Translate this page into:
Multimodality Surgical Treatment Approach to Acne Keloidalis Nuchae Based on Lesion Morphology
Address for correspondence: Dr. Sruthi Kareddy, Department of Dermatosurgery, Cutis Academy of Cutaneous Sciences, 5/1, 4th Main, MRCR Layout, Govindaraja Nagar Ward, Vijayanagar, Bengaluru, Karnataka, India-560040. E-mail: sruthikareddy261@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Acne keloidalis nuchae (AKN) correctly termed “folliculitis keloidalis”, is an unusual form of chronic folliculitis and cicatricial alopecia that affects nape of neck. AKN can lead to significant scarring with tumor like masses and alopecia. Treatment in chronic cases is challenging with recurrence being common. Several modalities are being tried with variable success. We aim to report our experience with multimodality surgical approach. Five patients of chronic AKN refractory to intralesional steroids were treated between 2015 - 2018 with (1) excision and primary closure or (2) punch excision followed by healing with secondary intention or (3) intralesional cryotherapy, based on lesion morphology, site and extent . All patients also underwent long-pulsed (LP) neodymium-doped yttrium aluminum garnet (Nd:YAG)laser hair removal for the affected part with an aim to prevent new lesions from developing in the surrounding area. Patients were followed at regular intervals till 6 months. 100% patients were satisfied with the treatment outcome. They showed 80%–90% overall reduction in lesions with satisfactory cosmetic outcome. Complete removal of follicles leads to least chance of local recurrence. Surgical excision remains the most effective modality of management. In case of lesions <5 mm, punch excision can be gratifying. Cryotherapy is useful where excision and primary closure is not feasible. Hair removal lasers can prevent new lesions in the sorrounding area. Combined multimodality approach tailored to the type of lesions gives maximal result with a better cosmetic outcome.
Keywords
Acne keloidalis
cryotherapy
laser hair reduction
morphology
multimodality
surgical
INTRODUCTION
Acne keloidalis nuchae (AKN), rather folliculitis keloidalis, is a form a persistent folliculitis that affects the nape of the neck. It is more common in postpubertal men. Chronic cases can manifest as papules, nodules, tumorous plaques, and scarring alopecia. Recurrence is very common and is troublesome. For the patients, the presence of keloidal lesions is more worrisome than alopecia.
Innovative approach is required to treat this chronic condition with relapses. Treatment is best directed as per the morphology, site, and size of lesions.
We aimed to report the outcomes of resistant AKN treated with multimodality approach (elliptical excision, punch excision, cryotherapy, intralesional steroid [ILS] injections, and laser hair removal).
CASE REPORTS
Five patients of chronic AKN refractory to intralesional steroids were treated with our surgical multimodality approach during 2015-2018. Informed written consent was obtained from all patients.
Patient 1 had several papules grouped over a rectangular area of 9 × 2.5 cm. A standard ellipse was taken in 4:1 ratio to include most of the lesions. Incision was placed up to subcutaneous level so as to removal the hair follicles in toto. Wound was closed with primary intention using simple interrupted sutures. Resultant scar was thin and cosmetically acceptable, easily camouflaged by overlying hair. Remaining outlying papules were punch excised and left to heal by secondary intention [Figure 1]. There was no recurrence at 6 months.

- (A) Multiple lesions along posterior hair line. (B) 4:1 elliptical excision. Arrows showing few outlying papules, which were punch excised after 4 weeks. (C) Cosmetically pleasing scar with excellent improvement at 6 months
Patient 2 had two plaques (3.5 × 2.5 cm), one on either side of lower occipital crease. Combined width was >3 cm, making elliptical excision and primary closure difficult. The upper one was excised and closed primarily. The lower lesion was ablated with CO2 laser and left for secondary intention healing. The laser ablation was probably not deep enough to destroy all the hair follicles, and at 6 weeks after procedure, there were few recurrent papules. The patient was started on oral isotretinoin 20mg daily. He patient was lost to further follow-up [Figure 2].

- (A) Two plaques above and below the lower occipital crease. (B) 6 weeks post CO2 ablation of lower plaque (encircled area) showing recurrence. Patient was lost to follow-up
Patient 3 had a very large thick plaque over neck 17 × 6 cm in size. Not much improvement was noticed after several sessions of surface cryotherapy and ILS injection. Following four sessions of intralesional cryotherapy (once in 3 weeks), there was significant reduction in the bulk of tissue. Hair follicles, which did not respond to laser hair reduction due to thickened surrounding tissue, were punch excised [Figure 3].

