Translate this page into:
The Closure of Nose Piercing Site Successfully Managed with Skin Grafting: A Case Series of Three Patients
Address for correspondence: Dr. Yogesh Bhingradia, Shivani Skin Care and Cosmetic Clinic, Sarthi Doctor House, Fourth Floor, Hirabag, Varachha Road, Surat, Gujarat, India. E-mail: yogeshbhingradia@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Historically, nose piercing was considered as the symbol of elegance and sometimes also associated with regional ritual. In modern civilization, there has been a decreasing trend to wear nose rings and some people demand for its closure. Herein, we report a case series of three patients who were successfully managed with full-thickness skin grafting for the closure of nose piercing site.
Keywords
Full-thickness
nose piercing
skin grafting
For the closure of nose piercing site, full-thickness skin grafting is the good alternative rather than primary wound closure

INTRODUCTION
The word “piercing” derives from the English verb “to pierce,” which means to transfix and this is a willful and somewhat semi-permanent procedure that has an inherent risk of infection and scarring.[12] Nose piercing is the procedure by which a needle penetrates the nostril, nasal septum, or nasal bridge to form an opening usually to wear jewelry, hence also recognized as nose-jewel. Of the different types of nose piercing, the nostril piercing is most widespread. This method was implemented for symbolic or beautification purposes, which was established more than 4000 years ago in the Middle East, and then migrated to India in the 1500s and reached Western civilization by the twentieth century.[3]
In modern era, this trend of nose piercing has been declined. Most of the females do not want it for a cosmetic purpose as it leaves scar if a ring is not worn for a long time, or sometimes the piercing hole becomes widened due to mismanagement or overweighed ornaments. Quite a while back, there has been an increased tendency of the closure of nose piecing in dermatological settings. Most of the dermatologists perform a primary wound closure technique for the closure of nose piercing site. We have established an extraordinary treatment protocol for the closure of nose piercing site with full-thickness skin grafting (FTSG) technique. From this case series, we highlight the skin grafting technique as a novel method for the closure of nose piercing site and its advantages over the primary closure techniques.
CASE SERIES
Treatment protocol
Personal history of hypertension, diabetes mellitus, and smoking was taken in all patients as smoking compromises oxygenation of tissue due to the vasoconstrictive effect of nicotine. Written informed consent was obtained from all patients. After cleaning with diluted betadine, the recipient site was anesthetized by local infiltration. The nose piercing site scar was excised that includes piercing site in elliptical fashion with depth (1–1.2 mm), which was removed and created raw area for the graft. The same size of full-thickness graft in terms of surface area and depth was harvested with a scalpel from the retro auricular site (donor site) [Figure 1]. Once harvested, the graft was handled in atraumatic fashion. Donor site wound was closed with simple interrupted suture. The harvested graft was placed over the recipient area and sealed with surgical glue which would be shed after 6–7 days. The donor site was covered with bandages after the procedure. As post-operative care, patients were prescribed analgesics and antibiotics for 5 days. The patients were instructed to avoid trauma to the site and strenuous activity for at least 2 weeks after surgery. Patients were followed up at weekly interval till two visits and then monthly till complete healing.

- Showing retro-auricle donor area from where graft was harvested
Case 1
A 28-year-old female presented with a complaint of depressed scar at nose piercing site. Clinical examination revealed an oval-shaped scar with a depth of 1.5 mm with altered texture at the base. The patient was much satisfied after skin grafting. Pre-and post-procedure pictures of the nose piercing site are shown in Figure 2. With same protocol of skin grafting technique, we have treated two more females, and demography and procedural details for them are well summarized in Table 1.

