Translate this page into:
Revisiting Rhombic Flaps for Aesthetic Facial Resurfacing: Addressing a Surgical Conundrum
Address for correspondence: Dr. Neeraj Kant Agrawal, 704, Rudra Samriddhi, Bhagwanpur, Behind Trauma Centre, Varanasi, Uttar Pradesh, India. E-mail: agrawalnk@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Facial resurfacing is a surgical and aesthetic challenge, as it requires soft, pliable, and stretchable donor skin with a good match of color, texture, and thickness and minimum donor scarring. Rhombic flap is a highly versatile flap that has the aforementioned properties. Careful flap planning and execution is vital for successful outcomes.
Aims:
The aim of this work was to study the geometry of the classic rhombic flaps; to evaluate their versatility and technical finesse as well as their application to resurface defects over various regions of the face.
Materials and Methods:
Overall, 42 patients with facial scars due to trauma, malignancies, small nevi, and mature scars of the face were studied and operated on. Of the four rhombic flaps that were possible, choosing the best option required careful attention to camouflage of scar and proximity to vital deformable anatomical structures. Geometrical planning of the flap was the essence of the entire surgical exercise.
Results:
Outcome of rhombic flaps were meticulously and critically analyzed. The study consisted of 36 females (85.71%) and only 6 males with a mean age of 23 years. Defects were created on 27 mature scars (64.29%) and 11 burn scars (26.19%). Defects over the cheek and lateral canthus of the eye were especially problematic. It is a safe flap with excellent results as far as visible scarring and traction deformities are concerned. Scars elsewhere on the face fared better than on the bony prominence.
Conclusion and Significance:
Rhombic flaps offer an excellent alternative to resurface facial scars and defects in a selected subset of patients.
Keywords
Facial resurfacing
facial scars
geometry rhombus
lines of maximum extensibility
rhombic flaps
INTRODUCTION
Alexander Limberg worked extensively to design a rhomboid flap, and the preliminary work was published first in 1928;[1] however, it was Limberg’s landmark work in 1946[2] that unfolded yet another option for resurfacing facial defects. Aesthetic facial reconstruction, a surgical challenge, was made possible by the simple yet versatile rhombic flap.[3] The vital criteria for an ideal flap is soft, pliable, and stretchable donor skin with a perfect color match, similar texture, and adequate thickness. The rhombic flap reliably fulfils these criteria. Vital anatomical structures and landmarks should be taken care of lest they get deformed. Poor reconstructive techniques can cause or exacerbate significant deformities, especially in the oral and ocular regions.[4] Other aesthetic landmarks that merit due attention are philtrum, eyebrows, eyelids, canthi, hairline, and earlobes. Traditional transposition, advancement, and rotation flaps are other options that have clinical limitations owing to their dimensions and gross encroachment of anatomical boundaries. Being random-pattern cutaneous flaps, the rhombic flaps are safe as far as viability is concerned. They are precisely geometric, and a thorough knowledge of the anatomical principles helps to plan and execute them accurately. They have mainly found usefulness in small- to medium-sized defects over different regions of the face. Therefore, this can be understood as a versatile addition to the armamentarium of a plastic surgeon, which provides a precise mathematical design for closure of both the primary and the secondary (donor) defect.
