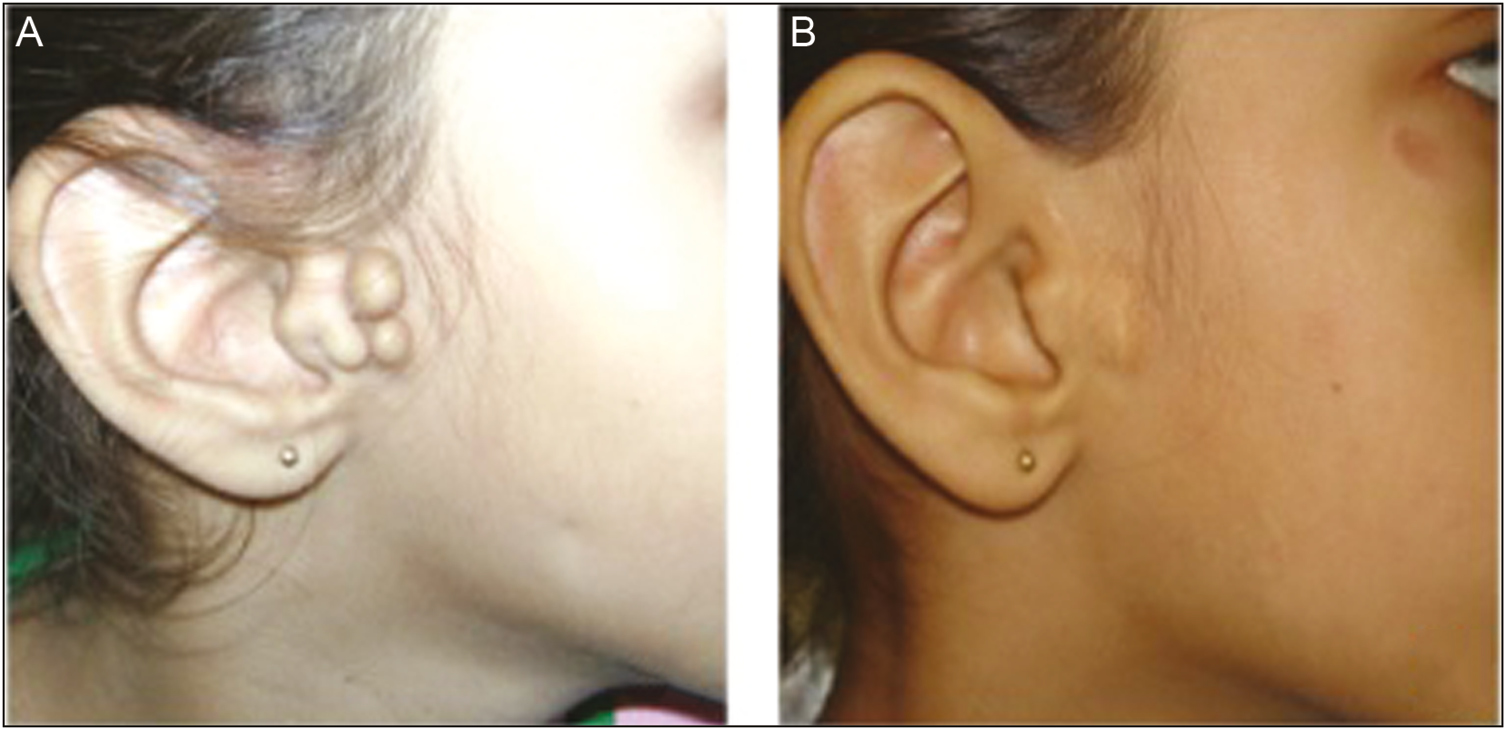
- (A) Accessory tragus before treatment (B) After surgical cosmesis
| Total score of 15 | N (%) |
|---|---|
| 0, excellent | 112 (72) |
| 1, good | 33 (21.29) |
| 2, moderate | 4 (2.58) |
| 3, minimum | 6 (3.87) |
Table 2 shows the number of participants as per the modified Vancouver Scar Scale scoring system at the end of third month for various dermatological indications. In our study, we found excellent improvement (0 scales) in the modified Vancouver Scar Scale in most of the indications for elliptical excision with using nonabsorbable buried sutures. Approximately, 82.60% of patients with compound nevus got 0 scale, that is, almost invisible scar at the end of 3 months. Approximately, 56.86% of posttraumatic scar patients got 0 score, which is quiet appreciable, likewise 88.88% of patients with junctional nevus, 50% of tattoo removal patients, 70% of patients with congenital melanocytic nevus, 100% of patients with seborrheic keratosis, 66.66% of patients with accessory tragus, and 100% of patients with keratoacanthoma got 0 score in this study. Apart from these, no complaint was reported during the study period.
