Translate this page into:
Minimal Incision Technique for Gynecomastia
Address for correspondence: Dr. Souvik Adhikari, Department of Plastic Surgery, IPGME&R and SSKM Hospital, 244 A J C Bose Road, Kolkata – 700020, India. E-mail: souvikadhikari@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Gynecomastia or enlargement of the male breasts affects a large proportion of males, with most patients requiring surgical intervention as only a few lesions are actually resolved with medical management alone. Surgery cures the patients of their problems, albeit, at the cost of scarring and other cosmetic problems in some patients. Therefore, refinements in the surgical process are still ongoing so as to provide the best results with minimal scarring.
Aims and Objectives:
To find out the feasibility of a minimal incision technique for glandular excision after liposuction in patients with gynecomastia so as to decrease the final visible scars in these patients.
Materials and Methods:
From July 2018 to September 2018, eight patients were subjected to gynecomastia surgery employing liposuction and gland removal through a single transverse 5–7 mm incision in the nipple. All the patients subjected to this technique had Grade IIa gynecomastia as per Simon’s scale. The Global Aesthetic Improvement Scale, comprising a 5-point Likert scale, was employed to find out the satisfaction level of the patients 12 months after surgery; this level was compared with that of a similar population of patients being operated on by employing liposuction and subcutaneous mastectomy by the periareolar technique.
Results:
The mean operating time was 110 min, and there was minimal bleeding during the procedure. Complications were also negligible, and all patients achieved an excellent chest contour with restoration of protective nipple sensation when evaluated 12 months after surgery. The difference in mean between the 2 patient groups was 0.125 with a p-value of 0.64.
Conclusions:
Glandular excision through a single transverse incision made through the nipple is a safe approach in selected patients and it produces excellent cosmetic outcomes. However, it requires patience on the part of the surgeon to achieve the desired goals of the surgery.
Keywords
Gynecomastia
liposuction
mastectomy
minimal incision
nipple
INTRODUCTION
Gynecomastia is a condition in which the male breast gets enlarged. This condition is extremely common and it is estimated that a large number of males actually suffer from this condition, with a range varying from 40% to 70% of the population as per studies.[1] It is the adolescent population who are most commonly found with this condition, although adult males can also be affected with gynecomastia.[2]
Gynecomastia is idiopathic in most cases, although it might be associated with several other conditions, which mandates screening for the same.[3] Conditions that might lead to gynecomastia include hypogonadism, liver failure and cirrhosis, aging, testicular tumors, malnutrition, hypothyroidism, renal failure, intake of certain medications, and so on.[4] The underlying condition may be obtained by taking a proper history, performing an appropriate clinical examination, and carrying out a battery of investigations when any condition is suspected, although elaborate investigations are not required in most patients. As already mentioned, the most common cause of gynecomastia is idiopathic and the underlying pathology seems to be an imbalance between the testosterone and estrogen levels in the body, with the rudimentary breast tissue in males being more sensitive to the effect of estrogens.
Gynecomastia is characterized by breast development in males, and a histopathological examination of the excised specimens reveals that the breast swelling may comprise glandular elements admixed with fat in varying proportions.[5] If no glandular tissue is present and there is a breast swelling, then the condition is labeled as pseudogynecomastia, a condition that usually occurs in obese patients. It is important to distinguish between true gynecomastia and pseudogynecomastia, as the treatment modalities of these conditions vary.[6]
Gynecomastia may be classified on the basis of both the clinical appearance and the histopathology of the excised specimen. The most common clinical classification of gynecomastia used in practice was devised by Simon et al.,[7] with a small enlargement without any excess skin being labeled as Grade I and a large swelling mimicking the female breast being labeled as Grade III. Intermediate stages are labeled as Grades IIa and IIb. Histopathologically, gynecomastia may be classified as florid, fibrous, and intermediate as per the classification system provided by Bannayan et al.[8]
Although gynecomastia is considered a harmless condition, it may have a tremendous psychological effect on the patient.[9] Patients may be affected both emotionally and socially, with occasional suicidal tendencies and it is because of these that treatment is advocated. A watchful period of waiting and medical management may be instituted but in recalcitrant cases where the swellings persist for more than a year, surgical management is the only curative option. Surgical management is also advocated initially in severe cases of gynecomastia where surgery would be required eventually.
