Translate this page into:
Acral Nodular Melanoma Presenting With Rapid Progression
Address for correspondence: Dr. Sunil Vitthalrao Jagtap, Department of Pathology, Krishna Institute of Medical Sciences, Deemed University, Karad 415110,Maharashtra, India. E-mail: drsvjagtap@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Melanoma is a malignant tumor that is derived from melanocytes of the skin and other sites. Melanoma accounts for 1% to 3% of all malignancies and 1% to 2% of all cancer deaths worldwide. We are presenting a case of a 42-year-old female who presented to the surgery department with a growth over the right heel since 18 months, with a history of trauma to the site. The lesion showed rapid progression with a large mass and secondary skin ulceration and sloughing. A PET scan showed an enhancing lesion on the right heel measuring 11 mm in thickness. There was no evidence of any systemic organ or any lymph node metastasis. Surgical excision and reconstruction on the part of the heel by a local flap with sural graft with split-thickness skin grafting was done. The excised growth was sent for histopathology. The histopathological diagnosis of nodular melanoma (NM) of the heel was given. We are presenting this case for its clinical, histopathological, and surgical management.
Keywords
Melanoma foot
reconstruction skin grafting
surgical management
INTRODUCTION
Melanoma is a malignant tumor that is derived from melanocytes of the skin and other sites. The incidence of melanoma is increasing faster than any other cancer in the world. Melanoma accounts for 1% to 3% of all malignancies and 1% to 2% of all cancer deaths worldwide. An NM of the foot is a relatively uncommon. The term “acral” defines the location, which is of the extremities, namely the skin of the hands and feet, including the nail unit. Melanoma arising on the foot carries a poor prognosis when compared with melanoma arising at other body sites.[1]
CASE REPORT
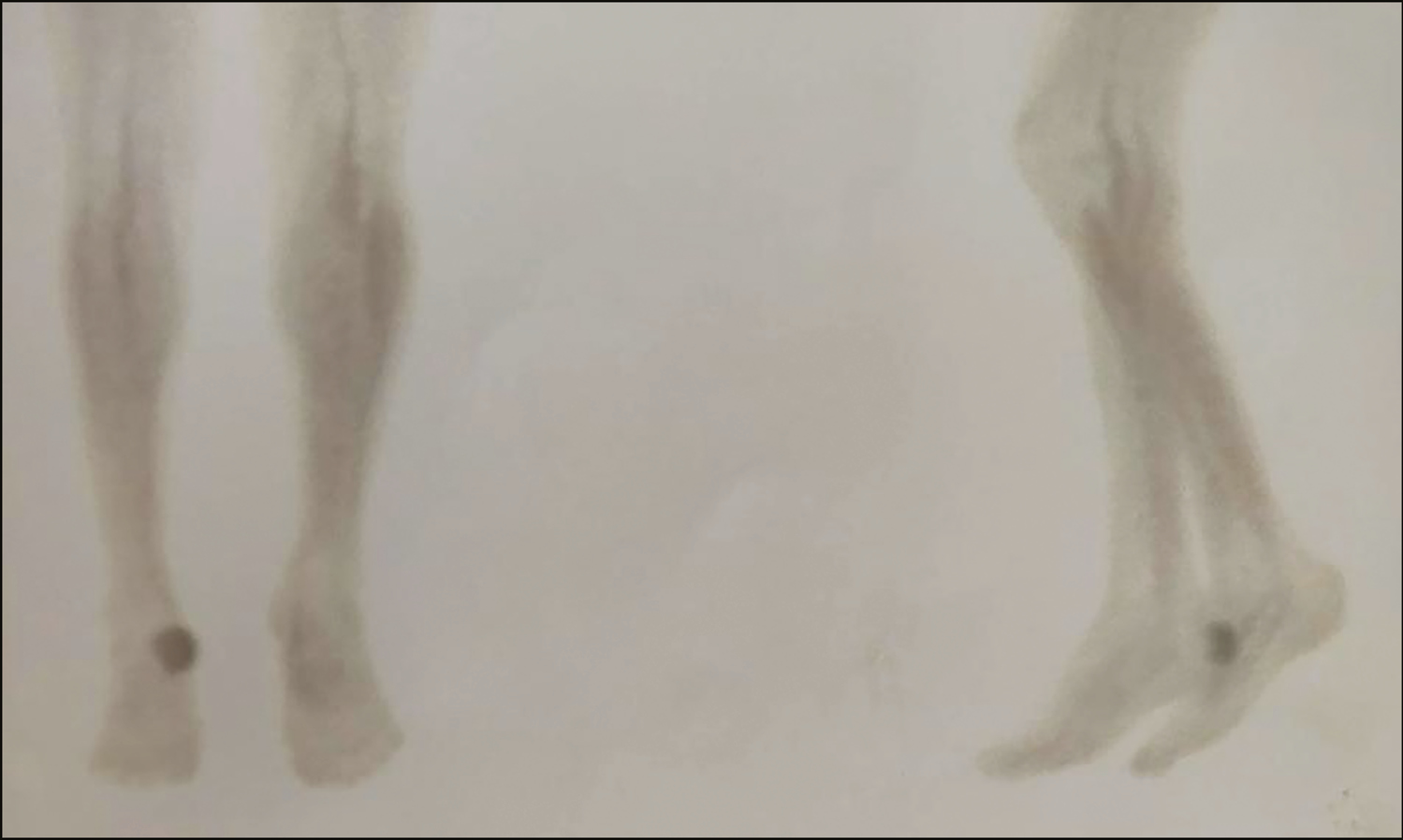
We present the case of a 42-year-old female who was evaluated at Krishna Institute of Medical Sciences in Karad for a malignant melanoma (MM) of the heel. The patient was without any family history of cancer. She presented with a