Translate this page into:
Efficacy of Surgical Excision and Adjuvant High-dose Rate Brachytherapy in Treatment of Keloid: Our Experience
Address for correspondence: Dr. Kalapurmat N. Manjunath, Department of Plastic & Reconstructive Surgery, MS Ramaiah Medical College (MSRMC), M S Ramaiah Nagar, Mathikere, Bengaluru 560054, Karnataka, India. E-mail: drknmanjunath@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Keloids are dermal tumors that are due to increased production of collagen caused by abnormal and prolonged wound healing. The incidence of recurrence is extremely high if only conservative measures are used. This study was conducted to evaluate the feasibility and efficacy surgery and high dose rate brachytherapy as an adjuvant therapy for treatment of keloids.
Materials and Methods:
50 patients with clinically diagnosed 71 keloids were treated with excision of keloid and post-operative high-dose rate brachytherapy were studied. Complete excision of the keloid till the healthy skin margin was excised. The wound were closed in 2 layers. Subcutaneous tissue closed using absorbable suture, over which a 6F flexible polyethylene tube was placed. High dose rate cobalt-60 brachytherapy was administered. Total of 15 Gy in divided dose, 5 Gy in 3 fractions were administered.
Results:
50 patients with 71 keloids were studied. Out of the 50 patients, 12 were male (24%) and 38 were females (76%). Age of the patients ranged between 14 and 71 years. Recurrence rate was 2% with 2 keloids recurring at 5 months interval. 4 patients scored the results as unacceptable, remaining 45 patients rated their results as excellent during their follow up at 10 days, 3 months and 6 months.
Conclusion:
Treatment of keloids in the plastic surgeon’s practice even today is still challenging. Many therapies have been described, but recurrence rate is high with mono-therapy. Combination therapy especially surgical excision with postoperative radiotherapy is best in preventing recurrence.
Keywords
Brachytherapy
keloid
recurrence
INTRODUCTION
Keloids are dermal tumors that are due to increased production of collagen caused by abnormal and prolonged wound healing.[1] Hypertrophic scars and keloids are the same lesions with different endpoints. As compared to hypertrophic scars, keloids tend to grow into the healthy surrounding skin.[2] Histopathology of keloids shows collagen bundles arranged in nodular/cluster fashion. This feature differentiates the keloid from hypertrophic or other scars.[34] Although the histo-pathological examination is well defined, the pathophysiology of keloids is less known.[2] As the pathophysiology is less defined, the treatment of keloids is also challenging. The major concern for patients as well as treating doctor is the chance of recurrence. The incidence of recurrence is extremely high if only conservative measures such as intralesional steroids are used. If surgery alone is considered, then also recurrence rate is 45%–100%.[567] However adding radiotherapy postoperatively reduces this to <40% (i.e., 8%–60%).[89101112]
But radiotherapy-induced damage to the healthy surrounding line and radiation-induced secondary malignancy are major indexing factors for perioperative adjuvant radiotherapy. Various modalities of radiotherapy have evolved in recent times, to reduce damage to healthy skin and to reduce the chances of recurrence. One of such therapy is high-dose rate (HDR) brachytherapy. This study was conducted to evaluate the feasibility and efficacy surgery and HDR brachytherapy as an adjuvant therapy for the treatment of keloids.
MATERIALS AND METHODS
A total of 50 patients with clinically diagnosed 71 keloids were treated with excision of keloid and postoperative HDR brachytherapy was studied.
Inclusion criteria
The inclusion criteria of the study were clinically diagnosed keloids.
Exclusion criteria
The exclusion criteria of the study were children aged under 13 years, pregnant, and breastfeeding women. People who were unwilling for radiotherapy and or had any contraindication for radiotherapy were also excluded from the study. All patients were well informed and consent was taken for both surgical excision and radiotherapy.
Surgical technique
Keloid excision was done under local anesthesia in most of the surgical procedures; general anesthesia was given in those cases where multiple keloid excision was contemplated. Complete excision of the keloid till the healthy skin margin was excised. The wounds were closed in two layers. Subcutaneous tissue closed using absorbable suture, over which a 6F flexible polyethylene tube was placed. Skin was closed on top of the tube. The closed end of the tube was placed at least 5 mm beyond the wound margin. Using postoperative 3D computed tomography (CT) reconstruction [Figure 1A and B], brachytherapy was planned limiting the irradiation to surrounding normal structures.