This study was designed to investigate the geometry of the ideal rhombic flap, to evaluate the versatility of rhombic flaps, and to discuss the finer technical details and their application to resurface defects over various regions of the face.
MATERIALS AND METHODS
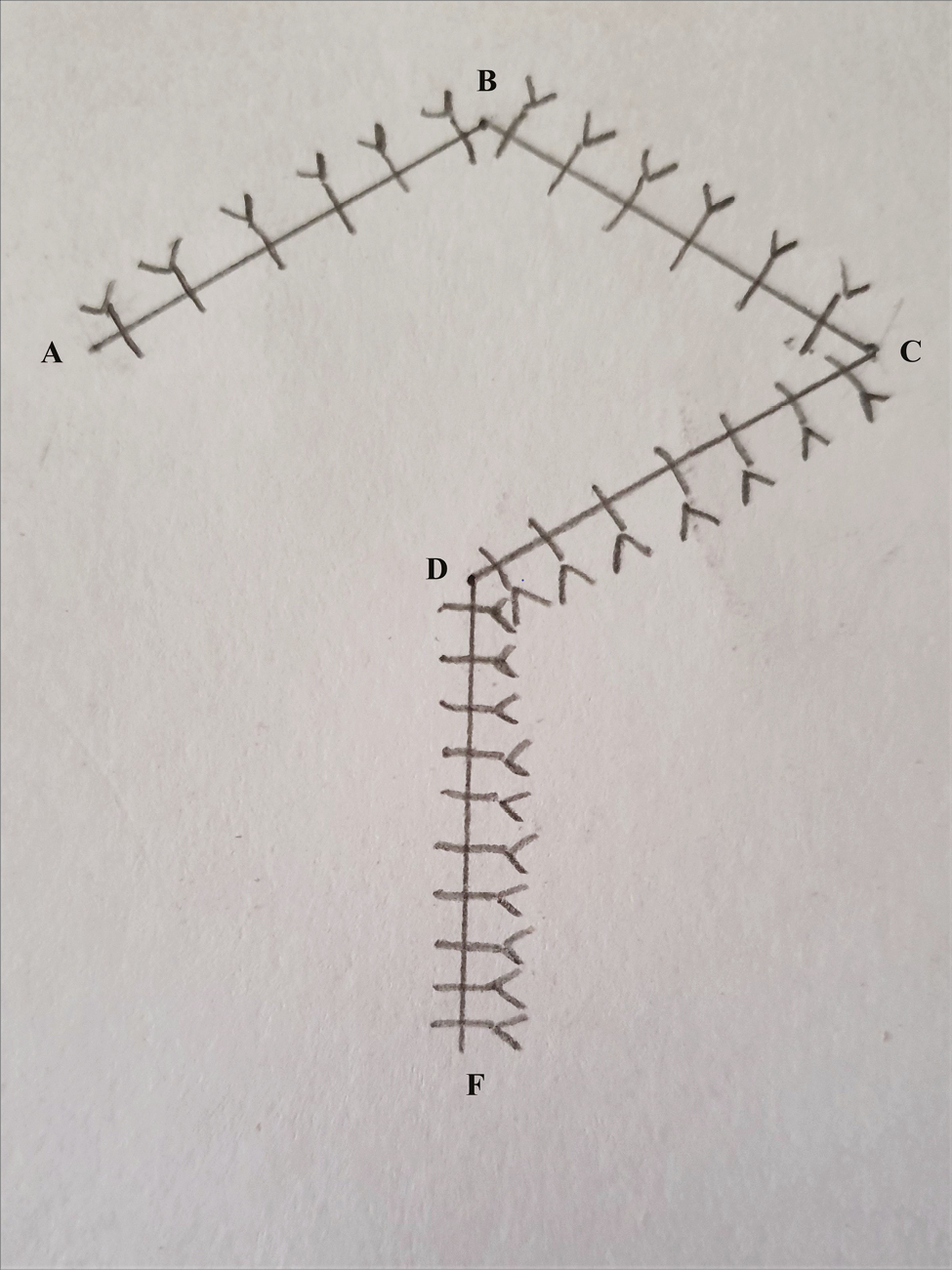
This prospective study was conducted on 42 patients with iatrogenic cutaneous defects over various anatomical regions of the face managed by rhombic flaps. This was carried out from May 2016 to November 2019 in the department of Plastic Surgery, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh, India. Facial plastic surgery was avoided in patients younger than 10 years, as they had inconsistent perception and description of pain and were likely to damage the sutures. Strict vigilance was warranted in psychiatric patients, as psychiatric disorders were considered one of the predictors of poor outcome in cosmetic plastic surgery and it was considered best to exclude them from the study. Patients with uncontrolled diabetes and scleroderma, which usually results in tightening of the facial skin, were also excluded from the study. In the preoperative visits, dimensions of the scars or defects, anatomy and availability of donor tissue, mobility and pliability of the donor tissue, and direction and camouflage of the final scar and its bearing on the vital anatomical landmarks and apertures were evaluated. When planning a reconstruction, every rhombus could be closed with four possible flaps [Figure 1] and only one distinct flap was borrowed from the donor site that had the greatest relative laxity. The outcome depended on the appropriate positioning of the defect and on proper flap choice. The patients were assessed by age, etiology, location and size of the defect, and, if any, postoperative complications.
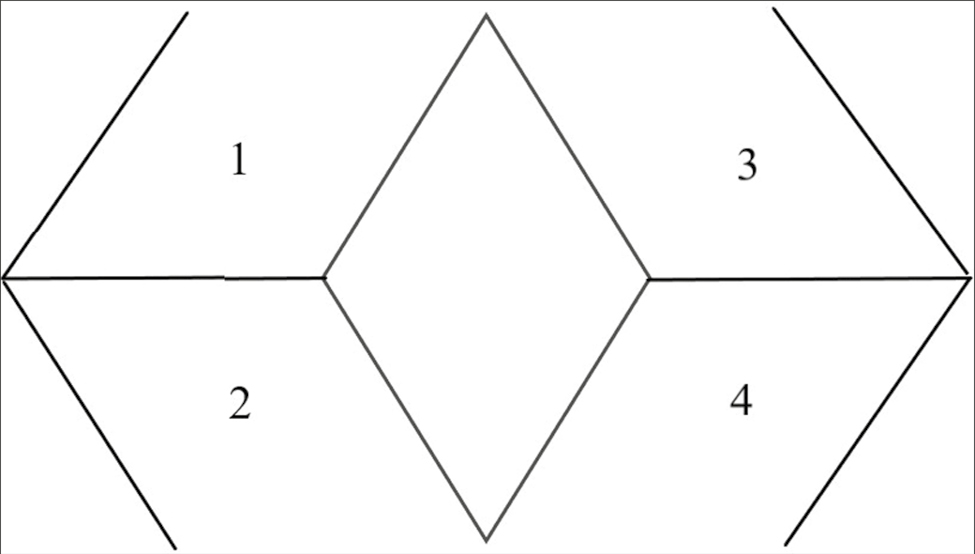
- Four possible options of a rhombic flap to resurface a rhomboid defect based on the two short diagonals of the rhombus
Design of the flap
Rhombic flaps were found to be applicable to defects that were shaped like a rhomboid with angles of 60° and 120°, which were also called 60° rhomboid defects.[5] It may be considered as two equilateral triangles with a common base known as a short diagonal of the rhombus [BD in Figure 2]. Rhombic flaps used tissue adjacent to the defect to enable primary closure of the donor site. The flaps were designed in continuity with the defect in such a manner that they share one side of the defect [AD of the rhomboid defect and ADˊ of the rhombic flap in Figure 2]. Irregular, circular, or oval defects were also converted into a rhomboid with special care to avoid excision of excess tissue without distorting the vital anatomical landmarks. At least two sides of the rhombus should lie along lines of maximum extensibility (LME) [Figure 3]. These lines were described as lying at a right angle to Langer’s line, which was identified by pinching the facial skin between the thumb and the index finger[6] The length of all sides and that of the short diagonal were described as being the same [Figure 2]. When possible, the short diagonal was marked along the LME. Brobyn et al.[7] suggested that the line of closure of the donor site (the line of maximum tension of the completed procedure) should be placed in an LME of the face, if possible.