growth over the right heel since 10 months, with a history of trauma to the site. She was apparently alright and had a history of trauma, after which there was a small lesion that kept on increasing to a size of 10 × 10 cm; it exhibited asymmetry, border irregularities, color heterogeneity, and elevation. The patient recalled that over the preceding 18-month period, the lesion increased in size, was ulcerated, painful, and bleeding. There was no significant family history. Systemic examination revealed no evidence of any disease or metastasis. On radiological evaluation, x-ray and PET scan showed an enhancing lesion on the right heel measuring 11 mm in thickness. There was no evidence of any systemic organ or any lymph node metastasis. There was no evidence of any abnormal hypermetabolic elsewhere in the body [Figures 1–4].

- X-ray showing increased soft tissue density at right heel A/P, and lateral view

- PET scan showed enhancing lesion on right heel measuring 11 mm in thickness. There is an evidence of abnormal hypermetabolic.
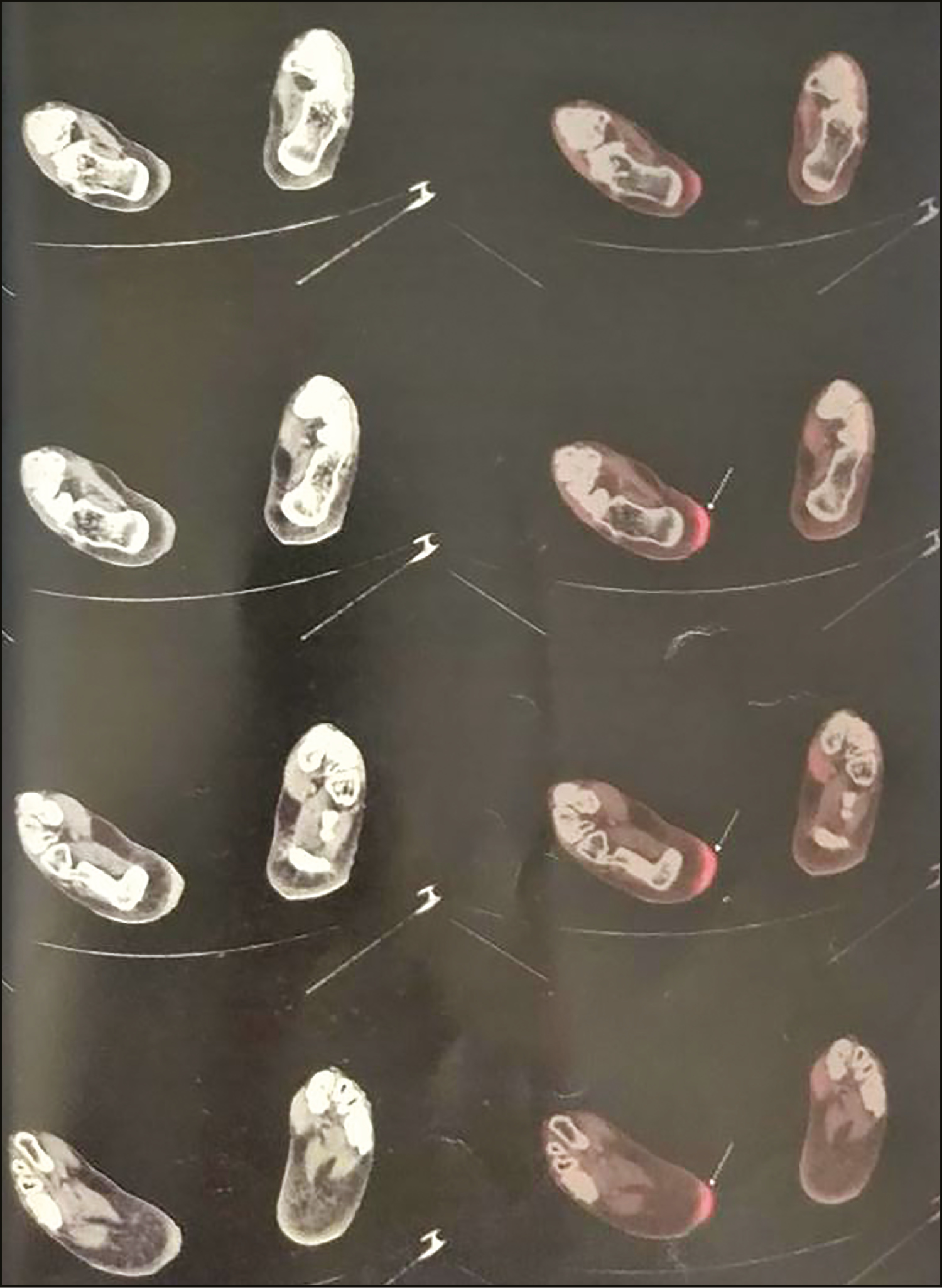
