Translate this page into:
Self-involution of a Solitary Keratoacanthoma: A Case Report with Photographic Documentation
Address for correspondence: Dr Stephanie Saavedra-Portales, Department of Dermatology, Faculty of Medicine, University of Chile, Stephanie, Santos Dumont 999, Independencia-Santiago, Chile. E-mail: stephanie.saavedra@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Keratoacanthoma (KA) is a common and distinctive cutaneous neoplasm that behaves in a benign fashion, displaying rapid growth followed by spontaneous involution. Clinical and histological examinations are essential to confirm this diagnosis, although differentiating KA from squamous cell carcinoma is often difficult. In general, complete surgical excision is a standard of care for solitary KAs; however, the conservative approach could be considered in some selected situations.
We present the case of a 59-year-old female patient who presented with a KA, on a high-risk area, displaying self-involution after undergoing a biopsy. This is one of the few cases in the literature in which spontaneous resolution process was photographically documented with good cosmetic results.
Keywords
Keratoacanthoma
squamous cell carcinoma
tumor
Keratoacanthoma is a unique skin tumor characterized by rapid growth followed by spontaneous involution. This case report illustrates this special behavior, providing good photographic evidence of the spontaneous resolution process.

INTRODUCTION
Keratoacanthomas (KAs) are common epidermal tumors that tend to occur on sun-exposed sites in light-skinned persons of middle age or older.[1] It has several clinical variants, but the most common form of KA is the sporadic and solitary one.[2] Its clinical presentation is characterized by a firm, flesh to pink-colored, crater-like nodule with a central keratotic plug.