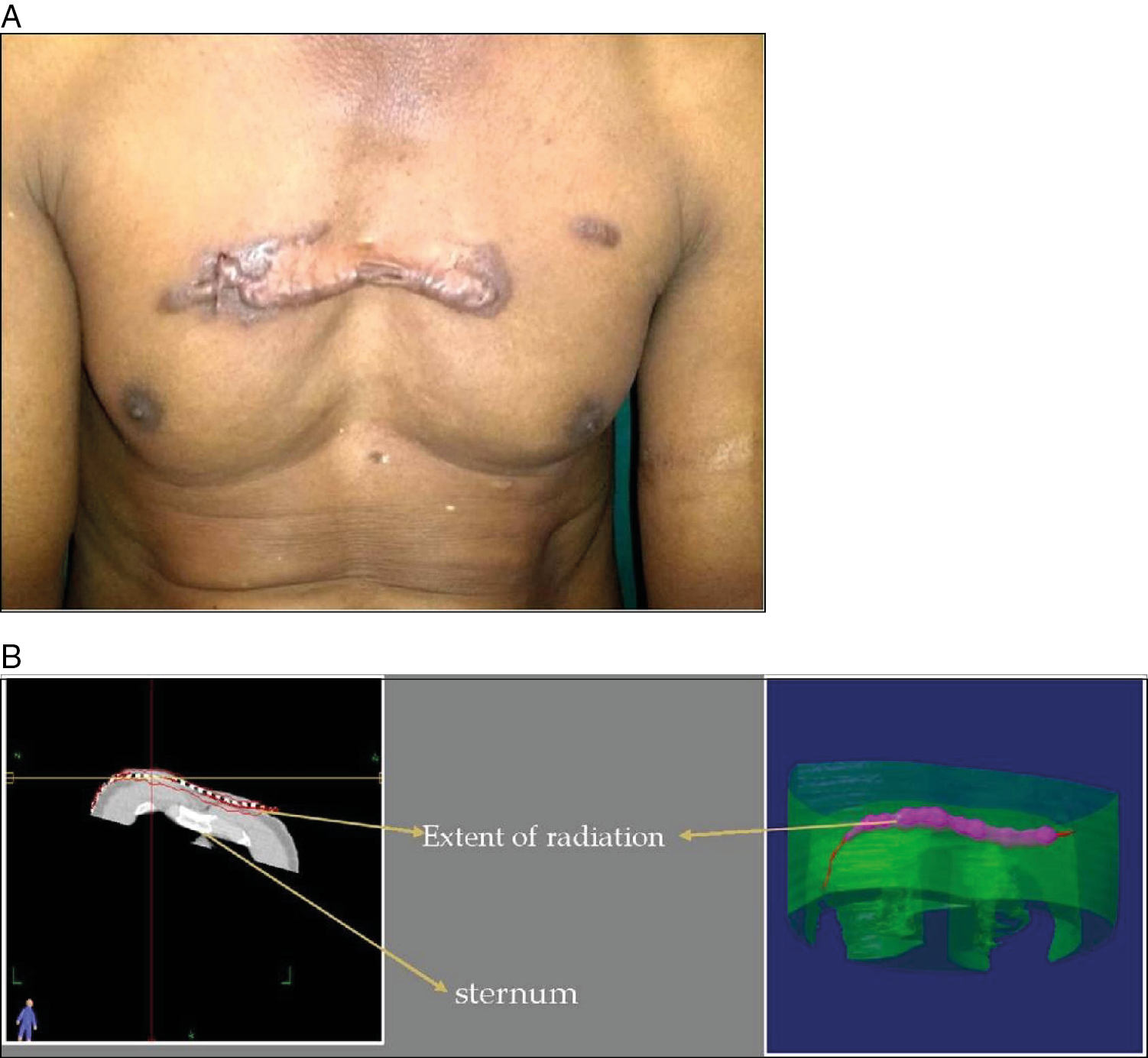
- (A) Chest keloid. (B) CT showing location of brachythearpy tube
Radiation
HDR cobalt-60 brachytherapy was administered. Of 15 Gy in divided dose, 5 Gy in three fractions were planned. The first fraction was administered within 24 h of excision of the keloid and the following two fractions were given on the next 2 days. As soon as the last brachytherapy fraction was administered, the tube placed was removed and the wound covered with a gauze pad. The patient was instructed to remove the pad the following day and follow-up on the 10th postop day for suture removal.