- (A) Large plaque over nape of neck. (B) and (C) Good improvement with four sessions of intralesional cryotherapy, intralesional steroid injections followed by laser hair removal. Circles show few hairs, which did not respond to laser reduction, and were punch excised
Patient 4 had wide thin plaque (6 × 4 cm) over posterior hair line, which responded to multiple sessions of surface cryotherapy and ILS injection. He was also given oral isotretinoin 20mg daily for 3 months as he had active lesions also at the time of presentation. Few tufted hair follicles were punch excised as they did not respond to neodymium-doped yttrium aluminum garnet (Nd:YAG) laser hair removal.
Patient 5 had tumorous plaque (3 × 2 cm) just above posterior hairline. Lesion was excised in toto using an elliptical excision and was closed with simple interrupted sutures leaving a linear scar.
All five patients underwent laser hair reduction with Nd:YAG laser (four sessions 4 weeks apart) from the posterior hair margin till the maximum extent of the lesions and intervening area. Laser was started 4 weeks post surgery/cryotherapy. Three weekly ILS injections for 3 months were also given for leftover papules, which could not be punch excised. All patients were under regular follow-up till 6 months except Patient 2 who was lost at 2 months to follow-up.
All patients were satisfied with the treatment outcome, and the resultant scarring was acceptable to them. No recurrence was observed at 6 months, barring a few papules in two patients.
Long-term follow-up of 2 years in Patient 1 and 3 showed no recurrence.
DISCUSSION
The exact etiology of AKN is unclear, but it might be triggered by chronic irritation or occlusion of the follicles due to haircutting practices, trauma, friction, heat, or humidity.[1]
AKN is a troublesome recurrent disorder, and it requires a multimodal approach. It is not a true keloid and is most likely a chronic inflammatory process to hair fragments.[2] Histopathology studies have shown that initially there is an inflammatory process around the infundibulum and isthmus. This probably weakens the follicular wall with exposure of hair leading to a foreign body response. In chronic lesions, dermis shows hair fragments with inflammatory infiltrate.[3]
A meta-analysis suggests that only a few case reports exist regarding the management of chronic cases. Till date most evidence lies in complete surgical excision. However, recurrences have also been reported post surgery.[2]
With laser hair reduction, the hair becomes thinner and softer, it loses its strength to penetrate the skin, and the number of new eruptions decrease. Hair fragments in the dermis are destroyed, removing the perpetuating stimulus for inflammation in existing lesions. In addition, laser helps in reducing inflammatory process by reducing vascularity.[45] Long-pulsed Nd:YAG can destroy remnants of hair situated deeper as it has the longest wavelength among all the hair reduction lasers. However, even this laser cannot destroy hair that is buried inside thick nodules and plaques of AKN. Hence, we propose that in such lesions surgical removal/destruction of the lesion including all the hair fragments and follicles is essential. Laser here helps in preventing recurrences in the surrounding area.
Scarring is a concern with surgical approach, though use of a horizontal ellipse encompassing the posterior hairline results in excellent cosmesis by allowing the surgical scar to be hidden in the newly formed hairline. Small papular lesions are best excised using a punch and left to heal by secondary intention, especially when they are few and scattered. It is also simple and useful to remove outlying papules, which cannot be included in the ellipse that is excised.
Surgical excision with secondary intention healing though effective has a prolonged downtime. Hence, where primary closure is not feasible cryotherapy is a good option. When the lesion is less than 0.5 cm thick surface therapy should be done. Intralesional cryotherapy is a good option for thicker lesions.
CONCLUSION
Surgical excision remains the most effective modality of management. Complete removal of follicles leads to least chance of recurrence. In case of papulo-nodular lesions <5 mm, punch excision can be gratifying. In lesions, which cannot be excised, and closed primarily, cryotherapy (surface and intralesional) is the best option. Hair removal with Nd:YAG is helpful in preventing new lesions. Combined multimodality approach tailored to the grade of lesions gives maximal result with a better cosmetic outcome [Figure 4].