[3] Nevertheless, the essential clinical characteristic of solitary KA is its self-limiting course, with a rapid enlargement and subsequent spontaneous regression,[4] evolving in three clinical stages: proliferative, maturation or stabilization, and regression. The process from origin to spontaneous resolution usually occurs within 4–6 months.[5] However, despite these characteristics, it could be a challenge, for the clinician, to make a clear distinction between a KA and a squamous cell carcinoma (SCC).[6]
Although KAs are common and spontaneous resolution is well recognized, case reports with photographic documentation of their self-resolution are few.[6]
We present a case with an impressive series of clinical photographs documenting the self-involution of a solitary KA.
CASE HISTORY
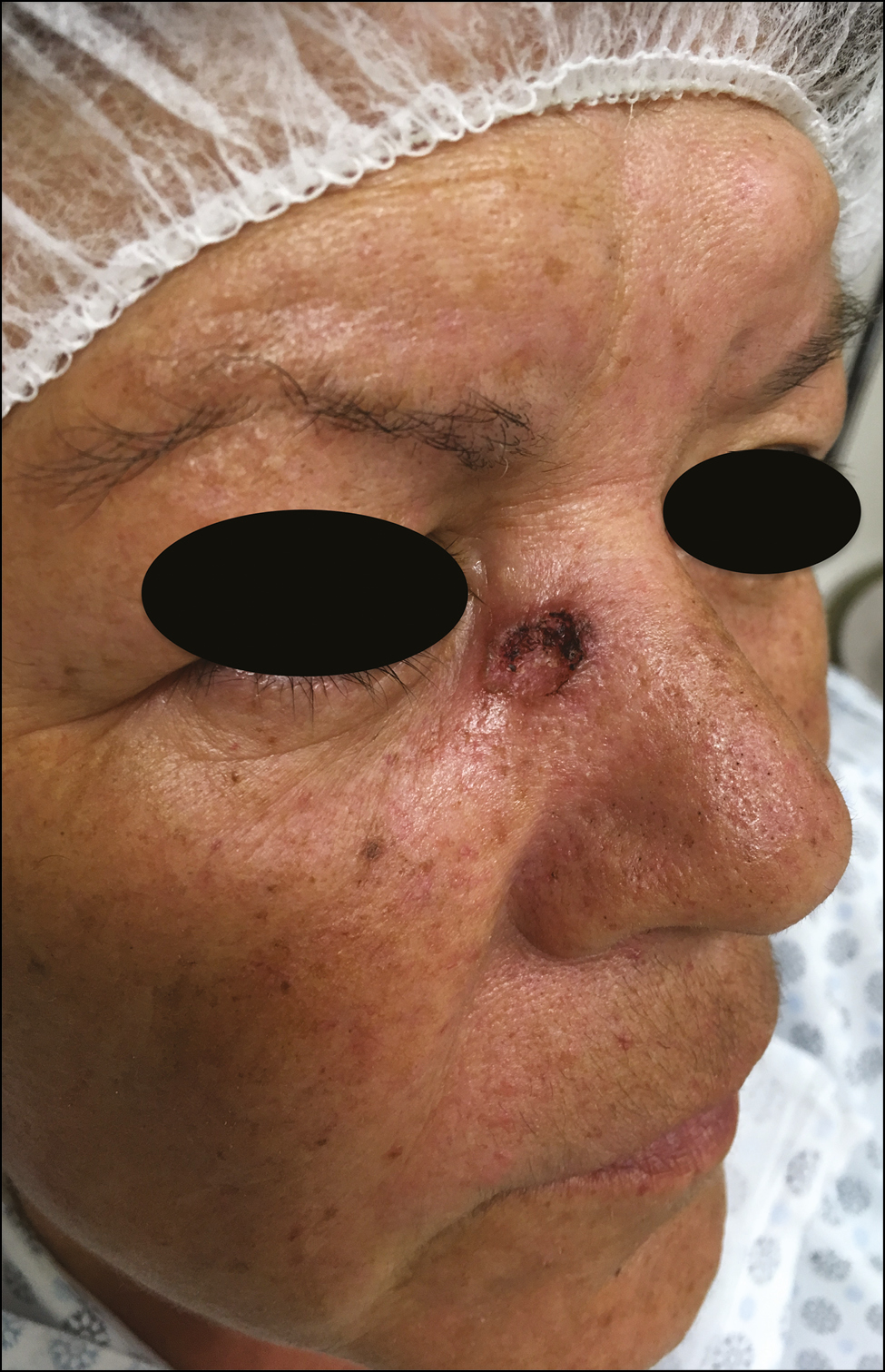
In August 2018, a 59-year-old previously healthy woman presented in our Medical Center with an 8-week history of a rapidly enlarging and asymptomatic nodule on the inner right canthus. Physical examination revealed the presence of a dome-shaped pink nodule measuring 15 mm in diameter, with a central keratin plug and hematic crust, located between the right nasal side wall and the ipsilateral inner canthus [Figure 1]. Dermoscopic examination revealed blood spots with keratinizing pearls in the center and peripheral hairpin vessels.

- Eight weeks after the occurrence. Dome-shaped and crateriform tumor located on the inner right canthus
One month prior to the consultation at our center, the patient had undergone an incisional biopsy, the histological examination of which reported: Histopathological architecture suggesting probable Keratoacanthoma; well-differentiated Squamous cell carcinoma cannot be ruled out [Figure 2].
