Translate this page into:
Dermoscopic Evaluation of CO2 Laser Treatment in the Scar of Lupus Vulgaris
Address for correspondence: Dr Yasmeen Jabeen Bhat, Postgraduate Department of Dermatology, Venereology, and Leprosy, GMC Srinagar, University of Kashmir, Jammu and Kashmir, India. E-mail: yasmeenasif76@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Lupus vulgaris (LV) is a chronic, progressive, secondary cutaneous form of tuberculosis that heals with scarring leading to cosmetic and psychological morbidity when present on the exposed sites. We hereby report a case of LV over nose complicated by scarring following treatment with anti-tubercular therapy (ATT). Six sessions of fractional CO2 laser resurfacing for the post-treatment atrophic scar resulted in excellent response clinically that was documented dermoscopically.
LV is a chronic, indolent form of cutaneous tuberculosis seen in patients with moderate-to-high immunity that classically presents as papulonodular lesions coalescing to form plaques with areas of progression as well as scarring. Face is a common site including the nose, though septal perforation is rare.[1] The resultant atrophic scarring following ATT may lead to deformity and mutilation along with fibrotic contractures.[2]
Treatment options for managing such scars are limited. Fractional carbon dioxide (10,600 nm) laser resurfacing has been used in the treatment of atrophic scars with varying degrees of success. It is supposed to work by stimulating collagen production in the dermis and by dermal remodeling of collagen fibers.[3]
A 12-year-old child presented with history of elevated lesion over nose since 1 year. It started with a single papule on ventral aspect of nasal tip which gradually enlarged and progressed in due course of time. Patient had no significant history of trauma at the site, systemic symptoms, or past history of pulmonary tuberculosis. However, there was past history of pulmonary tuberculosis in a family member. He had received BCG vaccination at birth.
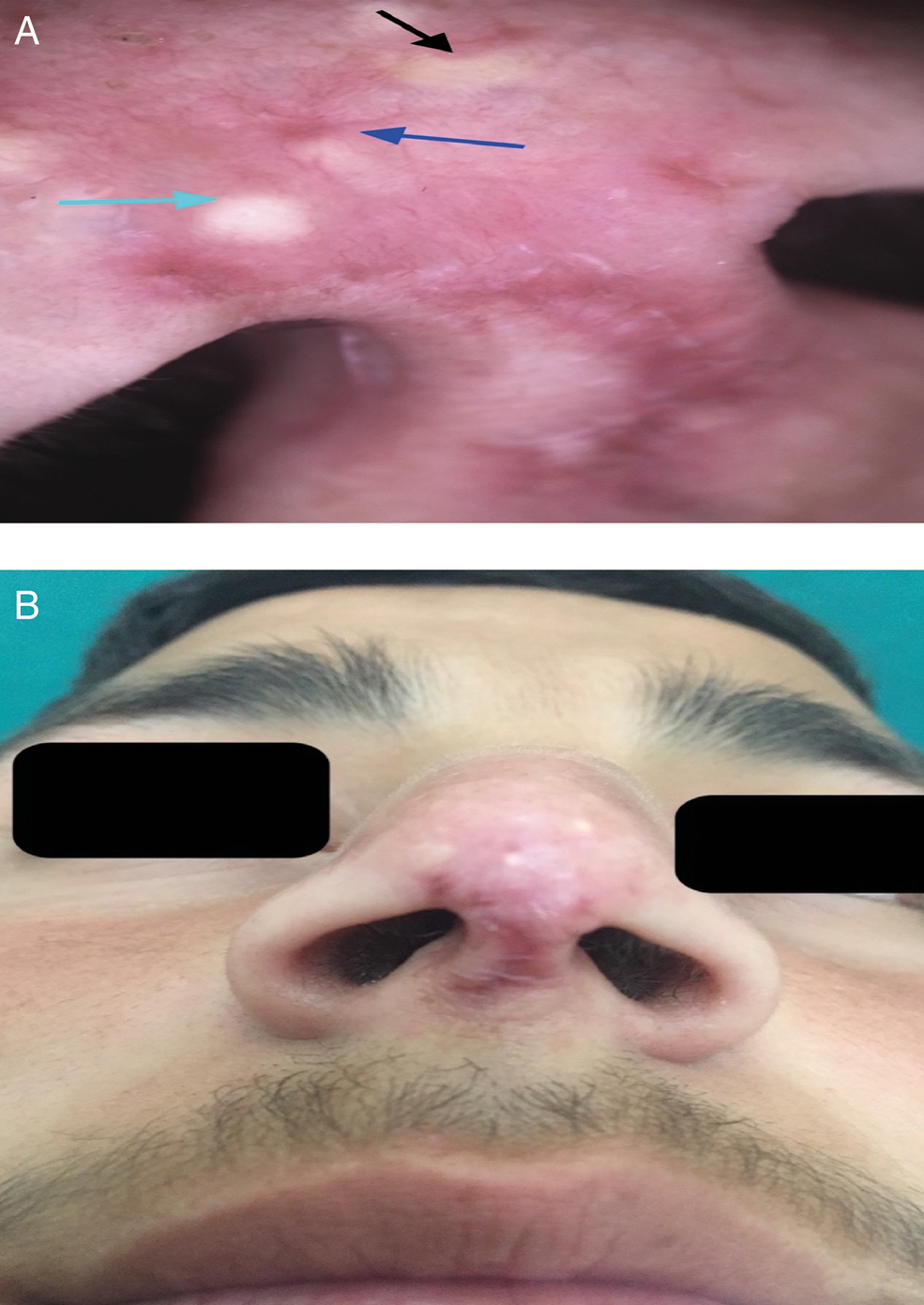
General physical and systemic examination were normal. Cutaneous examination showed well-defined erythematous and mildly scaly plaque of around 3 cm × 2 cm in size, involving right side of nasal tip with central brownish crust [Figure 1]. On diascopy, apple jelly nodules were seen in the center. Patient had firm and non-tender right submandibular lymphadenopathy. Nasal septum, lips, and oral mucosa were normal. Anterior rhinoscopy findings were normal.