Follow-up and assessment
Follow-up was done at 10 days, 3 months, and 6 months. At the end of 6 months, scoring system was used to assess the recurrence as well as cosmetic acceptability. Table 1 shows the assessment characters). After 6 months, patients were advised to report if they had any recurrence or any adverse reactions.
| Scores# | |
|---|---|
| Hypopigmentation | 1 |
| Hyperpigmentation | 1 |
| Skin fibrosis/induration | 2 |
| Alopecia | 1 |
| Skin atrophy | 1 |
#Score of >3 considered unacceptable result (aesthetically)
Scar elevation more than 2 mm from surrounding skin level was considered recurrence
RESULTS
A total of 50 patients with 71 keloids were studied. Of the 50 patients, 12 were male (24%) and 38 were females (76%). Age of the patients ranged between 14 and 71 years. The most common complaint was tumor/swelling; all patients came with this complaint (100%). Next common complaint was pruritis/itching. Ear lobule was the most common site [Figure 2A–C] and formed 48% of the cases [Figure 2D]. Next most common site was chest (in 24% of patients) [Table 2]. All ear keloid patients had a history of ear piercing. Among the 24 ear keloid patients, 21 had bilateral keloid and 3 had unilateral. Keloid found in other areas was single. Of the 50 patients, 8 had recurrent keloids. They had keloids excised earlier but had not taken any adjuvant treatment. All patients had their symptoms improved. One patient of bilateral recurrent keloid had recurrence at the same site at 5 months postoperative period. By 1-year postoperative time it was of the same size as before. Recurrence rate was 2% with two keloids recurring at 5 months interval. Four patients scored the results as unacceptable; the remaining 45 patients rated their results as excellent during their follow up at 10 days, 3 months, and 6 months [Figure 3A–C]. Five of 50 (10%) patients had cosmetically unacceptable results. These patients were concerned about the pigmentation, alopecia. Later patients are advised to report if they have any symptoms or recurrence. None among the 45 reported.
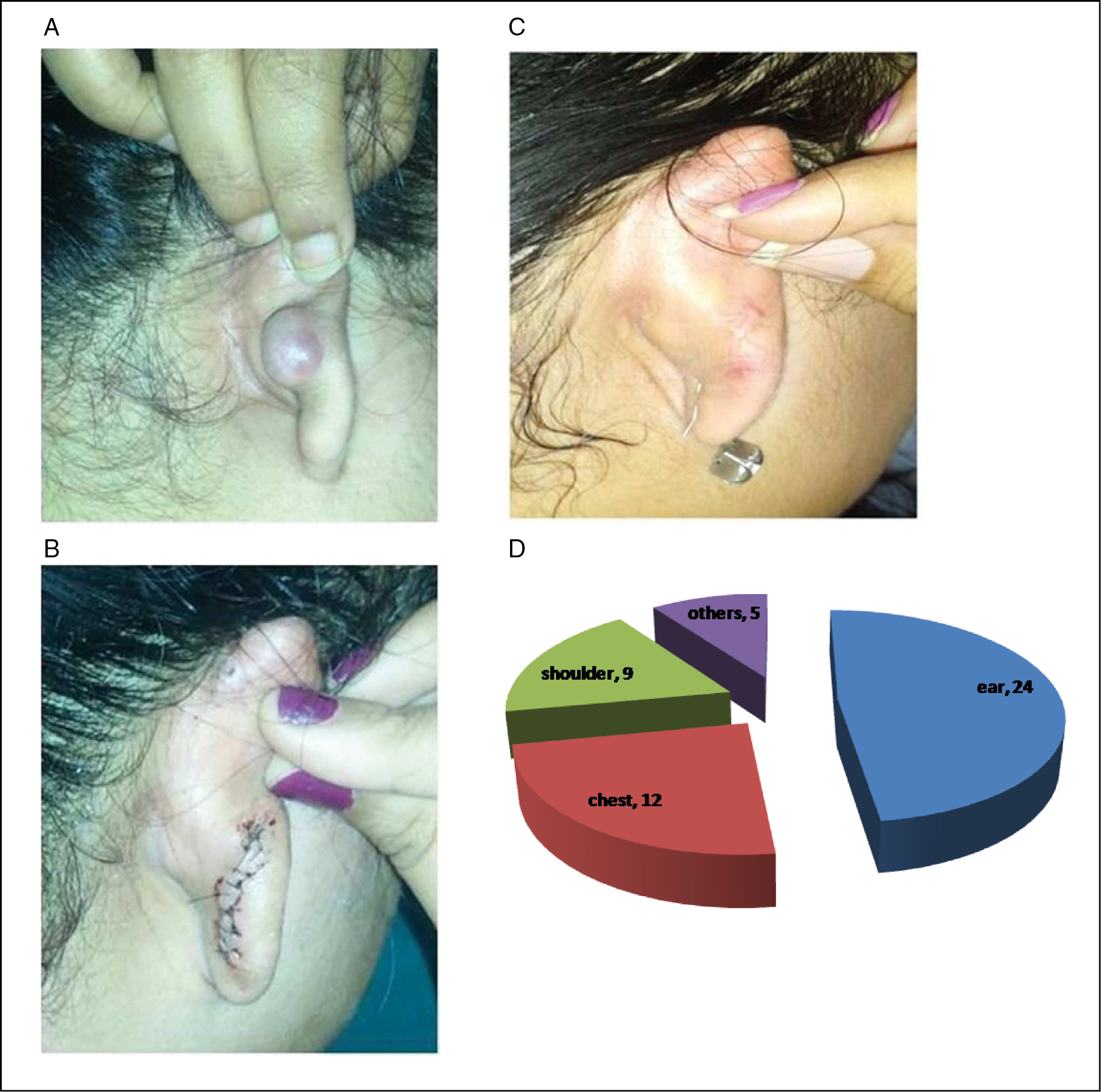
- (A) Ear keloid. (B) Immediate postop. (C) 1-year postop. (D) Site distribution of the cases
| Total number of cases | 50 | |||
|---|---|---|---|---|
| Total number of keloids | 71 | |||
| Age of patient | 14–71 years | |||
| Sex | Male-12 | Female-38 | ||
| Site | Ear-24 | Chest-12 | Shoulder-9 | Others-5 |

- (A) Shoulder keloid on excision. (B) With brachytherapy tube in situ. (C) Late postop-healed with hypopigmentation
DISCUSSION