- PET scan showing enhancing lesion on right heel. Arrow showing the evidence of abnormal hypermetabolic
- PET scan showed enhancing lesion on right heel.
Surgical excision and reconstruction on the part of the heel by local flaps was done with a sural graft with split-thickness skin grafting [Figure 5A–D].
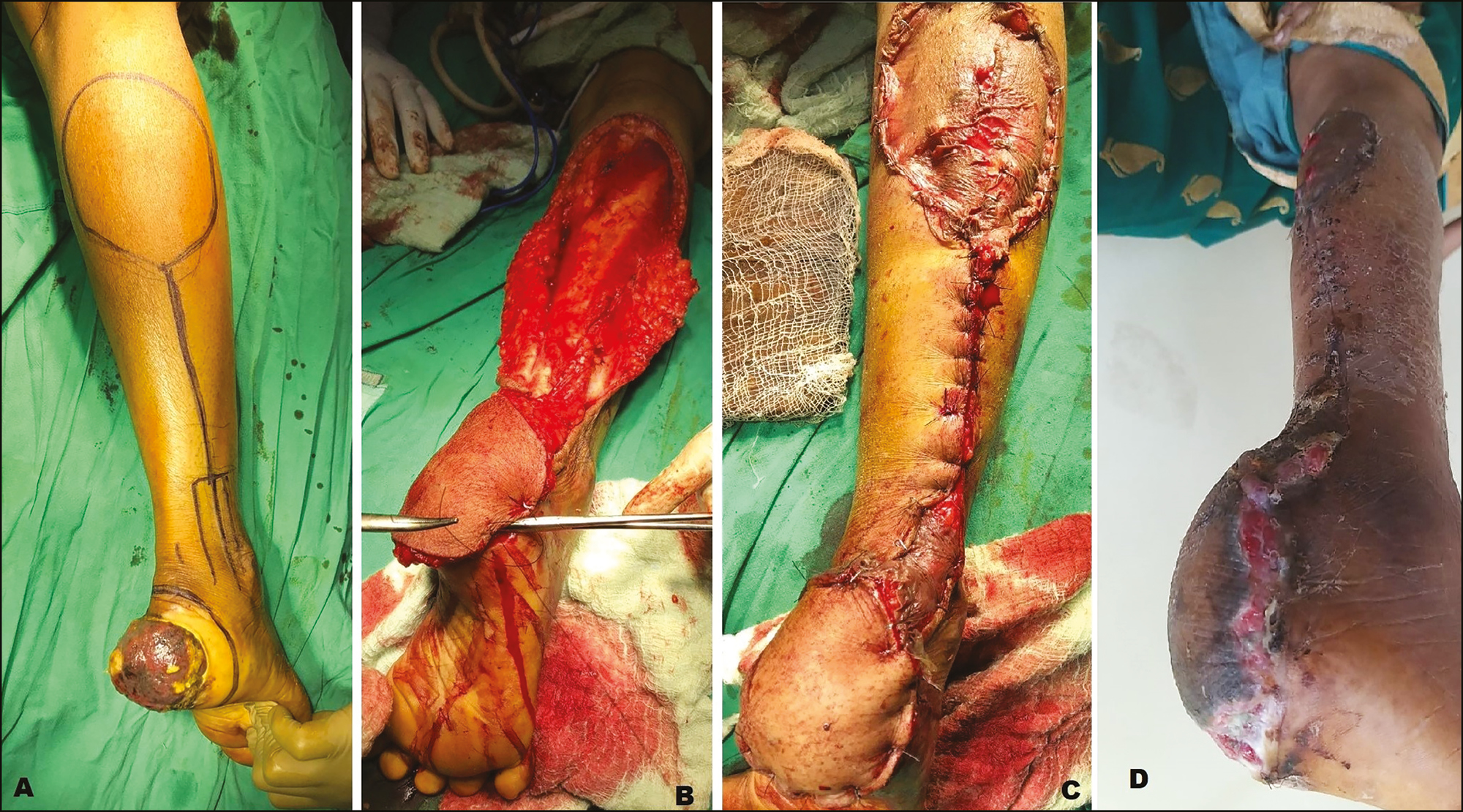
- (A) Preoperative, (B) intraoperative, (C) postoperative, and (D) follow-up images of acral melanoma
Gross: We received a specimen labeled as right heel melanoma totally measuring 7 × 6 × 3 cm. The external surface showed a large mass measuring 5.5 × 4.5 × 1.5 cm. The external surface of the mass showed multiple, large, ulcerated areas with exudative slough. The cut section showed a nodular, blackish area with hemorrhage [Figure 6A–C].
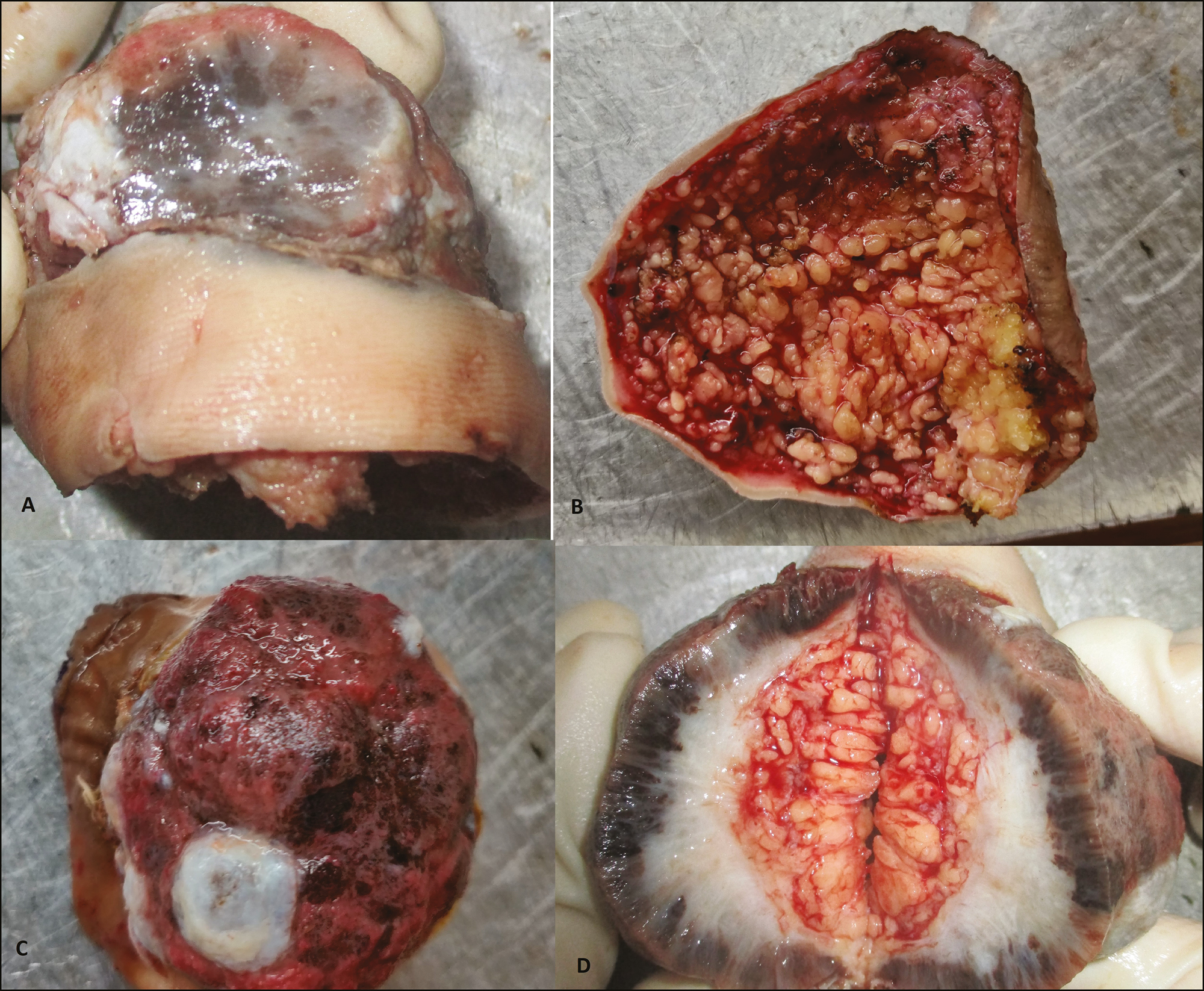
- (A) Gross specimen of excised right heel lesion, (B) tumor deep surgical margin, (C) tumor with ulcerative nodular growth with heavy blackish pigmentation, and (D) cut section showing nodular brownish black tumor
Microscopy showed MM with prominent nodular growth and a vertical component of the invasion of the tumor. A tumor cell with heavy melanin pigmentation was noted [Figure 7A–C].