A variety of surgical techniques have been advocated for gynecomastia, with new techniques evolving on a regular basis. Basically, these comprise suction-assisted liposuction to target the fat component, surgical removal of the glands, and appropriate skin tailoring when needed.[10] Adjunctive procedures may also be required. However, surgery for gynecomastia is not without complications. Excessive hollowing after surgery, asymmetry of the nipples, poor scarring, and hypertrophic scarring are some of the common problems that underlie surgery for gynecomastia.[11] Scarring may be especially problematic in patients with dark-complexioned skin, where hypertrophic scars and keloids are found in high proportions.[12] In an attempt to decrease scarring, incisions are now being shortened to make the surgery aesthetically pleasing.
In this article, a minimal incision technique for managing gynecomastia is described, where a single 5–7 mm transverse incision is made over the nipple to reduce scarring and also to limit scarring to the dark nipple. This procedure is slightly time-consuming but it is essentially safe, with a very low incidence of complications noted in patients.
MATERIALS AND METHODS
Patients
Gynecomastia surgery was performed on eight male patients with gynecomastia in our institution. All of these patients were classified as having Simon IIa grade lesions bilaterally [Figure 1]. The surgery was performed under general anesthesia in three cases and under local anesthesia in five cases, as per the patient’s preference. The age of the patients varied between 20 years and 25 years. All of these patients had a Fitzpatrick skin type on a scale of either 4 or 5. The areolar diameter of the patients was between 2.5 and 4.5 cm, with a mean diameter of 3.5 cm (SD of 0.7, 2SD or 95% CI ranging from 2.1 to 4.9). [Table 1]

- Preoperative picture of a patient
| Characteristics | Patients |
|---|---|
| Total number | 8 |
| Age range | 20–25 (Mean Age 22.5) |
| SD of 2.07 | |
| 2SD or 95% CI ranging from 18.36 to 26.64 | |
| Grade IIa gynecomastia | 8 |
| Bilateral gynecomastia | 8 |
| BMI of patients | 20.6–24.7 (Mean BMI 22.9) |
| SD of 1.487 | |
| 2SD or 95% CI ranging from 19.92 to 25.87 | |
| Areolar diameter (cm) | 2.5–4.5 cm (Mean 3.5 cm) |
| SD of 0.7 | |
| 2SD or 95% CI ranging from 2.1 to 4.9 cm |
Preoperatively, all patients were screened for any hormonal imbalance and associated conditions and only those patients categorized to be having idiopathic gynecomastia were included in the study. Ethical standards were followed for every patient. The patients also had an ultrasound done to characterize their gynecomastia, with glandular tissue increasing diffusely in the retroareloar region, noted in the ultrasound, and extending to the periphery.
Appropriate investigations were then done so as to ensure that the patients were fit for the surgical procedure and these were accompanied by an appropriate preanesthetic checkup.
The procedure was explained to the patients along with the possibility of complications that might accompany the procedure, and appropriate consent was obtained from them. Consent for taking photographs and recording videos was also obtained from the patients.
Anesthesia
Patients were given the option of being operated under either general anesthesia or local infiltration anesthesia: Three patients were operated under general anesthesia and five patients were operated under local anesthesia, as per the patient’s choice.