It is a well-known fact that trauma/injury is the etiological factor for any scar formation.[13] So it is in keloid formation. During the wound healing, normally there is laying down collagen in an organized manner. But the collagen laid in a disorganized manner lead to keloids.[14] Studies show that there is an increased activity of fibroblasts to a milder stimulus leading to excess production of the collagen.[2] This increased activity leads to hypertrophic scar or the keloid. For the same reason, recurrence in these conditions is a common feature. A meta-analysis of the various studies to determine the ideal keloid treatment done by Durani and Bayat[14] failed to conclude any definite protocol. A number of studies have proposed various treatment methods such as continuous pressure after surgery,[15] intralesional corticosteroid injections,[16] silicone gel,[17] retinoic acid,[18] silastic sheet coverage,[19] carbon dioxide laser,[20] NdYaG laser,[21] 5-fluorouracil, and interferon. But not many of these are effective in treating these keloid or hypertrophic scars. Recurrences are high with monotherapy such as 33% by intralesional steroid, and above[22] 50% with laser therapy.[23] Surgical excision is effective in removing the existing tumor.[2] However, many studies have shown that surgical excision alone cannot prevent recurrence, and recurrence rate was as high as >50% at 1-year follow-up.[2425]
Many studies indicate that postoperative radiotherapy is effective in achieving good control rate as much as 67%–98%[26] and some have achieved low recurrence rate (of 6%–27%).[2728] Hence, surgical excision with postoperative adjuvant radiotherapy has been decided on the most efficacious treatment regimen for severe keloids, treatment failures and recalcitrant keloids by the international advisory.[629] Even after so many studies, developing a definitive protocol has been a challenge, as the type of radiotherapy has also evolved from gross EBRT to specific brachytherapy. However irrespective of the method used Cal and Veen recommended that dose of radiation with a BED delivery of 30Gy % is effective in preventing recurrence.[30]Table 3 shows a comparison of the doses used and the dosage in different regimens. In our study we used three fractions of 5 Gy delivered at the site at 24-h interval. In our study, as keloids were not very large a fixed dose of 5 Gy was used. This fraction of 5 Gy was considered effective in limiting the activated fibroblasts. Radiation is also known to induce rest in normal fibroblasts and prevent excess collagen production.[13] Hence, the timing of radiation is equally important. The effect of radiation is highest when started within 24 h of excision. Studies show that immature fibroblasts are recruited into the surgery site within 24 h and start laying down collagen.[41] Newly laid unstable collagen is also sensitive to radiotherapy.[42] This results in a balance between the normal and abnormal collagen, thus preventing the development of keloid. In our study also first dose of brachytherapy was given within 24 h. The low recurrence rate in our study can be explained because of these factors also.