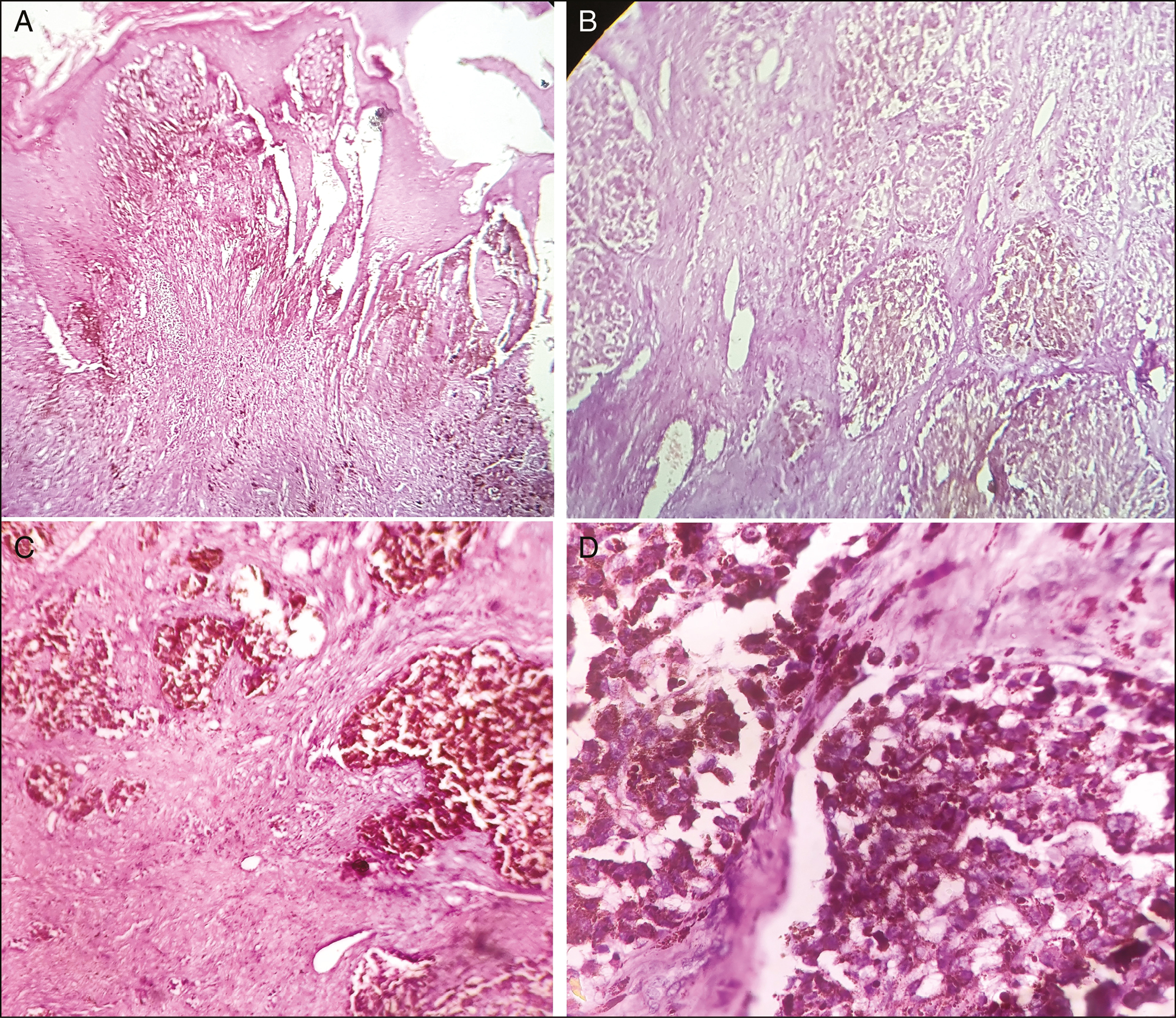
- (A, B) NM with nodular growth of a prominent vertical component to the invasion of the tumor (H&E stain, 40×). (C, D) Tumor cell with heavy melanin pigmentation (H&E stain, 100×)
Histological cell type: Epitheloid cells, level of invasion (Clarkes Method)—Stage IV (Invasion of reticular dermis). There was lymphovascular invasion. A few microscopic satellitosis were noted. We reported this as NM of the heel.
DISCUSSION
MM is a highly aggressive tumor of melanocytic origin. Foot and ankle lesions comprise 3–15% of all cutaneous MMs.[2] Predicting the survival and recurrence in localized melanoma requires a multivariate approach.[3]
Clinically, when small, nodular lesions with recurrence are noted, other soft tissue lesions such as nodular facitis, neurofibroma, and low-grade fibromyxoid sarcoma should be look for.[4] Melanoma of the foot is frequently misdiagnosed, especially when lesions are small, amelanotic, and within the nail unit. Melanomas in acral locations account for only around 1–7% of all cutaneous melanomas in Caucasians, but they are significantly higher in Asians.[5]
NM is characterized by a prominent vertical component to the invasion of the tumor when viewed under the microscope.
Clinically, the most common symptoms are change in the size of the lesion, bleeding change in color, and change in lesion form to becoming raised, irregular, and nodular. The duration of lesions before diagnosis is relatively short, ranging from a few months to two years. In our case, the tumor rapidly increased in size with secondary changes.
As per histological features, melanoma is of various subtypes: superficial spreading melanoma (SSM), NM, lentigo malignant melanoma (LMM), and acral lentiginous melanoma (ALM).[678]
Among these, the NM is the second most common subtype of melanoma, accounting for approximately 15–30% of all melanomas. The duration of lesions shows rapid evolution. It may takes over several weeks to months. Most of the time, it can be de novo, rather than in a preexisting nevus. It typically presents as a dark blue–black or blue–red raised lesion; however, 5% are amelanotic.