- Erythematous plaque on right side of nasal tip with single ulcer at the center. A: Dermoscopy showing intense background erythema (yellow stars), yellowish-orange structureless areas (black arrows), white reticular streaks (green arrows), and linear branching vessels (blue arrow) (DermLite DL3N 10×, polarized mode)
Dermoscopy ruled out verruca vulgaris and showed yellowish to orangish structureless areas, with linear branching vessels, reticular white streaks on an erythematous background favoring granulomatous pathology [Figure 1A]. Erythrocyte sedimentation rate was 30 mm/h. Mantoux test with one tuberculin unit of PPD RT23 was positive with 23 × 18 mm diameter erythema and induration after 48 h. Fine-needle aspiration cytology from the submandibular lymph nodes demonstrated tuberculoid granulomas with acid fast bacilli (AFB). Histopathology from the cutaneous plaque was consistent with LV [Figure 2]. Patient was started on category I ATT, DOTS regimen for 6 months after which he showed remarkable improvement and significant resolution of his lesions with atrophic scarring.
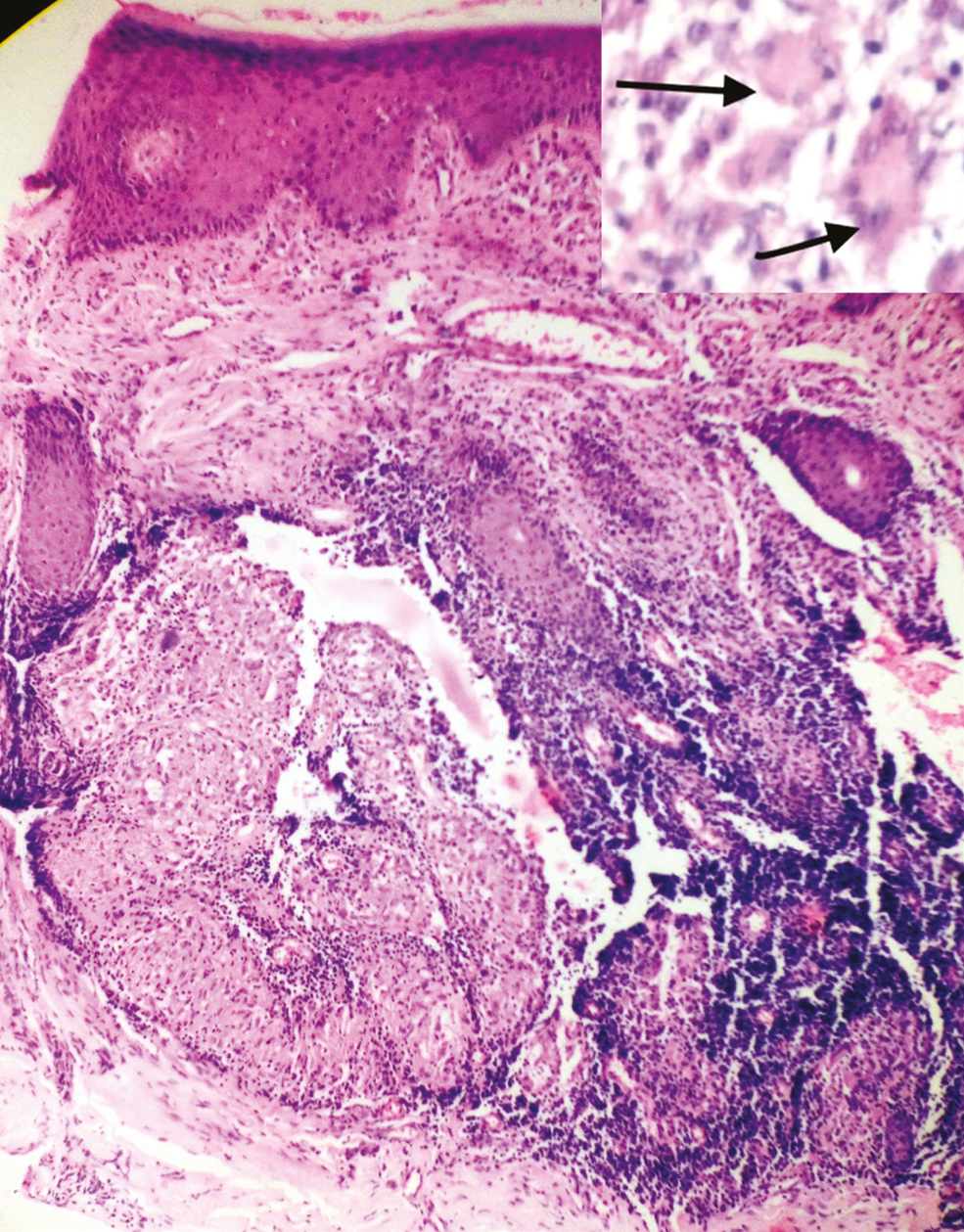
- Photomicrograph showing well-defined epitheloid cell granulomas (H&E 100×). The inset shows Langhans type of giant cells, epitheliod cells, lymphocytes along with inflammatory infiltrate in dermis (H&E 400×)
After 1 year of follow-up post-treatment, in view of an atrophic scar at the site of the lesion, that was cosmetically unpleasant for the patient, fractional CO2 laser resurfacing was planned [Figure 3]. On dermoscopy, atrophy with long arborizing telangectasias on a yellow to golden background and milia-like cyst were seen [Figure 3A].

- Atrophic scar over the nose 1 year post-treatment with ATT. A: Dermoscopy showing prominent structures like atrophy, faint background erythema, milia-like cysts (green arrow), faint yellowish structureless areas (black arrows), and long arborising telangiectasias (blue arrow) (DermLite DL3N 10×, polarized mode)
Fractional CO2 laser sessions were done every 4 weeks for first four sessions (stamped mode, energy 25 mJ/cm2, PPA 64, F 50), and last two sessions were done 6 weeks apart with increased fluence at each session. Improvement of the lesion was noticed without any adverse effects [Figures 4–6]. Post-laser treatment dermoscopic features showed few milia-like cysts and peripheral telangectasia that diminished progressively with the laser sessions [Figures 4A and 5A].