Surgical technique
The patients were first marked in the standing position. The areas of the breasts were marked out: the inframammary folds and the surrounding area for liposuction. The patients were next placed in the supine position, and infiltration started in the marked-out areas. The infiltration solution comprised Ringer’s lactate along with lignocaine and adrenaline (500ml of Ringer’s lactate, 15ml of 2% lignocaine, and 1ml of 1:1000 adrenaline). After a waiting period of 15 min, liposuction was started. Suction-assisted liposuction was done in all cases. Conventional liposuction ended when the pinch test revealed that mostly glandular tissue was present. After this, in cases where there were large glandular components in the peripheral aspect, special gynecomastia cannulas were used for gland removal along the periphery through the same liposuction port. [Figure 2] This was done carefully so as to eliminate the glands extending to the periphery, as anatomical studies have shown that the glands extend in all directions to the periphery and surgical resection might not be complete unless these areas are addressed.[13]

- Completion of liposuction
Once liposuction was complete with the serrated cannula, a 5–7 mm transverse incision was made over the nipple and deepened with a No. 15 blade. Once the blade progressed around 1 cm into the tissue, it was then rotated in all directions so as to ensure that a rim of breast tissue remained under the nipple-areolar complex in all directions. Then, progressively, breast tissue was removed from all quadrants in an incremental fashion, taking the central part out first [Figure 3A]. Since the slit was small, strips were taken out by holding them with an Allis tissue forceps and excising them in an incremental manner. The surgery ended when no breast tissue was found remaining, apart from the rim under the nipple-areolar complex, after the pinch