Translate this page into:
Role of Trichoscopy in the Management of Tinea Capitis in Two Infants: A Case Report
Address for correspondence: Dr Deepika Pandhi, Department of Dermatology and STD, University College of Medical Sciences and Associated GTB Hospital, Delhi 110095, India. E-mail: deepikapandhi@rediffmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
As tinea capitis rarely affects infants, early trichoscopic diagnosis facilitates timely institution of appropriate therapy. We report a 10-month-old female presenting with mixed pattern tinea capitis and coexisting tinea faciei wherein trichoscopy showed perifollicular scaling, comma hair, corkscrew hair, and horse-shoe hair. Case 2 was a 3-month-old female with gray patch tinea capitis, corroborated by the presence of perifollicular scaling, comma hair, corkscrew hair, and prominent telangiectasia on trichoscopy. Both cases were successfully treated with tablet fluconazole (5 mg/kg) for 6–8 weeks.
Keywords
Comma hair
corkscrew hair
infantile tinea capitis
trichoscopy
Infantile tinea capitis is a rare entity usually diagnosed by KOH examination and fungal culture, and trichoscopy is a recent adjuvant diagnostic modality. Comma hair, corkscrew hair, horse-shoe hair, and perifollicular scaling are trichoscopic signs of tinea capitis that were present in our cases. Both the cases responded well to fluconazole. Therefore, we recommend trichoscopy, especially when the disease is suspected in unusual age groups or has an atypical presentation

INTRODUCTION
Tinea capitis caused by an invasion of hair shaft and scalp skin by dermatophytes is common among pediatric population but remains a rarely encountered entity in infants.[1] The varied presentation further delays the diagnosis and the traditional methods for diagnosis. Direct microscopy has varied results and fungal culture takes several weeks to confirm the diagnosis. Non-invasive in vivo diagnostic modalities include trichoscopy; it has been employed for making rapid diagnosis of tinea capitis. Various studies have elaborated perifollicular scaling (95%), short broken hair (74–100%), comma hair (26–66%), corkscrew hair (13–80%), zigzag hair (25%), black dot (13–65%), horse-shoe hair (16.32%), i-hair, and morse code hair as trichoscopic features of tinea capitis.[2345]
Two genera (Trichophyton and Microsporum) are responsible for tinea capitis. Gold standard treatment is oral (suspension) griseofulvin 25 mg/kg/day, although fluconazole is also being used.[1]
CASE REPORTS
Case 1
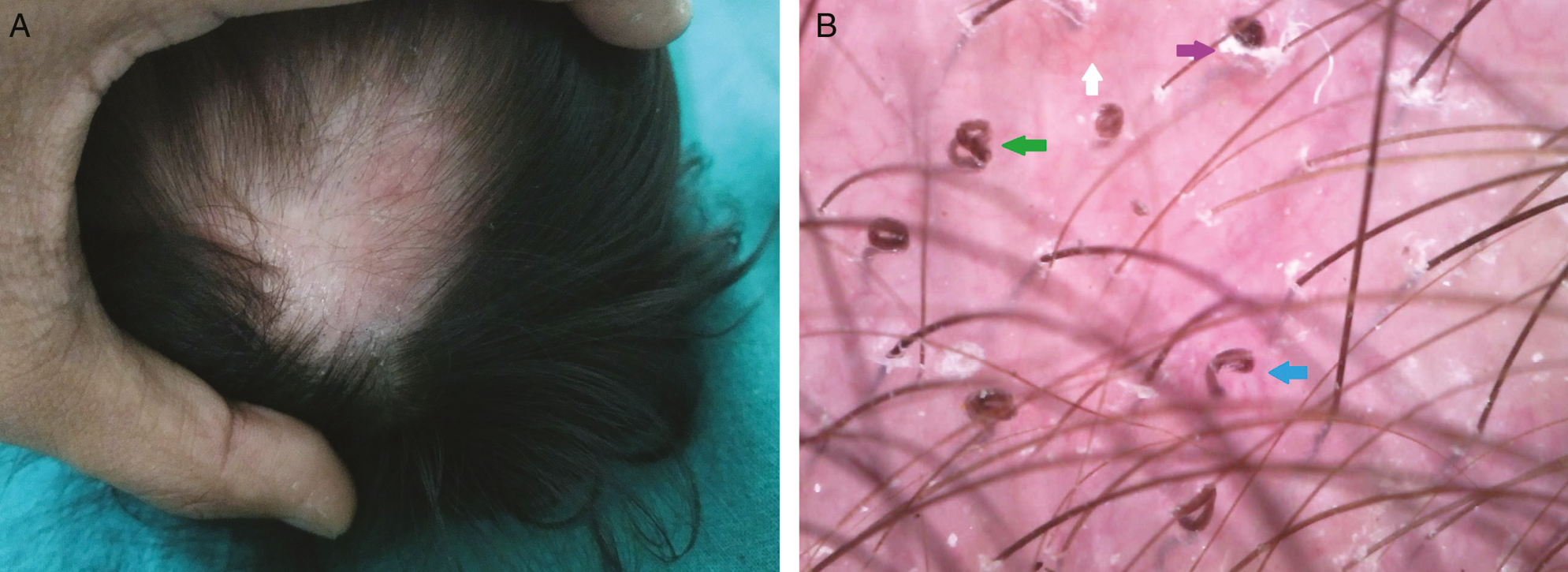