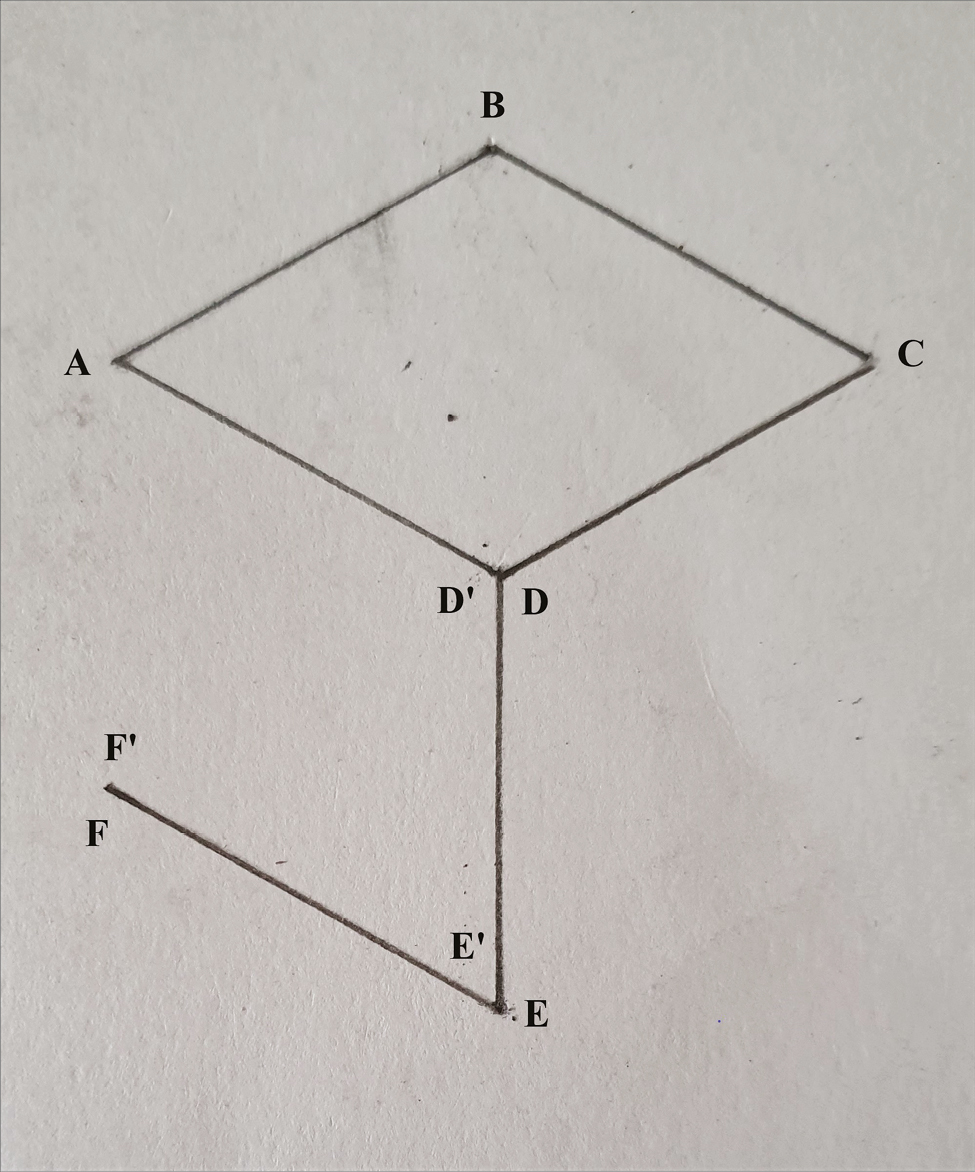
- Diagram showing a skin defect shaped like a 60° rhombus ABCD with a short diagonal BD. It also shows a rhombic flap AD′E′F′. AB = BC = CD = DA = BD = DˊEˊ = EˊFˊ. DˊEˊFˊ are the corresponding points of the rhombic flap that would be inset into the defect
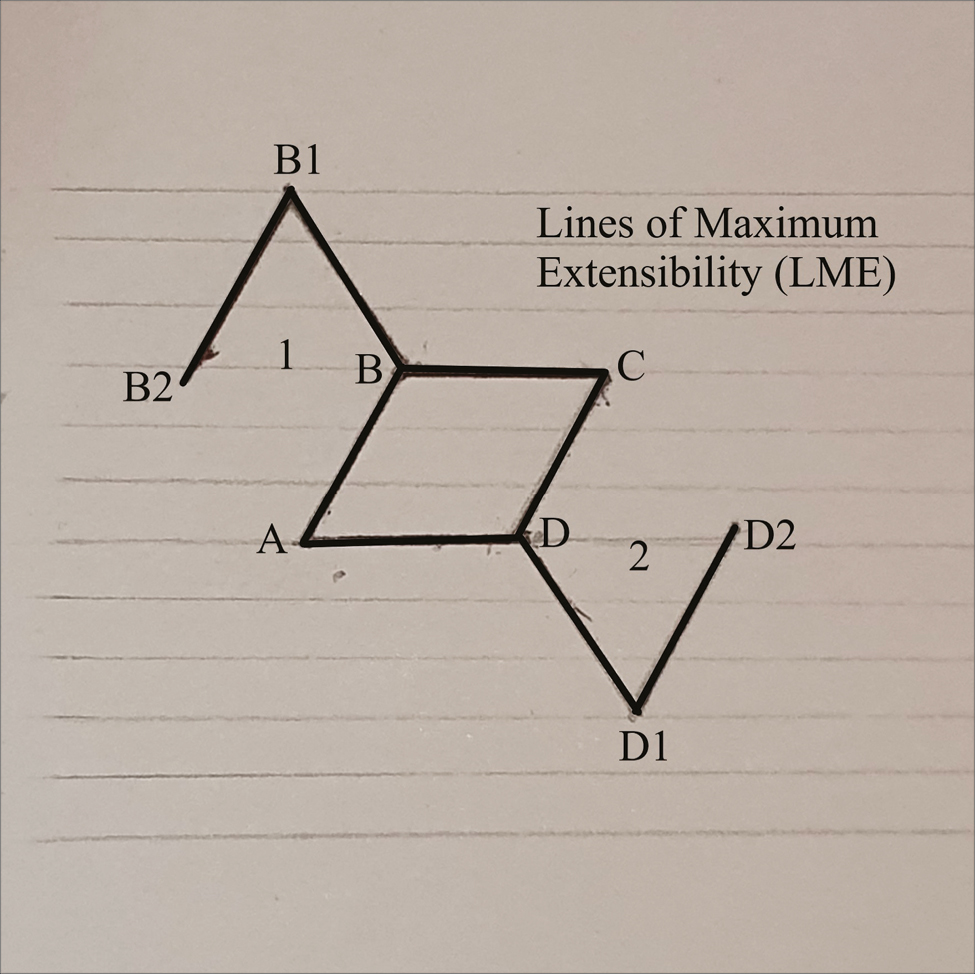
- Diagram depicting the LME with at least two sides of the rhombus lying along LME
Surgical technique
The flap was designed immediately adjacent to the soft-tissue defect, which was shaped as a rhomboid ABCD [Figure 2]. The angles 60° (Δ BCD and Δ BAD) and 120° (Δ ABC and Δ ADC) were subtended in the rhomboid lesion to be excised, The distal end of the flap (D’E’) was sketched as a continuation of the diagonal (BD) of the defect and was equal to the side BC of the defect, as they would oppose each other after transfer [Figure 4]. The far side of the flap (E’F’) was designed parallel to its counterpart (AD’) and was equal in length to side CD of the defect. Line DE was equal to EF, and flap Δ D’E’F’ was planned as 60°. The flap and surrounding tissue were undermined in the subdermal plane. The flap was sutured in layers [Figure 5]. Tension on the suture lines was evaluated and found to be greatest at the donor site. Generous undermining did not change the relative tension distribution at the donor suture line. This line of maximal flap tension or the line of closure of the donor site was placed in an LME of the face. This was performed as per Becker,[8] who described the concept of facial tension. Primary tension of closure must never displace a neighboring structure. Flap planning should avoid distortion of prominent landmarks, such as the eyelid, lip margin, or the nasal ala. Utmost care was taken to respect the boundaries of aesthetic subunits units when designing a flap. Skin color, thickness, and presence/ absence of hair were also taken care of.