test [Figure 3B]. The pinch test determined that adequate subcutaneous fat was remaining under the excision zone, with no evidence of glands palpated between fingers. Care was taken to ensure that the fascia overlying the pectoralis muscle was not damaged during the procedure so as to eliminate the prospect of troublesome bleeding from the perforating vessels.[14] Hemostasis was secured and a drain was inserted through the liposuction port, which was removed after 48–72 hours. The nipple incision was closed with 1 or 2 stitches by using 4-0 nylon, and a compression bandage was applied. [Figure 4] The liposuction effluent and the glands removed by this procedure are demonstrated in a case. [Figure 5] The stitches were removed 7 days after surgery.
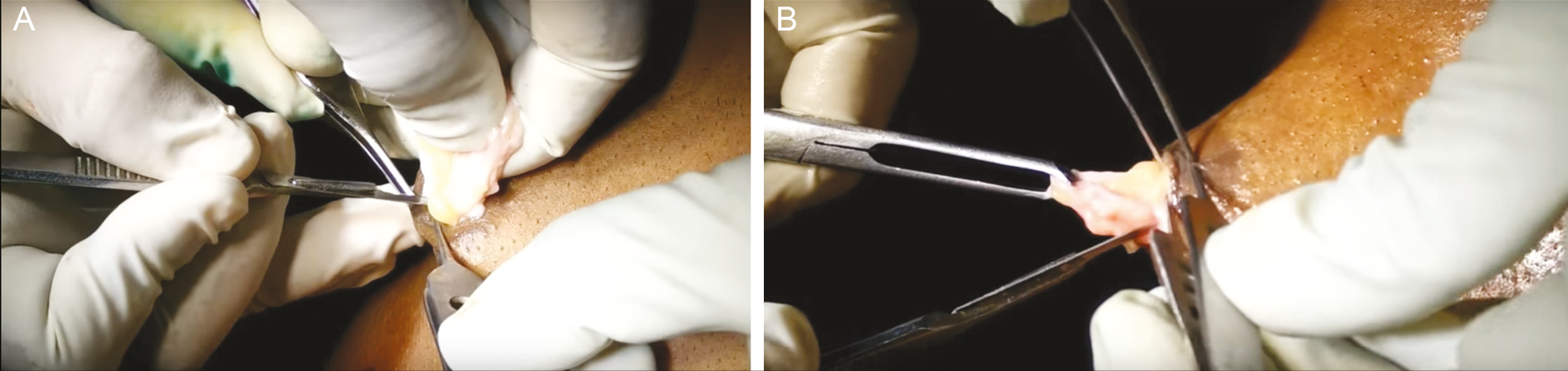
- A: Central part of breast tissue being extracted out through the nipple incision. B: Peripheral part being grasped with an Allis forceps and removed

- After completion of surgery (nipples have been sutured and drains are in place)
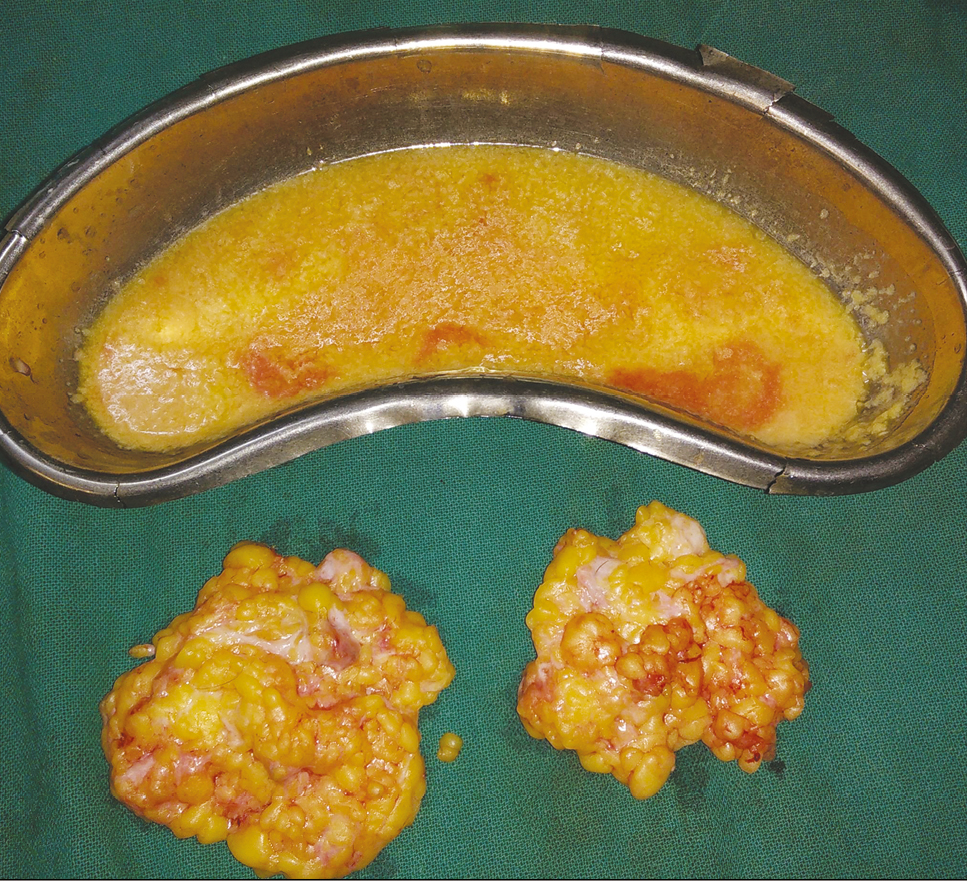
- Demonstrating the liposuction effluent and glands excised
Follow-up after surgery
The patients were followed up at 3 days when the drains were removed, 7 days when the stitches were removed, and finally at 4 weeks, 6 months, and 12 months after surgery. Surgical data along with clinical improvement and complications were noted in every patient and recorded.
Evaluation of surgery outcome in patients
Since there is no formal questionnaire related to an improvement in the quality of life in patients operated for gynecomastia, the patients and their family members were asked about their degree of satisfaction after the procedure and it was compared with that of patients of similar grades who underwent formal liposuction and subcutaneous mastectomy by using a periareolar incision. Final evaluations were done at 12 months after surgery.