| Malaker et al.[31] | 20 Gy | Ir 192 | Single |
| Bertiere et al.[32] | 16 Gy | LDR | Single |
| Clavere et al.[33] | 15 Gy | LDR | Single |
| Maalej et al.[34] | 20.4 Gy | Ir 192 | Single |
| Guix et al.[35] | 4 × 3 Gy | HDR | Four |
| Malaker et al.[36] | 4 × 4 Gy | Co60 | Four |
| Norkwong and Thirakhupt[37] | 3 × 5 Gy | Ir 192 | Three |
| Veen and Kal[38] | 3 × 6 Gy | Ir 192 | Three |
| 1 × 6+2 × 4 Gy | Ir 192 | Three | |
| De Lorenzi et al.[39] | 2 × 7 Gy | Ir 192 | Two |
| Arneja et al.[40] | 3 × 5 Gy | Ir 192 | Three |
| This study | 3 × 5 Gy | Co 60 | Three |
LDR = low-dose radiation, HDR = high-dose radiation, Ir 192 = iridium 192, Co 60 = cobalt 60
In our study, majority of the patients had ear keloids (48%). Ear piercing is one of the widespread practice in Indian community; the trauma caused by piercing leads to the ear keloids. Ear keloids formed 25% of patients in a study conducted by Petrou et al.[2] In another study, ear keloids formed 100% of the cases.[27] The treatment, used in our study, the combination of surgical excision, and HDR brachytherapy had excellent results and we had only one recurrence at 12 months follow-up period. The same was evident in other studies also. Study by Ogawa et al.[43] also had similar results for ear lobe keloid. The authors also found no recurrence in the head and neck region. All these studies show that the incidence of ear keloids although is more, if treated with combination therapy treated efficiently.
In our study, patients were followed up actively till 6 months postoperative. After that patients were advised to report if any complication/ recurrence. Only five patients had concerns during the period. One patient with ear keloid reported with recurrence. The recurrence was seen maximum within 2 years of therapy.[44] One of the studies showed that recurrences were within 12 months. Depending on the dosage of radiation studies have shown recurrence rate to vary between 3.5% and 27%.