| Indication | Total (N = 155) | Score 0 (excellent) N (%) | Score 1 (good) N (%) | Score 2 (moderate) N (%) | Score 3 (minimum) N (%) | Score 4–15 (poor) N (%) | |
|---|---|---|---|---|---|---|---|
| 1 | Compound nevus | 69 | 57 (82.60) | 11 (16.94) | 0 | 1 (1.44) | -- |
| 2 | Posttraumatic scar | 51 | 29 (56.86) | 15 (29.41) | 3 (5.88) | 4 (7.84) | -- |
| 3 | Junctional nevus | 9 | 8 (88.88) | 1 (11.11) | -- | -- | -- |
| 4 | Tattoo removal | 6 | 3 (50) | 3 (50) | -- | -- | -- |
| 5 | Basal cell carcinoma | 1 | -- | 1 (100) | -- | -- | -- |
| 6 | CMN | 10 | 7 (70) | 1 (10) | 1 (10) | 1 (10) | -- |
| 7 | Seborrheic keratosis | 3 | 3 (100) | -- | -- | -- | -- |
| 8 | Accessory tragus | 3 | 2 (66.66) | 1 (33.33) | -- | -- | -- |
| 9 | Keratoacanthoma | 3 | 3 (100) | -- | -- | -- | -- |
CMN = congenital melanocytic nevus
For better outcome of the scar, it is important to reduce tension over cutaneous stitches, which are achieved by subcutaneous wound closure by nonabsorbable (polyamide black) buried interrupted suture (6-0), and cutaneous closure by nonabsorbable suture in vertical mattress pattern, which needs to be removed on seventh day. Nonabsorbable suture material is preferable, because it is easier to tie, it is unlikely to break prematurely, and it elicits a minimal inflammatory response. Subcutaneous buried sutures do not require its removal and, it remains as it is at its location for a lifetime.[78910111213] In a recent study with rat models, Tomida et al.[14] postulated that the subcutaneous introduction of polypropylene does not produce pronounced foreign body reactions. Proper approximation of wound edges is crucial to reduce wound gap and for better cosmetic appearance of the scar. Complications such as hematoma, dehiscence, wound gap, unaesthetic scar, and indentation mark and dog-ear formation can be prevented by subcutaneous closure.
In conclusion, utilization of absorbable suture material in subcutaneous layer for strengthening the tissue can give tensile strength for 10–12 days only, and gradually it gives tension over healed tissue and it gives appearance of railroad track pattern scar, whereas, utilization of nonabsorbable buried suture subcutaneously gives strength to the subcutaneous tissue and it lasts for a lifetime and avoids widening of tissue and ultimately avoids the appearance of railroad track scar or visible fibrotic scar. As expected, nonabsorbable subcutaneous closure in elliptical excision is carried out to reduce skin tension and for better outcome of scar.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Elliptical or fusiform excision and its variations. In: Textbook of dermatosurgery and cosmetology (2nd ed). Mumbai, India: ASCAD; 2005.
- [Google Scholar]
- Textbook of cutaneous and aesthetic surgery :285-9.
- Proper planning and execution of surgical excisions. In: Wheeland RD, ed. Cutaneous surgery. Philadelphia: W.B. Saunders Company; 1994.
- [Google Scholar]
- Cold steel surgery. In: Lask GP, Moy RL, eds. The ellipse, principles and techniques of cutaneous surgery (1st ed). New Delhi: Jaypee Brothers Publishers; 1996.
- [Google Scholar]
- Subcutaneous non-absorbable polypropylene (SNAP) sutures in serial excision of congenital naevi: a new time-saving technique reducing dehiscence with optimized aesthetic results. J Eur Acad Dermatol Venereol. 2016;30:533-5.
- [Google Scholar]
- Comparison of absorbable with nonabsorbable sutures in closure of facial skin wounds. Arch Facial Plast Surg. 2003;5:488-90.
- [Google Scholar]
- Suturing techniques. In: Lask GP, Moy RL, eds. Principles and techniques of cutaneous surgery. 1996.
- [Google Scholar]
- Suture materials for closing the skin and subcutaneous tissues. Aesthetic Plast Surg. 1986;10:245-8.
- [Google Scholar]
- Comparative examination of subcutaneous tissue reaction to high molecular materials in medical use. Eur J Med Res. 2011;16:249-52.
- [Google Scholar]