RESULTS
From July 2018 to September 2018, eight patients with Grade IIa gynecomastia were operated on by using the minimal incision technique. The average age of the patients was 22.5 years, with a range between 20 years and 25 years (SD of 2.07, 2SD or 95% CI ranging from 18.36 to 26.64). The average BMI of the patients was 22.9, ranging from 20.6 to 24.7 (SD of 1.487, 2SD or 95% CI ranging from 19.92 to 25.87). Of these, three patients were operated under general anesthesia and five patients were operated under local anesthesia, as per the patient’s choice. The total infiltration volume ranged from 120ml to 260ml (mean 190ml, SD of 38.04, 2SD or 95% CI ranging from 114.17 to 266.33). The total effluent from liposuction ranged from 110ml to 230ml (average 160ml, SD of 40.62, 2SD or 95% CI ranging from 78.76 to 241.24). The mean operating time was 110 minutes (ranging from 95 min to 135 min, SD of 13.62, 2SD or 95% CI ranging from 82.76 to 137.24). The mean weight of glands excised was 90 gm (ranging from 80 gm to 120 gm, SD of 14.88, 2SD or 95% CI ranging from 60.24 to 119.76). Apart from the liposuction port and the nipple, no other incisions were used and the skin was not resected in any of the patients. The same surgeon operated on all of the patients, albeit, with different assistants and the patients were discharged the next day after surgery. Drains were removed 48–72 hours after surgery whereas stitches were removed 7 days after surgery, and the compression garment was continued for 2 weeks.
Complications
Bleeding was minimal during the surgical procedure in all patients, although one patient had a somewhat excessive blood-stained effluent through the drain on one side, which resolved by itself. All patients had hypopigmentation of the central part of the nipple, which resolved within a month of the surgery so that the final scar was barely seen in the long term. Apart from this, there were no other complications or wound-healing problems in any patient.
Outcome
All patients were extremely satisfied after the surgery. The scars were barely visible in the nipple area, and the chest contour was excellent in all cases. [Figure 6A–C] There was no evidence of any recurrence at 12 months after the surgery in any patient. Most patients had a swelling immediately after the surgery and some skin redundancy; however, all these were restored back to normal when an examination was done at 6 and 12 months. Although the nipples were insensate immediately after the surgery, protective sensation was restored in every patient at 6 months after the surgery. The Global Aesthetic Improvement Scale, comprising a 5-point Likert scale, was employed to find out the satisfaction level of the patients (ranging from 1: extremely