A 10-month-old girl presented with multiple, scaly, erythematous alopecia patch over the scalp [Figure 1A] of 2 months duration. Mother reported mustard oil application over scalp and treatment of sibling with terbinafine for recurrent gray patch tinea capitis (endothrix positive). Scalp examination of the infant showed mixed variant (black dot and gray patch) tinea capitis without regional lymphadenopathy. Endothrix pattern was seen in 10% KOH mount, and no growth was evident on culture. Scalp lesion was associated with tinea faciei. Trichoscopy (AM7013MZTS Dino-Lite Premier, AnMo Electronics Corporation, Taiwan, China) showed perifollicular scaling, hair dust, comma hair, corkscrew hair, and horse-shoe hair [Figure 1B]. Patients were treated with 2% miconazole cream and tab. fluconazole 30 mg twice a week for 8 weeks with complete resolution of the lesions.

- A. Clinical picture showing mixed variant: black dot and gray patch tinea capitis. B. Its trichoscopy (70× magnification, polarized mode) shows perifollicular scaling (violet arrow), comma hair (blue arrow), corkscrew hair (green arrow), and horse-shoe hair (red arrow)
Case 2
A 3-month-old girl presented with single erythematous scaly alopecic patch over the vertex [Figure 2A] of 20 days duration. Gray patch tinea capitis without lymphadenopathy was evident and 10% KOH mount revealed ectothrix variant. Her trichoscopy shows perifollicular scaling, comma hair, corkscrew hair, and prominent telangiectasia [Figure 2B]. No growth was seen in Sabouraud dextrose agar (SDA) culture media. The patient was treated with tab. fluconazole 20 mg twice a week and ketoconazole shampoo for 6 weeks.
- A. Clinical picture showing gray patch tinea capitis. B. Its trichoscopy (70× magnification, polarized mode) shows perifollicular scaling (violet arrow), comma hair (blue arrow), corkscrew hair (green arrow), and prominent telangiectasia (white arrow)
DISCUSSION
Tinea capitis is an invasion of hair shaft and contiguous scalp skin by dermatophyte fungus, predominantly affecting children aged 8–10 years, belonging to low socio-economic status. It rarely affects infants and only a few case reports have been published.[16789] The worldwide estimated prevalence of tinea capitis is 7.1–47.5% and that of India is 0.5–10%.[2]
Tinea capitis has variable clinical presentations: asymptomatic carrier state, non-inflammatory variants, inflammatory variants, and mixed pattern (new variant).[2] Case 1 belonged to the mixed variant (recently classified as variant of tinea capitis) and case 2 belonged to the gray patch which is the second most common clinical types of tinea capitis.
Tinea capitis is mainly diagnosed by microscopy (10% KOH mount) and culture, but non-invasive tests such as woods lamp (fluorescence in small spore ectothrix) and trichoscopy can aid in early diagnosis. Trichophyton violaceum (86.7%) is the predominant species isolated in north India.[2] Significantly, none of our cases shows growth in SDA culture media.