The diagnosis of MM requires several factors to be evaluated. These are location of the lesion, histological type of melanoma, presence of ulceration, infiltration of vessels, tumor thickness, tumor lymphocytic invasion, surgical resection margins, mitotic count etc. In addition, the presence of necrosis, regression, and tumor growth along nerves should be commented on.
The lymph node status is an important factor for prognosis. The number of metastatic nodes, the total number of resected nodes, and perinodal spill of tumor should be properly mentioned in the report. The pathologic report should include the Breslow thickness, ulceration, Clark level, surgical margins, a satellitosis, and regression. It is well known that a high tumor thickness (Breslow depth), the histological ulceration state of the primary melanoma, and increased mitotic rate are associated with a poorer prognosis.[9] Early recognition and diagnosis can significantly improve prognosis.
The immunohistochemistry for S-100 protein, HMB-45, and Melan-A are useful immunomarkers to identify melanocytes and characterize melanomas.[10] Evidence of tumors in regional lymph nodes is a poor prognostic sign. The overall melanoma accounts for less than 5% of skin cancer cases. However, it causes more than 75% of skin cancer deaths.
Foot melanoma is often treatable in the early stages. NM has a poor prognosis because of its vertical growth pattern and it tends to be thick when diagnosed. It often carries a poor prognosis related to its significant tumor volume and early distant metastasis.
In our case, clinically it was stage I melanoma. The treatment given was wide excision surgery to remove the tumor, as well as a margin of normal skin around it. Reconstruction on the part of the heel by local flaps was done with sural graft with split-thickness skin grafting. The patient was followed for six months, and there was no evidence of any recurrence or metastasis. She was advised long-term follow-up. The surgical excision and reconstruction on the part of the foot by local flaps are usually used in the distal third of the foot. Adjuvant chemotherapy and radiation therapy may also be considered in patients with stage IIB–III melanoma, because they have a high risk of recurrence.[11]
CONCLUSION
MM with a prominent nodular growth presented at the acral site showed rapid progression. We are presenting this case for its clinical, histopathological, and surgical management.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/ have given his/ her/ their consent for his/ her/ their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Survival of patients with primary pedal melanoma. J Foot Ankle Surg. 2003;42:193-8.
- [Google Scholar]
- Melanoma of the hand and foot: Epidemiological, prognostic and genetic features. A systematic review. Br J Dermatol. 2012;166:727-39.
- [Google Scholar]
- Prognostic factors in patients with localized primary cutaneous melanoma. Acta Dermatovenerol Alp Pannonica Adriat. 2012;21:27-31.
- [Google Scholar]
- Low grade fibromyxoid sarcoma presented with local recurrence and an extensive foot deformity. J Clin Diagn Res. 2012;6:1070-72.
- [Google Scholar]
- Benign pigmented lesions and malignant melanoma. In: Elder DE, Elenitasas R, Rosenbach M, Murphy GF, Rubin AI, Xu X, eds. Lever’s Histo-Pathology of the Skin (11th ed.). Philadelphia: Wolters Kluwer; 2014. p. :853-968.
- [Google Scholar]
- Melanocytic tumours. In: LeBoit PE, Burg G, Weedon D, Sarasin A, eds. Skin Tumours. Lyon: IARC Press; 2006. p. :49-120.
- [Google Scholar]
- Superficial spreading and nodular melanoma are distinct biological entities: A challenge to the linear progression model. Melanoma Res. 2012;22:1-8.
- [Google Scholar]
- Histologic criteria for diagnosing primary cutaneous malignant melanoma. Mod Pathol. 2006;19(Suppl 2):S34-40.
- [Google Scholar]
- Evidence and interdisciplinary consense-based german guidelines: Diagnosis and surveillance of melanoma. Melanoma Res. 2007;17:393-9.
- [Google Scholar]
- Diagnosis and treatment of malignant melanoma of the foot. Foot Ankle Int. 2006;27:696-705.
- [Google Scholar]