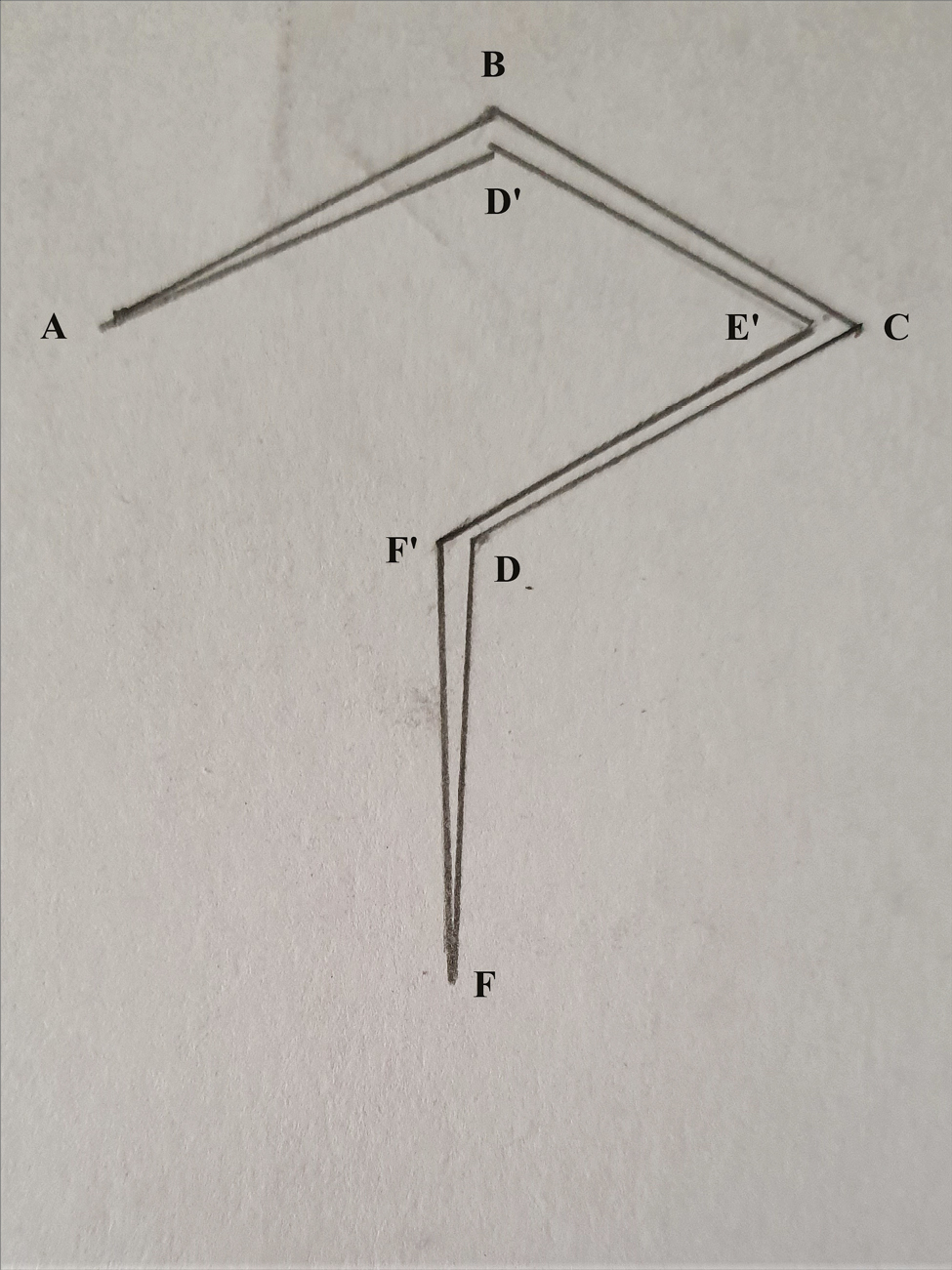
- Rhombic flap ADˊEˊFˊ transposed into the defect. The maximum tension of closure is along the line FˊF
- Rhombic flap sutured
RESULTS
The demographic variables of all the 42 patients were studied in great detail and we found that there were 36 females (85.71%) and only 6 males (14.71%), with a mean age of 23 years (range 16–60 years). The defects were created on 27 mature scars (64.29%), 11 burn scars (26.19%), 2 skin tumors (4.76%), and 2 nevi (4.76%) [Figures 6–9]. The anatomical distribution was diverse [Table 1]. Defects on the cheek [Figures 10–12] and in proximity to the lateral canthus of the eye [Figures 13–15] troubled the patients more and accounted for more than half the number of subjects. The length of sides of the rhombus [AB, BC, CD, AD in Figure 2] and the rhombic flap (AD, DE, EF) were equal as was the short diagonal (BD), the extension of which (DE) was vital in designing the flap. Therefore, the calculation of any one side of the defect would eventually give the remaining dimensions. The mean dimension of a side was found to be 3.26 cm, ranging from 1.7 to 5.6 cm, with the median being 3 cm. Anatomical sites such as lateral canthus of eye, vermilion of the lips, and nasolabial folds had limited adjacent tissue, which obviated the use of calculated rhombic flaps. Numerically, they make 21.4% (9 of 42) of patients. The mean operative time was about 45 minutes. The procedure was performed as an outpatient one under local anesthesia, and most patients returned to work within 1–5 days. There were no major or minor complications, with the flap being a safe flap.