[4546] Intrabeam radiation was better compared to external beam radiation. As intrabeam radiation limits the injury to normal structures, HDR brachytherapy [Figure 4] has promising results as compared to low-dose radiation brachytherapy. The relapse rate varied in different studies. But majority of them had less significant relapse rate whenever HDR brachytherapy was used. One study of 36 patients had only one recurrence[38] and similar studies of 21 patients had two recurrences. Both these studies used HDR brachytherapy as adjuvant therapy. All studies have different protocols but all of them propose high dose in divided fraction started early after surgical excision effectively presented in relapse/recurrence rate.[47]
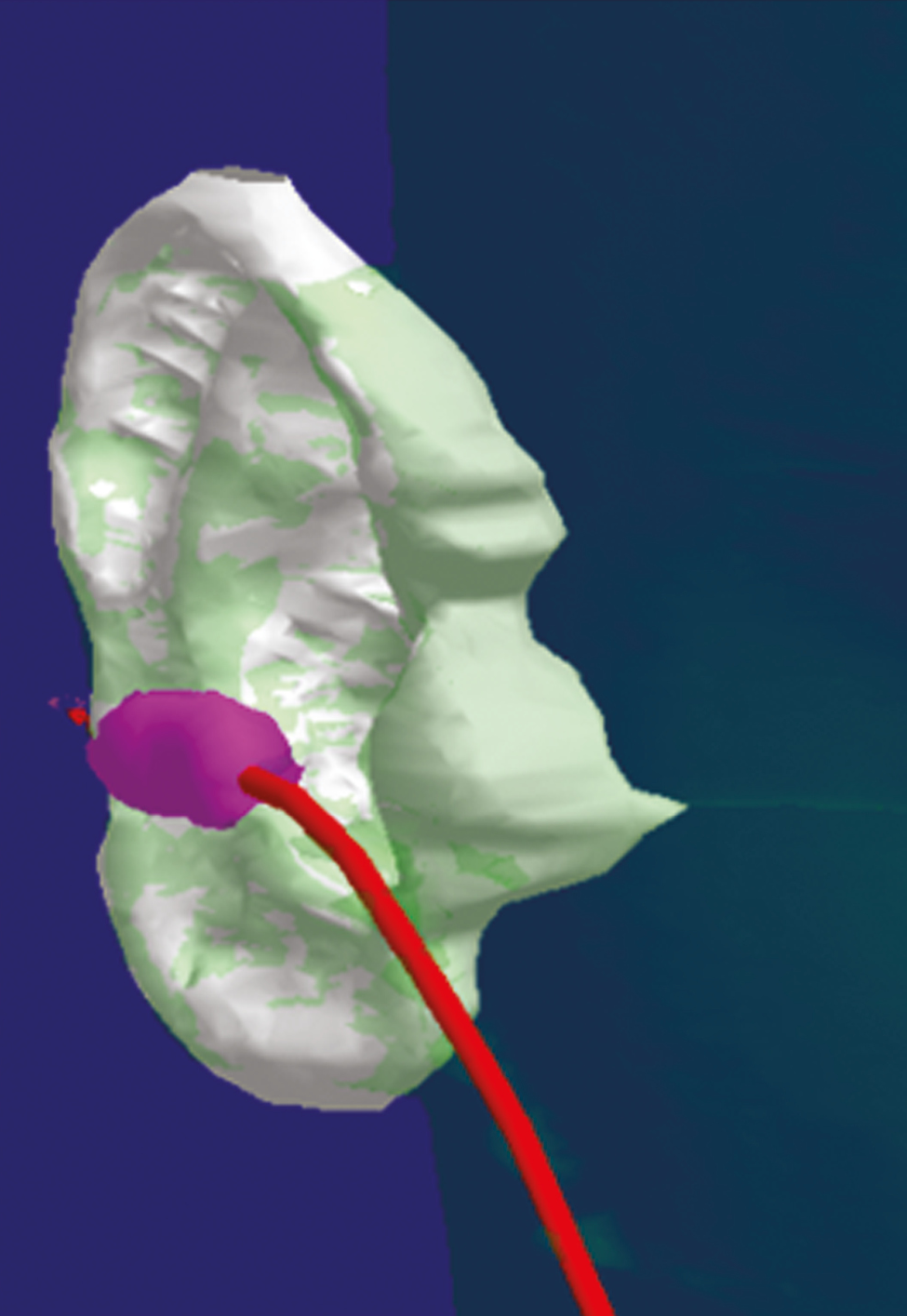
- Image showing the spread of radiation protecting the healthy ear cartilage
The major inhibiting factor for any surgeon is side effects of radiotherapy. Side effects are either encountered immediately after radiation or late. Pruritis, erythema, and pigmentation were the immediate side effects. Hyper/hypopigmentation and alopecia were late complications.[13] Alopecia resulted from the epilation of hair follicles at the site of the radiation which was seen in three of our patients. The major concern is about the radiation-induced carcinogenesis. The largest literature (between 1901 and 2009) review shows carcinogensis only in five cases. Among the five cases one was keloid transforming into malignancy.[13] In other four cases where skin cancer was reported, the radiation dose and the duration of the exposure was not documented. Many studies have found the chance of radiation-induced malignancy as just a theoretical concern[48] and some have has suggested as <0.1%. In the dose that we have used the chance of malignancy was insignificant and hence follow-up was limited to 1 year. Calculation also shows that patient getting one CT chest[49] is exposed to more radiation than the dosage we used and hence this compares the safety of the radiotherapy used for keloids. Hence, we believe that the present protocol can be effectively used in preventing the keloid recurrence.