Trichoscopy is defined as dermoscopy of hair, which is a rapid and non-invasive tool. In 2008, Slowinska et al.,[10] for the first time, described comma hair as trichoscopic signs of tinea capitis, due to Microsporum canis. Subsequent studies revealed various trichoscopic features of tinea capitis.[2345] Tinea capitis cannot be diagnosed by a single trichoscopic feature but requires a combination of features like perifollicular scaling, along with any type of dystrophic hair or broken hair for a specific diagnosis of tinea capitis.[234] Perifollicular scaling, comma hair, and corkscrew hair were common trichoscopic features of tinea capitis in both infants. In addition to this, horse-shoe hair in case 1 and prominent telangiectasia in case 2 were detected. Kumar et al.[2] also described horse-shoe hair as a trichoscopic sign of tinea capitis. It is defined as U-shaped hair with arms of equal length that could be explained by endothrix invasion by Trichophyton (T. violaceum and T. mentagrophytes complex) species, resulting in hair shaft weakness and subsequent bending of hair shaft or simply an exacerbation of the comma hair. They described it in both the non-inflammatory and inflammatory variants of tinea capitis.[2] Apart from this, trichoscopy also aids in differentiation of alopecia due to tinea capitis from other causes of alopecia in this age group [Table 1].[1112]
| Disease entity | Trichoscopic findings |
|---|---|
| Tinea capitis[2] | Perifollicular scaling, short broken hair, comma hair, corkscrew hair, zigzag hair, black dot, horse-shoe hair, i-hair, and morse code hair |
| Alopecia areata[11] | Black dots, yellow dots, exclamation hair, vellus hair, and thin hair |
| Seborrheic capitis[11] | Hidden hair, perifollicular white scales, brown dots, atypical red vessels, and comma vessels |
| Congenital triangular alopecia[11] | Vellus hairs with terminal hairs at the periphery |
| Pityriasis amiantacea[12] | Scales and compact white keratotic material adhering to tufts of hair (asbestos-like scaling) without erythema, “question mark,” and “zigzag” hairs |
None of the previous studies has described trichoscopic features in infants with tinea capitis.[2345]
Endothrix invasion (case 1) causes hair shaft deformation without color impairment resulting in comma hair, corkscrew hair, and horse-shoe hair, whereas ectothrix invasion results in morse code and zig-zag hair.[25]
Griseofulvin and terbinafine are the only FDA-approved drugs in children but no oral antifungals have been approved for the treatment of infantile tinea capitis.[1] These cases are treated with griseofulvin, terbinafine, itraconazole, and fluconazole with variable success rates.[17,9] Our cases responded well to fluconazole (5 mg/kg) along with general measures like avoidance of hair oil and treatment of family member infected with dermatophytes. Furthermore, fluconazole has an advantage of short duration therapy with high efficacy when compared with griseofulvin.[1] Moreover, none of our cases experienced any adverse effect.
Trichoscopy was a handy, useful, bedside tool for the diagnosis of both cases of tinea capitis in infancy, which obviated the need for time taking and low sensitivity investigation like fungal culture (sensitivity 45.7–52.04%).[23] Therefore, we recommend its usage especially when disease is suspected in unusual age groups or has atypical presentation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
None.
REFERENCES
- Tinea capitis in infants: Recognition, evaluation, and management suggestions. J Clin Aesthet Dermatol. 2012;5:49-59.
- [Google Scholar]
- Trichoscopy as a diagnostic tool for tinea capitis: A prospective, observational study. Int J Trichol. 2020;12:68-74.
- [Google Scholar]
- Different trichoscopic features of tinea capitis and alopecia areata in pediatric patients. Dermatol Res Pract. 2014;2014:848763.
- [Google Scholar]
- Trichoscopy as an additional tool for the differential diagnosis of tinea capitis: A prospective clinical study. Br J Dermatol. 2016;175:208-9.
- [Google Scholar]
- Analysis of trichoscopic signs observed in 24 patients presenting tinea capitis: Hypotheses based on physiopathology and proposed new classification. Ann Dermatol Venereol. 2017;144:490-6.
- [Google Scholar]
- A case report of tinea capitis in infant in first year of life. BMC Pediatr. 2019;19:65.
- [Google Scholar]
- Comma hairs: A dermatoscopic marker for tinea capitis: A rapid diagnostic method. J Am Acad Dermatol. 2008;59:S77-9.
- [Google Scholar]
- Relevance of trichoscopy in the differential diagnosis of alopecia: A cross-sectional study from north India. Indian J Dermatol Venereol Leprol. 2016;82:651-8.
- [Google Scholar]
- Dermoscopy as a useful supportive tool for the diagnosis of pityriasis amiantacea-like tinea capitis. Dermatol Pract Concept. 2016;6:63-5.
- [Google Scholar]