- Mild improvement in the scar after two sessions of fractional CO2 laser. A: Post-laser treatment dermoscopic image showing structures like atrophy, mild erythema with milia-like cysts (green arrow), fainter yellowish structureless areas (black arrows) and long arborising telangiectasias (blue arrow) (DermLite DL3N 10×, polarized mode)

- Moderate improvement in the scar after four sessions of fractional CO2 laser. A: Dermoscopy showing subtle erythema, milia-like cysts (green arrow), and barely visible yellowish structureless areas (black arrows), absence of vessels (blue arrow) (DermLite DL3N 10×, polarized mode)

- Excellent improvement in the scar after six sessions of fractional CO2 laser
Dermoscopy helps in assessing the response to treatment in the granulomatous disorders. Dermoscopy of early plaque of LV shows yellowish orange discoloration in the background along with milia-like cysts and white reticular streaks with numerous broad and long arborizing telangectasias. The resolving plaque of LV shows variety of vascular patterns with peripheral telangectasias and decreased erythema and decreased hue of orange background.[45]
In our case, fractional CO2 laser was used in the management of atrophic scar left after treatment with ATT, six sessions of fractional CO2 lasers were done, 4–6 weeks apart with increased fluence on each session, showing a marked improvement in the lesion. Dermoscopy after laser treatment showed resolving erythema with few peripheral telangectasias and reduced milia-like cysts.
To conclude, fractional laser resurfacing with CO2 laser offers a well-tolerated and effective treatment option in atrophic scars of LV, and dermoscopy offers a good tool for the assessment of treatment response. It may be utilized for scarring left after other granulomatous diseases.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Lupus vulgaris of external nose with septal perforation—A rarity in antibiotic era. Indian J Tuberc. 2010;57:157-9.
- [Google Scholar]
- Mycobacterial diseases. In: Andrew’s diseases of the skin (12th ed.). Philadelphia, PA: Elsevier; 2016. p. :332.
- [Google Scholar]
- The use of fractional laser photothermolysis for the treatment of atrophic scars. Dermatol Surg. 2007;33:295-9.
- [Google Scholar]
- Dermoscopy in general dermatology: A practical overview. Dermatol Ther (Heidelb). 2016;6:471-507.
- [Google Scholar]
- Dermoscopic patterns of common facial inflammatory skin diseases. J Eur Acad Dermatol Venereol. 2014;28:609-14.
- [Google Scholar]