CONCLUSION
Treatment of keloids in the plastic surgeon’s practice even today is still challenging. Many therapies have been described, but the recurrence rate is high with monotherapy. Combination therapy especially surgical excision with postoperative radiotherapy is best in preventing recurrence. HDR brachytherapy with 15 Gy in divided doses irrespective of the site has provided good results with less recurrence rate and good cosmetic result. The technique provides a high local control rate without significant complications. It is well tolerated and does not present significant side effects. The advantages of HDR brachytherapy over superficial X-rays or low energy electron beams is that it provides a better selective deposit of radiation in tissues within a short duration and causes lower degree of normal tissue damage. Studies involving large numbers will prove the efficacy. The cost involved in brachytherapy is a major hindrance for therapy in Indian subcontinent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
Pictures in original form are published in Plastic Surgery and Burns 2017;5(3):75–142. The necessary permission has been obtained.
REFERENCES
- Keloid treatment: What about adjuvant radiotherapy. Clin Cosmet Investig Dermatol. 2019;12:295-301.
- [Google Scholar]
- Proliferating activity of dermal fibroblasts in keloids and hypertrophic scars. Acta Derm Venereol. 1995;75:102-4.
- [Google Scholar]
- Differential diagnosis between keloid and hypertrophic scars: A new approach by full-field optical coherence tomography. Ann Chir Plast Esthet. 2014;59:253-60.
- [Google Scholar]
- Adjunct therapies to surgical management of keloids. Dermatol Surg. 1996;22:126-30.
- [Google Scholar]
- International clinical recommendations on scar management. Plast Reconstr Surg. 2002;110:560-71.
- [Google Scholar]
- Biologically effective doses of postoperative radiotherapy in the prevention of keloids: Dose-effect relationship. Strahlenther Onkol. 2005;181:717-23.
- [Google Scholar]
- New combination of triamcinolone, 5-fluorouracil, and pulsed-dye laser for treatment of keloid and hypertrophic scars. Dermatol Surg. 2006;32:907-15.
- [Google Scholar]
- Efficacy of intralesional 5-fluorouracil and triamcinolone in the treatment of keloids. Aesthet Surg J. 2009;29:40-6.
- [Google Scholar]
- Intralesional triamcinolone alone or in combination with 5-fluorouracil for the treatment of keloid and hypertrophic scars. Clin Exp Dermatol. 2009;34:219-23.
- [Google Scholar]
- Surgery and perioperative intralesional corticosteroid injection for treating earlobe keloids: A Korean experience. Ann Dermatol. 2009;21:221-5.
- [Google Scholar]
- German S2k guidelines for the therapy of pathological scars (hypertrophic scars and keloids) J Dtsch Dermatol Ges. 2012;10:747-62.
- [Google Scholar]
- Single-fraction radiation: A promising adjuvant therapy to prevent keloid recurrence. J Cancer Res Ther. 2018;14:1251-5.
- [Google Scholar]
- Levels of evidence for the treatment of keloid disease. J Plast Reconstr Aesthet Surg. 2008;61:4-17.
- [Google Scholar]
- Keloids treated with topical injections of triamcinolone acetonide (kenalog). Immediate and long-term results. Scand J Plast Reconstr Surg. 1977;11:169-72.
- [Google Scholar]
- Effectiveness of silastic sheet coverage in the treatment of scar keloid (hypertrophic scar) Aesthetic Plast Surg. 1988;12:95-9.
- [Google Scholar]
- Failure of carbon dioxide laser excision of keloids. Lasers Surg Med. 1989;9:382-8.
- [Google Scholar]
- Experience with the nd:YAG laser in the treatment of keloid scars. Ann Plast Surg. 1988;21:231-5.
- [Google Scholar]
- The effect of carbon dioxide laser surgery on the recurrence of keloids. Plast Reconstr Surg. 1991;87:44-9; discussion 50-3.
- [Google Scholar]
- Superficial x-ray therapy in keloid management: A retrospective study of 24 cases and literature review. Plast Reconstr Surg. 1995;95:1051-5.