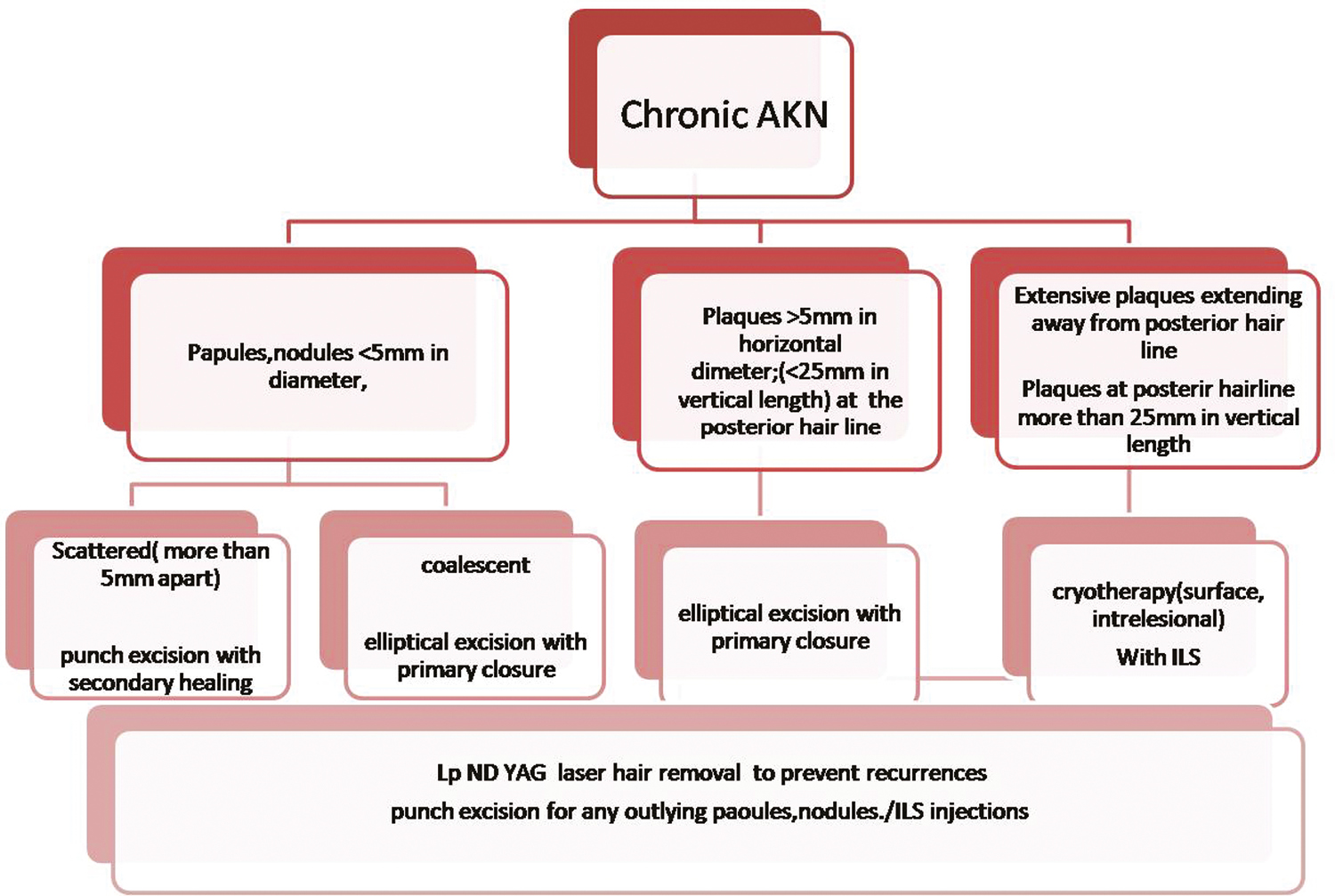
- Proposed surgical management of chronic AKN
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Acne keloidalis nuchae: prevalence, impact, and management challenges. Clin Cosmet Investig Dermatol. 2016;9:483-9.
- [Google Scholar]
- Treatment of acne keloidalis nuchae: a systematic review of the literature. Dermatol Ther (Heidelb). 2016;6:363-78.
- [Google Scholar]
- Histologic features of alopecias: part II: scarring alopecias. Actas Dermosifiliogr. 2015;106:260-70.
- [Google Scholar]
- Efficacy of diode laser for treating acne keloidalis nuchae. Indian J Dermatol Venereol Leprol. 2005;71:31-4.
- [Google Scholar]
- The efficacy of laser-assisted hair removal in the treatment of acne keloidalis nuchae; a pilot study. Eur J Dermatol. 2012;22:645-50.
- [Google Scholar]