- (A) Pre-treatment picture of nose piercing site. (B)The planned direction of excision at nose piercing site. (C) Excision at nose piercing site. (D) Full-thickness skin grafting at nose piercing site. (E) Post-operative view after closure of nose piercing site
| Case | Age (years) | Clinical examination | Final cosmetic outcome |
|---|---|---|---|
| 2 | 34 | A single round-shaped hole with a surface diameter of 2.5 mm was observed | After procedure, nose piercing area was completely healed and closed after skin grafting leading to improved cosmesis [Figure 3] |
| 3 | 34 | A history of widening of nose piercing site since 4 years. She was operated in the past by primary wound closure technique after ablating the margin by a plastic surgeon at Mumbai but somehow the result was not much satisfying. On clinical examination, we found a linear scar with bewelling at the nose piercing site | After 3 months of surgery, the piercing area was completely sealed without any sign of scarring |
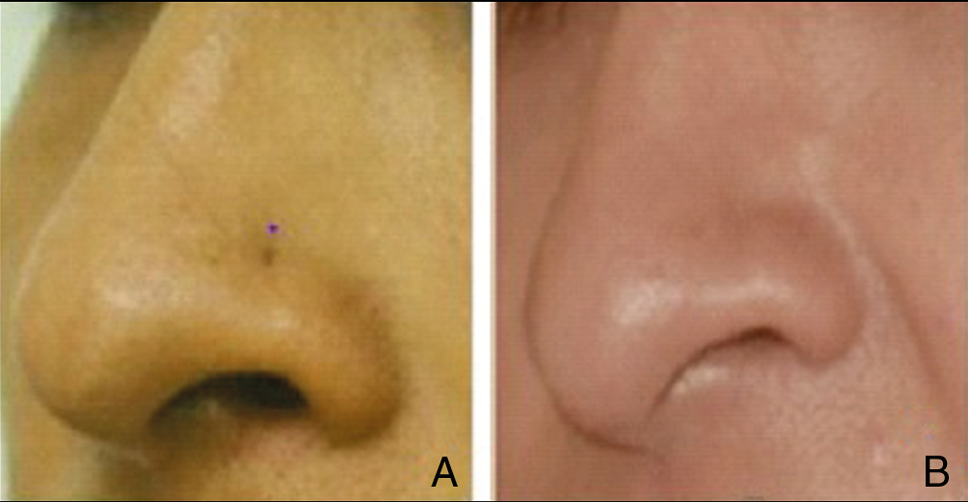
- (A) Pre-treatment view of nose piercing site. (B) Post-treatment cosmetic improvement after 3 months of surgery
DISCUSSION
A skin graft is a cutaneous tissue and not cutaneous free tissue transfer that is separated from a donor site and transplanted to a recipient site.[4] In dermatological practice, skin graft has been mainly used for skin infections, deep burns, large and open wounds, skin cancer surgery, bedsores, and non-healing ulcers. Utilization of this modality in the closure of nose piercing is indeed a novel concept. When used appropriately, FTSG makes for a simple and aesthetically acceptable reconstruction option for nasal defects.[5] This is the first reported case series in the literature, in which closure of nose piercing site is successfully done with skin grafting.
Any piercing itself is regarded as a type of wound. Hence, in day-to-day practice, primary wound closure technique is widely accepted in the closure of nose piercing site. It is the fastest type of closure and is also termed as healing by primary intention. In the primary intention method, surgical wound closure aids the biological event of healing by connecting the wound edges.[6] Since the last 200 years, skin grafting has evolved as a fundamental part of the armamentarium of the reconstructive surgeon. Plasmatic imbibitions (nourishment of graft by absorbing the nutrients via diffusion), inosculation and capillary ingrowths (new blood vessels begin growing from the recipient area into the transplanted skin within 36 h), and revascularization (newly formed vascular connections continue to differentiate into afferent and efferent vessels) are three main steps involved in the mechanism of grafting.[7] Sites in which grafts are most commonly used include the nasal tip, dorsum, ala, and sidewall as well as the eyelids and the ears.[8]
FTSGs consist of complete epidermis and dermis. Usually, they are used to resurface small, uncontaminated, well-vascularized wounds due to their confined size. They are also precious for the reconstruction of defects where better cosmetic improvement or a durable skin cover is expected.[9] The presence of a well-vascularized bed, meticulous attention to graft selection, and atraumatic handling of graft are necessary requisites to ensure graft intake and survival.
The skin of the lower third of the nose is thick and composed of sebaceous glands, unlike the thin skin of the upper two-thirds.[10] This inherent thickness makes it difficult to rotate a local flap into position, making skin grafting with proper donor site selection an excellent reconstructive option. Weathers et al.[5] have concluded in their study that skin grafting in nasal reconstruction can deliver superior aesthetic results and could become a go-to reconstructive procedure for small, shallow defects of the nasal region.
Some upsides associated with FTSGs are that they undergo less contraction on healing, better aesthetic result, and they do not alter the architecture of the recipient site. Bearing the mentioned merits in mind and further adding our practical experience, we hypothesized that skin grafting might become a most privileging modality in the closure of nose piercing site.[79]
In the case of primary closure, the wound heals on the 7th day after removal of stitches, but there is a chance of separation of wound-scar due to force applied by underlying cartilage. In the case of grafting, the grafted skin heals by the end of 7–10 days, but the texture of the skin can be either elevated or depressed at 7–10 days and that becomes normal gradually as the grafted skin is accepted well by the recipient site. Sometimes, there are chances of elevated scars at the end of 4–6 weeks, which may require ablation of the elevated skin with the help of CO2 laser under topical anesthesia. Of interest, the most relevant fact about this method is that this skin grafting is associated with minimum scarring when compared with primary closure techniques.
The major drawback of skin grafting is that it should be performed under trained surgeons only, and careful handling is necessary to maximize graft survival. Other concern with using FTSGs is the potential for color mismatch and contour irregularity, which can be overcome by insetting the graft under appropriate tension and proper selection of donor site.
CONCLUSION
The FTSG is easy to perform, reliable, and minimally invasive procedure for the closure of nose piercing. In this case series, all three patients had satisfactory cosmetic improvement after the closure of nose piercing site with skin grafting.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Sequential survey of body piercing and tattooing prevalence and medical complication incidence among college students. Arch Pediatr Adolesc Med. 2007;161:1219-20.
- [Google Scholar]
- Body art (body piercing and tattooing) among undergraduate university students: “Then and now.”. J Adolesc Health. 2008;42:201-3.
- [Google Scholar]
- Body piercing: Medical consequences and psychological motivations. Lancet. 2003;361:1205-15.
- [Google Scholar]
- Grafts in dermatologic surgery: Review and update on full- and split-thickness skin grafts, free cartilage grafts, and composite grafts. Dermatol Surg. 2005;31:1055-67.
- [Google Scholar]
- Full-thickness skin grafting in nasal reconstruction. Semin Plast Surg. 2013;27:90-5.
- [Google Scholar]
- Wound closure technique. Medscape. Available from: https://emedicine.medscape.com/article/1836438-overview.
- [Google Scholar]
- Full-thickness skin grafts. Medscape. Available from: https://emedicine.medscape.com/article/876379-overview#showall.
- [Google Scholar]
- Full thickness skin grafts in SP [internet]; updated 2020 January 9. Treasure Island, FL: Stat Pearls Publishing; 2020.
- Full thickness skin grafts. Available from: https://www.intechopen.com/books/skin-grafts-indications-applications-and-current-research/full-thickness-skin-grafts
- [Google Scholar]
- The quantification and distribution of nasal sebaceous glands using image analysis. Aesthetic Plast Surg. 1996;20:303-9.
- [Google Scholar]