- [Google Scholar]
- Evaluating keloid recurrence after surgical excision with prospective longitudinal scar assessment scales. J Plast Reconstr Aesthet Surg. 2012;65:e175-81.
- [Google Scholar]
- Up-to-date approach to manage keloids and hypertrophic scars: A useful guide. Burns. 2014;40:1255-66.
- [Google Scholar]
- Postoperative electron beam radiotherapy for keloids: Objective findings and patient satisfaction in self-assessment. Int J Dermatol. 2007;46:971-5.
- [Google Scholar]
- Radiation therapy for the adjunctive treatment of surgically excised keloids: A review. J Clin Aesthet Dermatol. 2017;10:12-5.
- [Google Scholar]
- Surgical excision with adjuvant irradiation for treatment of keloid scars. Plast Reconstr Surg. 2015;3:e440.
- [Google Scholar]
- Surgical excisionand adjuvant brachytherapy vs external beam radiation for the effective treatment of keloids:10-year institutional retrospective analysis. Aest Surg J. 2017;37:212-5.
- [Google Scholar]
- Keloid scars: A new method of treatment combining surgery with interstitial radiotherapy. Clin Radiol. 1976;27:179-83.
- [Google Scholar]
- Value of interstitial irradiation of keloid scars by iridium 192. Apropos of 46 cases [In French] Ann Chir Plast Esthet. 1990;35:27-30.
- [Google Scholar]
- Postoperative interstitial radiotherapy of keloids by iridium 192: A retrospective study of 46 treated scars. Dermatology. 1997;195:349-52.
- [Google Scholar]
- Intraoperative brachytherapy in the management of keloids. Apropos of 114 cases [In French] Cancer Radiother. 2000;4:274-8.
- [Google Scholar]
- Treatment of keloids by high-dose-rate brachytherapy: A seven-year study. Int J Radiat Oncol Biol Phys. 2001;50:167-72.
- [Google Scholar]
- Treatment of earlobe keloids using the cobalt 60 teletherapy unit. Ann Plast Surg. 2004;52:602-4.
- [Google Scholar]
- Postoperative radiotherapy with high dose rate iridium 192 mould for prevention of earlobe keloids. J Med Assoc Thai. 2006;89:428-33.
- [Google Scholar]
- Postoperative high-dose-rate brachytherapy in the prevention of keloids. Int J Rad Oncol. 2007;69:1205-8.
- [Google Scholar]
- Is the treatment of keloid scars still a challenge in 2006? Ann Plast Surg. 2007;58:186-92.
- [Google Scholar]
- Treatment of recurrent earlobe keloids with surgery and high-dose-rate brachytherapy. Plast Reconstr Surg. 2008;121:95-9.
- [Google Scholar]
- Pentoxifylline inhibits epidural fibrosis in post-laminectomy rats. Med Sci Monit. 2016;22:840-7.
- [Google Scholar]
- A novel radiotherapy approach for keloids with intrabeam. BioMed Res Int. 2019;2019:Article ID 4693528.
- [Google Scholar]
- Postoperative radiation protocol for keloids and hypertrophic scars: Statistical analysis of 370 sites followed for over 18 months. Ann Plast Surg. 2007;59:688-91.
- [Google Scholar]
- Radiotherapy of keloids. Patterns of care study – results. Strahlenther Onkol. 2003;179:54-8.
- [Google Scholar]
- The treatment of 783 keloid scars by iridium 192 interstitial irradiation after surgical excision. Int J Radiat Oncol Biol Phys. 1993;26:245-51.
- [Google Scholar]
- Radiotherapy in the management of keloids. Clinical experience with electron beam irradiation and comparison with X-ray therapy. Strahlenther Onkol. 2002;178:330-5.
- [Google Scholar]
- Outcomes of surgical excision and brachytherapy in intractable keloids. World J Plast Surg. 2017;6:280-4.
- [Google Scholar]
- Brachytherapy in the adjuvant management of keloid scars: Literature review. Scars Burn Heal. 2017;3:2059513117735483.
- [Google Scholar]
- 1990 Recommendations of the International Commission on Radiological Protection. Ann ICRP. 1991;21:1-201.
- [Google Scholar]