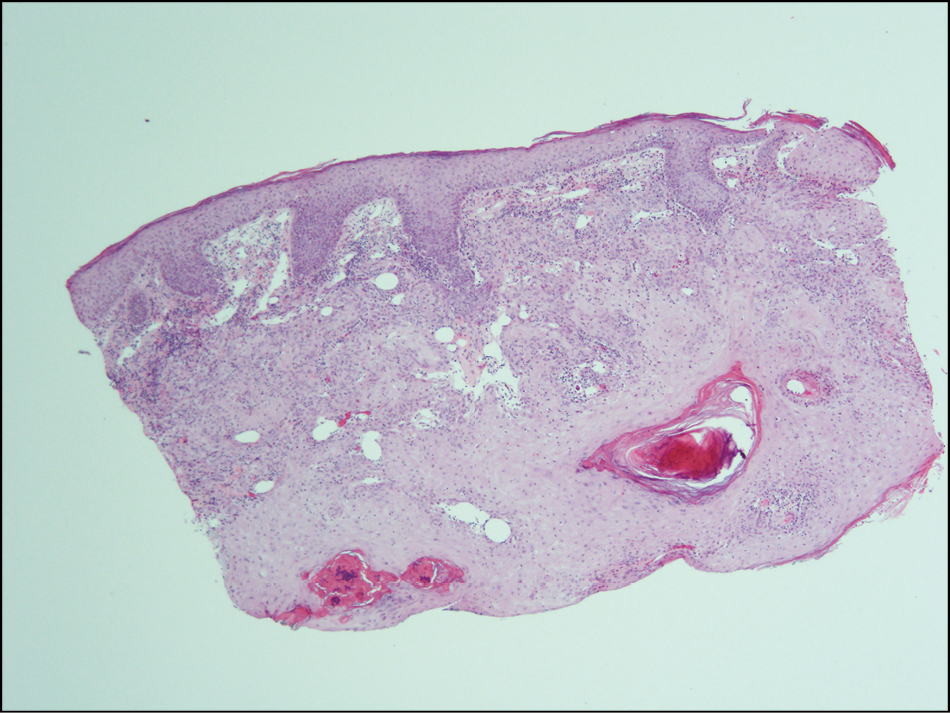
- Histopathologic examination of an incisional biopsy specimen (Hematoxylin and Eosin stain, ×10)
Given this result, the patient was programmed for complete surgical excision in October 2018. However, by the time of the programmed surgery, the tumor showed spontaneous and almost complete regression [Figure 3]. Accordingly, the diagnosis of KA was made and a “watch and wait” policy was implemented, with monthly clinical and dermoscopic checks-ups. In December 2018, 6 months after the occurrence, the tumor completed self-involution, leaving only a small flat scar [Figures 4 and 5].
- Sixteen weeks after the occurrence. Spontaneous incomplete regression of the tumor
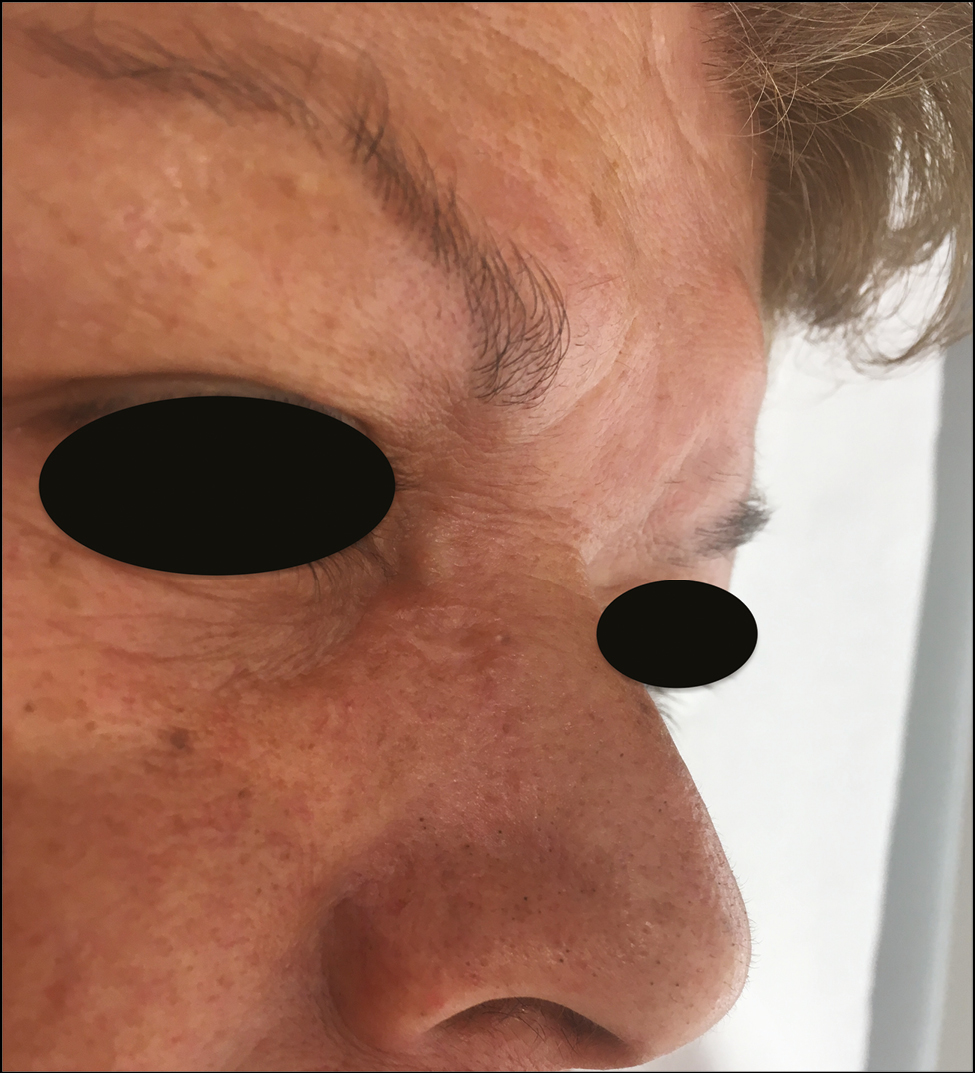
- Twenty-four weeks after the occurrence. Complete self-resolution stage
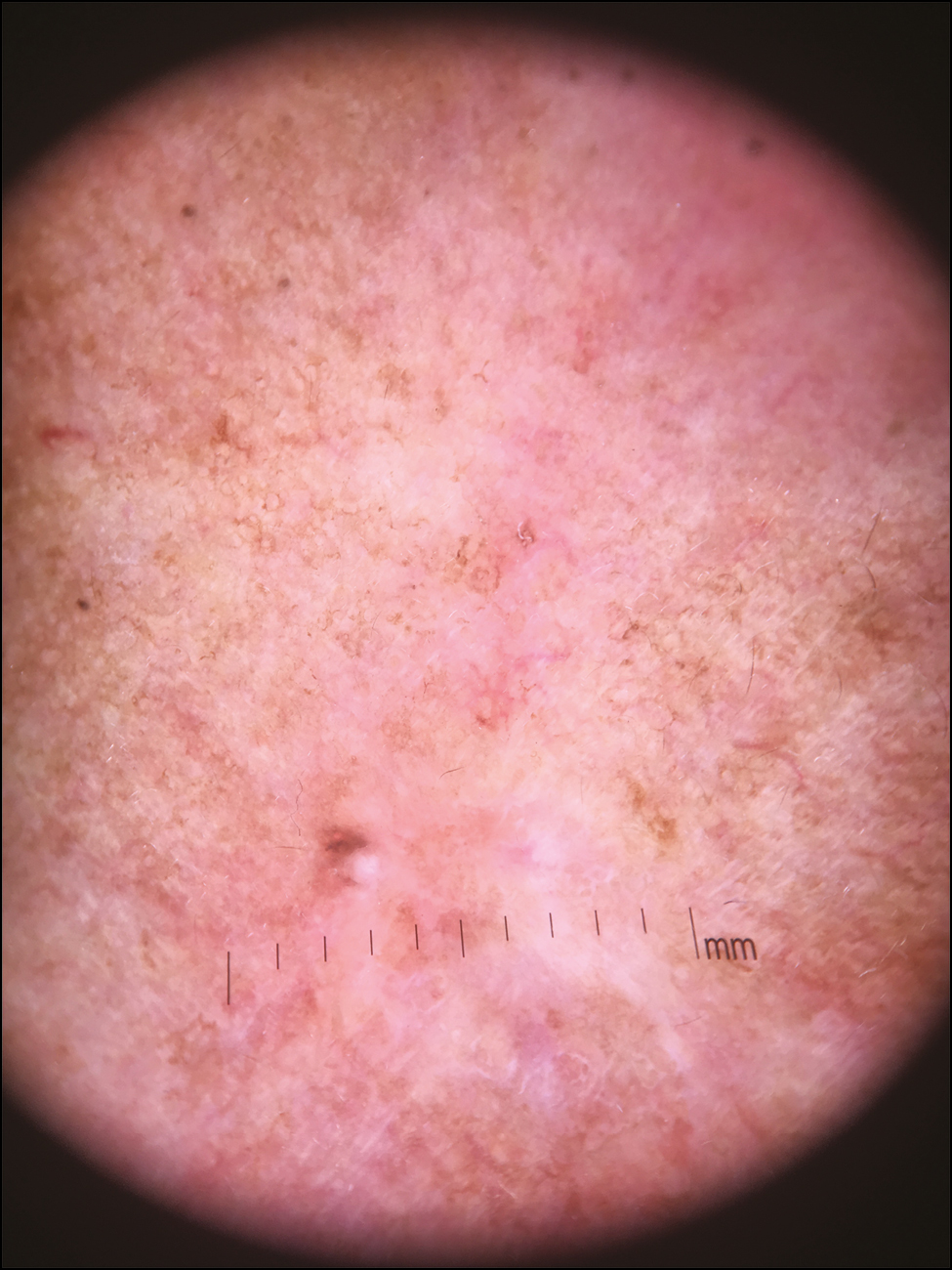
- Dermoscopic evidence of complete self-resolution stage, showing a white scar area
The patient continues to have periodic medical controls, with no evidence of recurrence to date.
DISCUSSION
Although KA was first described by Sir Jonathan Hutchinson in the late 1880s as “crateriform ulcer of the face,”[7] its epidemiology, histopathological diagnostic criteria, prognosis, and treatment guidelines remain controversial. The most common concern is related to its borderline position between malignancy and benignity.[25]