- A 2.6-cm hairy nevus, along the long axis, on the chin of a 16-year-old girl

- Excision of the nevus done with a margin of 1 mm on all sides, making the excision upto 2.8 cm. The nevus was expected to be deep. Limberg flap 2.5 cm planned from the right side of the chin

- Flap sutured in place

- Appearance of the scar 3 months after surgery
| Anatomical location | Number of patients | Percentage (%) |
|---|---|---|
| Cheek (Zone II) | 14 | 33.33 |
| Forehead | 10 | 23.81 |
| Lateral canthus of eye | 8 | 19.05 |
| Cheek (Zone 1) | 6 | 14.29 |
| Chin | 2 | 4.76 |
| Nose | 2 | 4.76 |

- An irregular post-traumatic scar in the suborbital region or Zone I of cheek. It was densely adherent to the underlying right maxilla

- Limberg flap harvested from the preauricular region utilizing the skin laxity. A separate transverse scar also seen separate from the rhombic flap
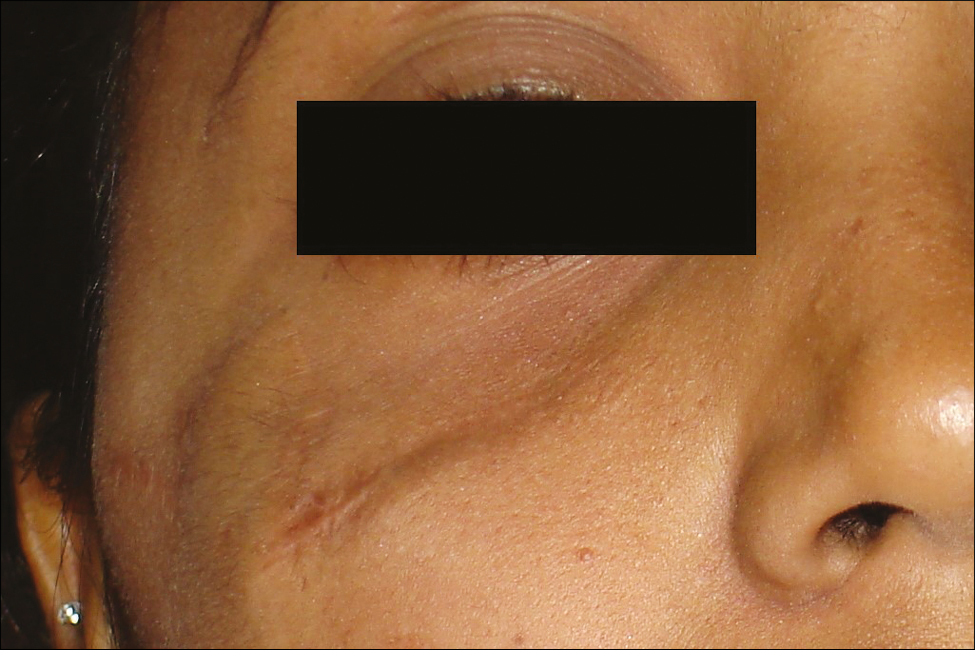
- Appearance of the scar 4 months after surgery. The scar is hardly visible and it can further be modulated by silicon-based gels

- A traumatic scar adjacent to the lateral canthus of the left eye. A 1.8-cm rhombus marked and the best possible rhombic flap also marked
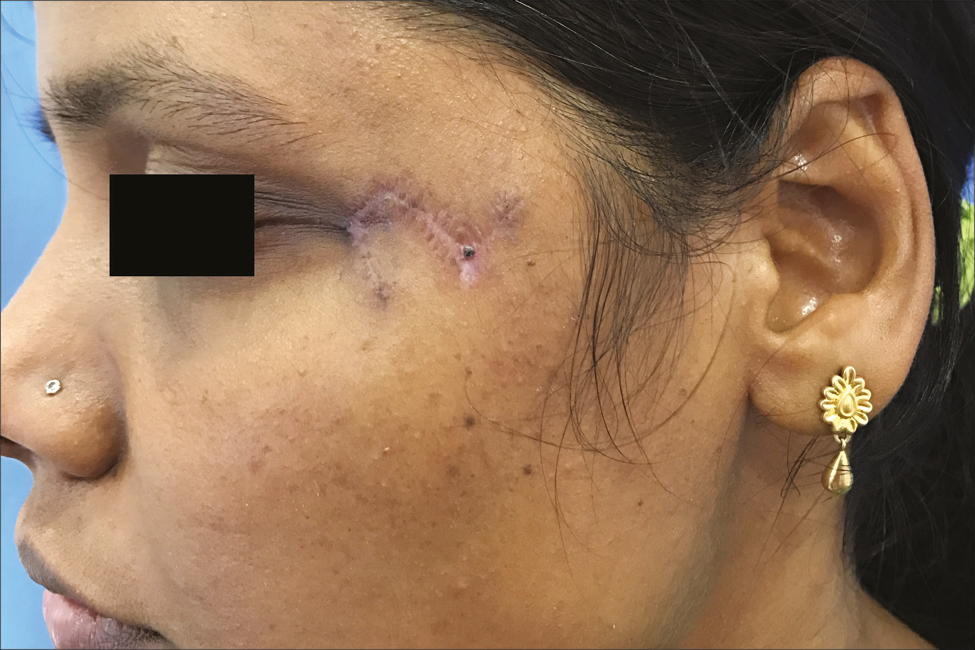
- Three months follow-up showing the improved appearance of the scar. It can be seen that the final scar was lying parallel to the Langer’s lines. Primary closure of such a defect would produce deformity of the lateral canthus. This justifies the use of rhombic flaps in such anatomical sites
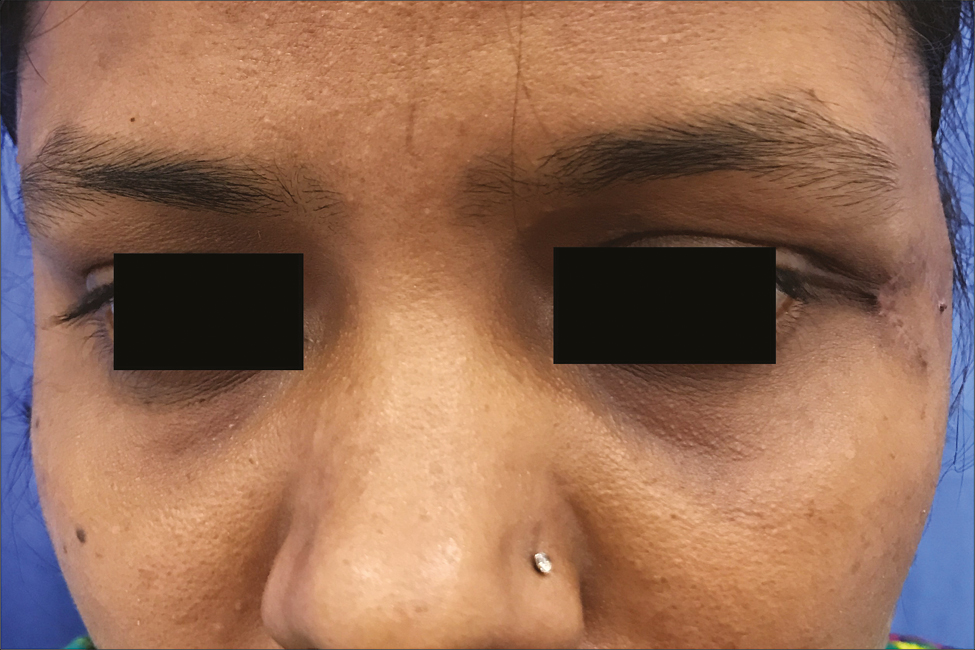
- Postoperative frontal view of the same patient demonstrating a normal-looking lateral canthus of the left eye without any intrinsic contracture
DISCUSSION
The reconstruction of skin and soft tissue defects of the face can be challenging[9] There are several reconstructive options after excision of facial scars and pathology, including primary repair, skin grafts, and different local flaps. The advent of rhombic or Limberg flap added another weapon to the armamentarium of the plastic surgeon, whereby defects over the face are successfully managed, which, otherwise, could not be closed primarily without undue tension or alternative surgery such as skin grafting. Local flaps fare better than skin grafts, as the latter are usually difficult to camouflage.