satisfied to 5: condition worsened after surgery). The mean value was 1.375 with an SD of 0.5175 (2SD or 95% confidence interval ranging from 0.34 to 2.41). The mean value of another set of eight patients with a similar grade of gynecomastia operated on by liposuction and subcutaneous mastectomy by periareolar incision was 1.5 with an SD of 0.5345 (2SD or 95% confidence interval ranging from 0.43 to 2.569). The difference in mean was 0.125 with a p value of 0.64 [Table 2].
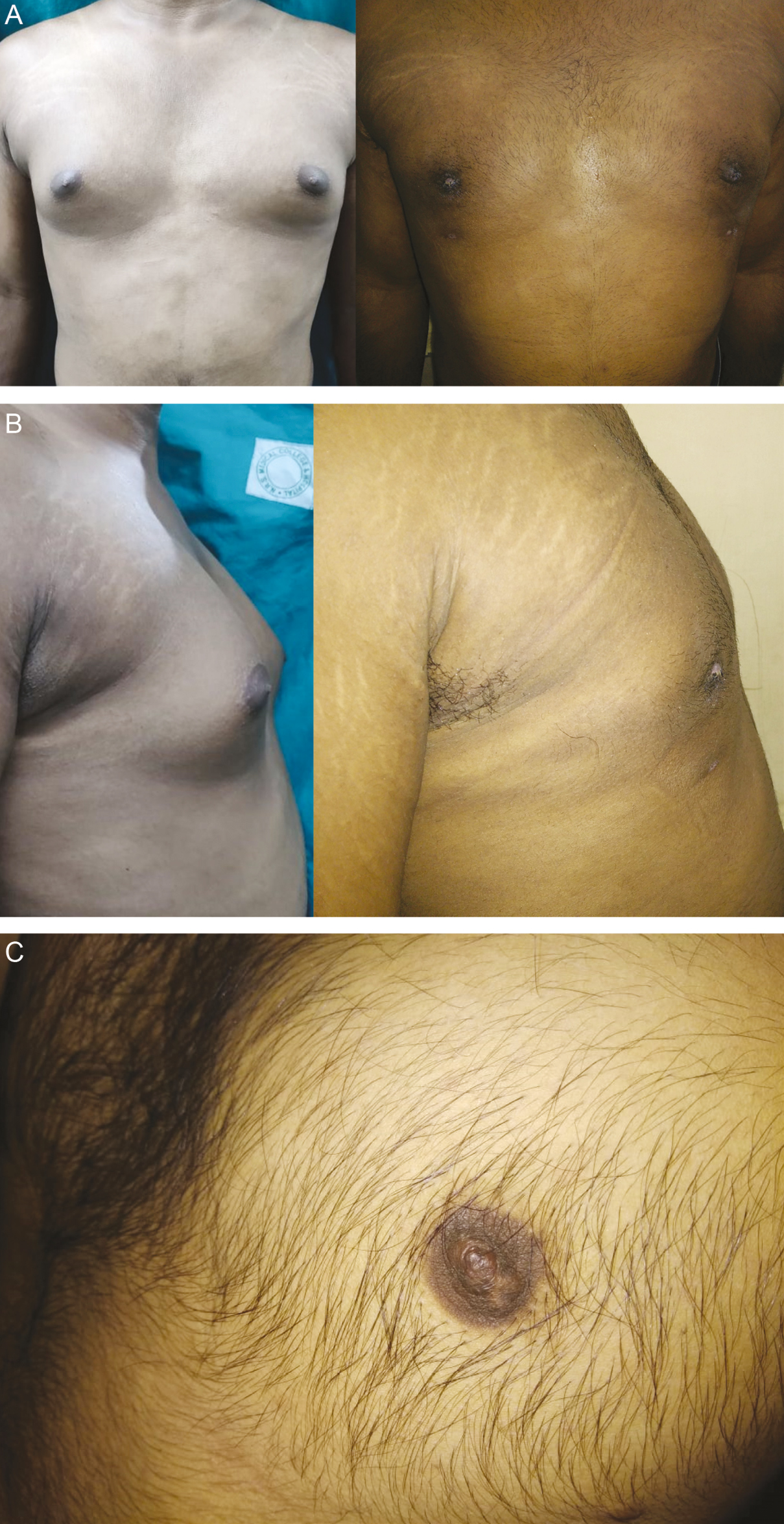
- A: Early (2 week) postoperative picture with slight nipple hypopigmentation. B: View from the side after 2 weeks postsurgery. C: Close view of nipple scar after 6 months in another patient
| Parameter | Result |
|---|---|
| Surgery under local anesthesia | 5 |
| Surgery under general anesthesia | 3 |
| Total infiltrate | 120 ml–260ml (mean 189ml) |
| SD of 38.04 | |
| 2SD or 95% CI ranging from 114.17 to 266.33 ml | |
| Total liposuction effluent | 110 ml–230ml (mean 160ml) |
| SD of 40.62 | |
| 2SD or 95% CI ranging from 78.76 to 241.24 ml | |
| Operating time | 95 min–135 min (mean 110 min) |
| SD of 13.62 | |
| 2SD or 95% CI ranging from 82.76 to 137.24 min | |
| Excised gland weight (total) | 80 gm–120 gm (mean 90 gm) |
| SD of 14.88 | |
| 2SD or 95% CI ranging from 60.24 to 119.76 gm | |
| Global Aesthetic Improvement Scale | 1–2 (mean 1.38) |
| SD of 0.5175 | |
| 2SD or 95% CI ranging from 0.34 to 2.41 | |
| Comparison with the periareolar incision group Difference in mean | 0.125 |
| p value | 0.64 |
DISCUSSION
Adolescents and adults who have gynecomastia who are unresponsive to medications and who face psychological problems are good candidates for surgery. The aim of the surgery for gynecomastia is excision of the breast tissues while maintaining a normal contour of the chest and nipple without asymmetry and while preventing unsightly scars and recurrence in the long run.[5] A variety of surgical procedures have been described, with new techniques coming up on a regular basis to reduce scarring and lessen complications. Initially, the glandular tissue and fat were taken out directly through a variety of incisions, including infra-areolar, periareolar, transareolar, or circumareolar, and this process is known as subcutaneous mastectomy.[15] In a large percentage of these patients, this surgical procedure can lead to a sinking of the nipple and an unsightly hollow over the excised area with poor scarring in many cases. With the advent of suction-assisted liposuction, it was easier to address fat deposits of the chest, thereby achieving a good chest contour.[16] However, the residual glandular tissue still needs to be excised to complete the surgery through any of the access incisions.