Given this controversy, and because a clear distinction between SCC and KA cannot always be made on clinical or histologic grounds, KA should best be regarded as a subtype of SCC and should be treated accordingly.[5]
Observation is not usually the preferred option, despite some published cases showing spontaneous resolution with good cosmetic results.[89] Wait-and-see management should only be used, after a careful risk and benefit assessment, in patients with a clinically and histopathologically typical KA with no SCC component, for whom complete resection is difficult because of the anatomical location and/or poor general condition.[10] Prompt excision, either conventional or by Mohs surgery, should be considered the treatment of choice for solitary KAs.[5]
The case presented illustrates the self-resolution of a KA located in a high-risk area, showing an excellent cosmetic result.
Despite the special clinical characteristic of KA, with a self-limited course, of rapid enlargement and spontaneous regression,[10] we believe that in our case, the incisional biopsy could probably help in accelerating this process, given the inflammatory response produced by it.
This case demonstrates the role of a wait-and-see policy when the lesion clearly behaves in a KA-like fashion. Despite the outcome of our case, we strongly agree that early surgical treatment must remain the gold standard of management for solitary KAs.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Natural course of keratoacanthoma and related lesions after partial biopsy: Clinical analysis of 66 lesions. J Dermatol. 2015;42:353-62.
- [Google Scholar]
- Keratoacanthoma: A clinico-pathologic enigma. Dermatol Surg. 2004;30:326-33; discussion 333.
- [Google Scholar]
- Spontaneous resolution of a giant keratoacanthoma penetrating through the nose. Clin Exp Dermatol. 2011;36:369-71.
- [Google Scholar]
- Morbid growths and tumours. I. The “crateriform ulcer of the face,” a form of acute epithelial cancer. Trans Pathol Soc Lond. 1889;40:275-81.
- [Google Scholar]
- Self-involution of giant keratoacanthoma on the tip of the nose. Case reports. Plast Reconstr Surg. 2003;111:1560-61.
- [Google Scholar]
- Advances in histopathological diagnosis of keratoacanthoma. J Dermatol. 2017;44:304-14.
- [Google Scholar]