Limberg originally described the coverage of a rhombus-shaped defect by using a paper model. Skin and subcutaneous tissue are not rigid, and the paper models provide a useful but oversimplified view of flap dynamics. Some generalizations may be made from the model to assist in the design of rhombic flaps. Larrabee et al. found predictable changes in the lengths of the specific sides of the rhombic flaps. He also concluded that the actual position of the final scars was more variable than the changes in length of the sides and was related to local tissue characteristics and the ease of tissue advancement from different directions.[10] The classic rhombic transposition flap can be designed and executed off the long axis of the rhombus, but there are definite advantages to design it off the short axis of the defect.[11] The flap can be designed as small as possible while completely filling the defect. In addition, the arc of rotation of the flap is smaller.[7] Irrespective of the axis of the flap, a correct understanding of the tension forces is essential to the planning and outcome of the rhombic flap. These tension forces have been realized at two sites, first during the approximation and closure of the secondary defect and the second at the tip of the flap after transfer.[12] These forces are due to the resistance to rotation at the flap’s pedicle, shortening of the length of the flap during rotation into the recipient site, and pivotal restraint.[13] Suturing the flap into the recipient site under high tension may lead to tip ischemia and necrosis.
Nevertheless, the rhombic flaps are simple and effective owing to the geometrical design and the fact that only one measurement is needed to construct both the defect and the flap.[5] Therefore, it is easy to learn, teach, propagate, and reproduce. Excellent blood supply of the face makes it a reliable flap but mathematical calculations should be followed to avoid any tension on the suture line and tissue adjustment. Too much tension on the donor site may produce slight depression along the line of closure, which usually resolves with time but may gradually become permanent when used over a bony landmark such as nose or mandible.[14] On the contrary, our experience with scars adherent to the underlying bone also yielded reasonably good results provided proper planning and execution of the flap were performed [Figure 10].