Ultrasonic-assisted liposuction is an advancement in the field of liposuction when applied to gynecomastia, with studies implying excellent cosmetic outcomes.[17] Endoscopic surgical removal of glandular tissue can also serve the purpose, with excellent results.[18] Other investigators have utilized a criss-cross incision over the nipple for glandular removal after liposuction.[19] The pull-through technique via the liposuction port has also been employed.[20]
In this study, the safety of a new technique employing the removal of glandular tissue through a small 5–7 mm transverse incision made through the nipple after adequate liposuction has been completed is demonstrated. The peripheral glandular tissue can be addressed by using special serrated or sharp-cutting liposuction cannulas after conventional liposuction is complete.[21] A cross-chest liposuction can also be done to facilitate better fat removal.[22] The shift in location of the incision from the periareolar to the nipple area was done while keeping in mind the skin type of Indian patients, where hypertrophic scarring is a genuine possibility that would pose aesthetic problems when placed in the periareolar area. The incision in the nipple healed well in all cases, with an imperceptible scar in the long run, and this resulted in improved cosmetic outcomes; however, in all cases, there was initial hypopigmentation in the central part of the nipples.
A similar approach can be used with the endoscope to remove the glandular tissue, and this could be comparable with the current technique described. It is important to keep a rim of tissue around 1 cm behind the nipple-areolar complex so as to prevent the nipple sinking during the postoperative period.
Once the procedure was carried out by sweeping the blade in either a clockwise or counter-clockwise fashion, the breast tissue was excised in strips by simply pushing the knife between the breast tissue and the subcutaneous fat. Tissue planes of dissection were facilitated by using comprehensive liposuction before gland excision. Liposuction also facilitated defining the plane between the glandular tissue and the pectoralis fascia so that the latter was not breached when excising strips and troublesome hemorrhage from the perforators was thereby avoided. The assistant could actually push on the glandular tissue, which facilitates strip removal. The strips were caught by using an Allis tissue forceps, and gentle pushing and pulling can result in a smooth removal of tissue. This procedure is time-consuming and hence, patience is recommended. Finally, the access incision was closed by using one or two sutures of nylon; a drain was inserted through the liposuction port on either side, and it was removed 72 hours after the surgery. This procedure is quite safe and has minimal complications, with a high degree of satisfaction in the patients.
Proper patient selection is important when employing this technique. Not all patients with gynecomastia can be subjected to this procedure. Only patients having Grade I or IIa gynecomastia as per Simon’s scale can be offered this type of surgery. Patients with larger grades, especially Grade III patients, should not be subjected to this procedure, as they inevitably need skin excision as part of the procedure for best aesthetic results, which cannot be provided with this technique. These patients are better addressed with circumareolar or vertically based excisions. This surgery should also be avoided in patients having problems with blood coagulation, in whom a larger incision would be better to manage troublesome hemorrhage should it happen. This procedure is also not recommended for patients with glands that have a hard consistency on preoperative checkup (where an ultrasound indicates primarily glandular tissue in the breasts).