In the present study, 85.71% of the patients were females with an average age of 23 years. Younger females usually seek consultation before their marriage. They gave consent for the surgery once the simplicity of the procedure and its aesthetic merits were explained. The fact that the surgery can be performed under local anesthesia with a quick return to work further resulted in more and more patients consenting to the surgery.
On the contrary, Mathew et al.[15] reported the execution of Limberg flaps in 11 patients, 9 males and 2 females, with age ranging from 45 to 76 years. The mean age was higher, as most of the patients had cutaneous malignancies.
In our study, the mean dimensions of the rhomboid defect and the rhombic flap were 3.26 cm but the dimensions ranged from 1.7 to 5.6 cm. The size depended directly on the site of the pathology, quality, availability, and laxity of skin in the donor area and the position of anatomic structures adjacent to the defect. Since closure of the donor site is accomplished by shifting of the local tissues, the donor site was placed in an area containing excess skin. The flexibility of the skin in the area to be excised was inspected by pinching the skin with the forefinger and thumb.[12]
Even with meticulous planning, some amount of flap disproportion was observed owing to variable characteristics of the skin and their anatomic availability in different individuals. Therefore, Gunter et al. suggested that when such an area could not be found, it may be necessary to decrease the size of the defect so that a smaller flap may suffice.[14] At times, it appeared easier to excise and suture primarily but the tangential and tractional pull on vital structures such as lateral canthus of the eye, nose, and perioral area made us rethink and plan a local flap. Skin grafts were deliberately avoided, as they usually look patchy and hyperpigmented. Camouflage of the grafted skin may not be possible, and the donor scar is usually not acceptable to females. Rhombic flaps in such cases is a viable option but too large flaps are avoided especially if they encroach on the other aesthetic facial subunits. Aydin et al. also reported a series of 24 patients, of whom 17 patients were operated on for malignancies and 5 cases were operated on due to burn contractures. Therefore, the median age was 47.5 years (range 9–83 years). The patients operated on were not only for the pathologies of head and neck but also for the extremities and torso. They also used larger flaps, with the largest dimension being 12 × 14 cm, but they did not experience partial or total flap necrosis or hematomas.[16] This study once again emphasized the survival and safety of rhombic flaps.
Alternatives to rhombic flaps are a myriad of local flaps such as transposition, bilobed, rotation, and advancement or V-Y flaps but there are limitations common to all local flaps. The correct quality of skin may not be readily available, for example after excision of lesion of/ or near the eyelids and close to hair margins. At the same time, the rhombic flaps can be designed in so many different directions that it is more often possible to construct a flap of the right skin than with less versatile designs.[5]
Correct placement of the flap is extremely challenging on the face, as facial subunits and anatomical features create confines. The flap should be positioned in the direction of minimal tension and maximum extensibility. Chasmar suggested that the incisions should not be placed on relaxed skin tension lines, but rather parallel to the relaxed skin tension lines.[17] The placement of incisions parallel to Langer’s lines allows the resulting scar to fall within the creases of the skin.[3] The flap should be raised with enough subcutaneous tissue, and generous dissection should be performed beyond the base to prevent a dog ear when the flap is transposed and sutured. In most cases, the quality of the scar is good without hypertrophy and hyperpigmentation.[5]
CONCLUSION
The simplicity and efficacy of the Limberg flap makes it versatile, allowing for adequate cosmesis with a few complications. If correctly executed and if good primary healing occurs, the Limberg flap produces excellent color and texture match.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form/ forms, the patient(s) has/ have given his/ her/their consent for his/her/ their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Modern trends in plastic surgery. Design of local flaps. Mod Trends Plast Surg. 1966;2:38-61.
- [Google Scholar]
- Mathematical principles of local plastic procedures on the surface of the human body. Leningrad: Medgis; 1946.
- Geometric limit of multiple local limberg flaps: A flap design. Plast Reconstr Surg. 1999;104:1675-8.
- [Google Scholar]
- Simplifying cheek reconstruction: A review of over 400 cases. Plast Reconstr Surg. 2012;129:1291-9.
- [Google Scholar]
- Closure of rhomboid skin defects: The flaps of limberg and dufourmentel. Br J Plast Surg. 1972;25:300-14.
- [Google Scholar]
- The significance of Langer’s lines. In: Huston JT, ed. Transactions of the 5th International Congress of Plastic and Reconstructive Surgery. Australia: Butterworth; 1971. p. :1213.
- [Google Scholar]
- Rhomboid flap in facial reconstruction. New concept of tension lines. Arch Otolaryngol. 1979;105:569-73.
- [Google Scholar]
- Complex local flap design in cheek reconstruction. Oper Tech Otolaryngol Head Neck Surg. 2011;22:53-8.
- [Google Scholar]
- The dynamics of flap movement: Effect of pivotal restraint on flap rotation and transposition. J Dermatol Surg Oncol. 1987;13:1348-53.
- [Google Scholar]
- The limberg flap for cutaneous defects - a two year experience. Indian J Surg. 2007;69:184-6.
- [Google Scholar]
- Versatile use of rhomboid flaps for closure of skin defects. Eurasian J Med. 2011;43:1-8.
- [Google Scholar]