Whether liposuction should be used before or after gland removal is debatable, with some investigators employing it either before or after gland removal. In this series, the application of liposuction is considered before gland removal due to two reasons: (a) Liposuction developed adequate planes of dissection between the gland and subcutaneous fat and also between the gland and pectoralis fascia, which facilitated gland removal through the small incision without any injury to the internal mammary perforators, thereby avoiding troublesome hemorrhage, which could have been difficult to manage given the small access incision; (b) liposuction using the serrated cannulas adequately addressed removal of the glands in the periphery, which was then confirmed clinically. This did not produce any contour irregularities in the postoperative period, and patients experienced a very high degree of satisfaction after this surgery.
CONCLUSION
In conclusion, a new minimal access incision over the nipple is portrayed here for gland removal after liposuction. The criss-cross incision advocated by others is avoided, thereby utilizing a transverse incision only in our patients. An additional difference is the utilization of serrated cannulas for the removal of glandular tissue in the remote peripheral locations, thereby making this surgery complete in all aspects with excellent cosmetic outcomes.
Limitations of the study
The study had a very small sample size of eight patients, which is a major limitation; however, as a larger number of patients are subjected to this technique, its efficacy can be properly ascertained. The small sample size is primarily due to the apprehension of the patients toward a new technique and the increased operative time required, which was informed to them. The patients were not randomized and were subjected to the surgical technique as per their own choice and that of the operating surgeon. No postoperative ultrasound was done to confirm complete excision of the glands, as the patients did not agree to it and they were satisfied with the results of the surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form/forms, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in this journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Plasma testosterone and estrogens in pubertal gynecomastia. Z Kinderheilkd. 1973;115:89-94.
- [Google Scholar]
- Surgical correction of gynecomastia in thin patients. Aesthetic Plast Surg. 2011;35:439-45.
- [Google Scholar]
- Classification and surgical correction of gynecomastia. Plast Reconstr Surg. 1973;51:48-52.
- [Google Scholar]
- Gynecomastia: Clinicopathologic study of 351 cases. Am J Clin Pathol. 1972;57:431-7.
- [Google Scholar]
- The round-the-clock technique for correction of gynecomastia. Arch Plast Surg. 2019;46:221-7.
- [Google Scholar]
- Gynecomastia surgery-impact on life quality: A prospective case-control study. Ann Plast Surg. 2017;78:264-8.
- [Google Scholar]
- Correction of gynecomastia through a single puncture incision. Aesthetic Plast Surg. 2007;31:244-9.
- [Google Scholar]
- Hypertrophic scarring and keloids: Pathomechanisms and current and emerging treatment strategies. Mol Med. 2011;17:113-25.
- [Google Scholar]
- Anatomy of the gynecomastia tissue and its clinical significance. Plast Reconstr Surg Glob Open. 2016;4:e854.
- [Google Scholar]
- The blood supply to the nipple-areola complex of the human mammary gland. Aesthetic Plast Surg. 2004;28:393-8.
- [Google Scholar]
- A systematic approach to the surgical treatment of gynaecomastia. Br J Plast Surg. 2003;56:237-46.
- [Google Scholar]
- Our experience with the so-called pull-through technique combined with liposuction for management of gynecomastia. Ann Plast Surg. 2004;53:22-6.
- [Google Scholar]
- Gynecomastia management: An evolution and refinement in technique at UT southwestern medical center. Plast Reconstr Surg Glob Open. 2016;4:e734.
- [Google Scholar]
- Endoscopic subcutaneous mastectomy: A novel and effective treatment for gynecomastia. Exp Ther Med. 2013;5:1683-6.
- [Google Scholar]
- Trans-nipple removal of fibro-glandular tissue in gynaecomastia surgery without additional scars: An innovative approach. Indian J Plast Surg. 2014;47:50-5.
- [Google Scholar]
- Prospective analysis and comparison of periareolar excision (delivery) technique and pull-through technique for the treatment of gynecomastia. Aesthetic Plast Surg. 2020;44:653-61.
- [Google Scholar]
- A sharp cutting liposuction cannula for gynecomastia. Aesthet Surg J. 1998;18:261-5.
- [Google Scholar]






