Translate this page into:
Operative Treatment of Severe Allergic Reactions to Red Tattoo Dye: Presentation and Comparison of Possible Surgical Procedures in Seven Patients
Address for correspondence: Dr. Joerg Laske, Department of Dermatology, University Hospital Dresden, Fetscherstr. 74, Dresden, Germany. Email: joerg.laske@ukdd.de
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Context:
The treatment of allergic reactions to red tattoo dye is challenging in most cases, as local therapy often does not offer long-term improvement and laser therapy is considered relatively contraindicated by many authors owing to the risk of generalized side effects. Therefore, surgical removal of these tattoos is favored; shave excision is the method of choice, particularly for the removal of the entire dye.
Aims:
The aim of this article was to retrospectively analyze the best post-operative outcome after surgical removal of allergic tattoo reactions using different excision techniques.
Materials and Methods:
We compared the different surgical procedures performed on seven patients with single and multiple allergic tattoo reactions treated between 2013 and 2018.
Results:
The best aesthetic results were achieved by superficial ablation of the inflammatory reaction, partially leaving tattoo remains in the skin.
Conclusion:
Based on our experience with this small number of patients, a superficial removal of the tattoo without complete removal of the dye is, in most cases, sufficient to achieve healing. The remaining dye residues seem to be better tolerated by the immune system afterwards. Furthermore, the tattoo is often preserved in large parts.
Keywords
Allergic
reaction
shaving
tattoo
treatment
A superficial removal of the allergic tattoo reaction without complete removal of the dye is, in most cases, sufficient to achieve healing.

INTRODUCTION
The proportion of people with tattoos among the western population of the world has been increasing for decades. Tattoos are particularly popular in the younger age groups. It is estimated that approximately one in five people in Germany has a tattoo.[1]
There are little data on the general frequency of tattoo-associated complications. Kazandjieva and Tsankov[2] found tattoo-associated complications in five of the 234 screened patients. Serup[3] proposed a clinic-based diagnostic algorithm to classify these side effects on the basis of a large cohort of 405 patients with 493 tattoo-related complications. According to this study, allergic reactions are among the most frequent side effects, followed by infections. The reaction to red tattoo dye and its variations are, therefore, almost exclusively allergic reactions. Conservative treatment in these cases is usually frustrating, because success with intralesional triamcinolone has only been reported in isolated cases.[4] The reactions usually subside only after removal of the triggering pigment.
The gold standard for removing non-inflammatory tattoos is by laser. However, complications in the form of generalized eczematous reactions have been described in the laser treatment of allergic tattoo reactions to red dye[5]; hence, laser treatment of allergic tattoo reactions is now considered as relatively contraindicated by many authors.[6] Sepehri et al.[7] therefore suggested removal of the tattoo or tattoo reaction using a dermatome and were able to successfully treat 50 patients. Since then, this treatment method has been regarded as the treatment of choice for non-responders to conservative therapy in case of colored tattoo reactions.
In the following retrospective study, we report our experience of operative treatment of allergic tattoo reactions to red dye in seven patients.
SUBJECTS AND METHODS
Detailed information of the seven patients is provided in Table 1 in the Appendix.

- Patient 1 before therapy

- Patient 1 at approximately 6 years after therapy

- Patient 2 before therapy
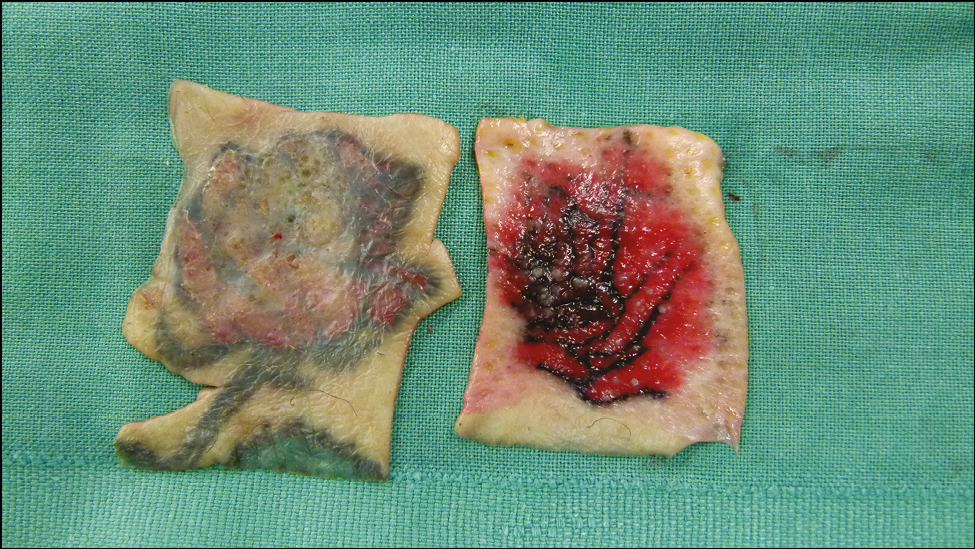
- Patient 2 intraoperative

- Patient 2 at approximately 6 years after therapy

- Patient 3 before therapy

- Patient 3 at approximately 5 months after therapy

- Patient 4 before therapy

- Patient 4 at approximately 6 weeks after therapy

- Patient 5 before therapy (the tattooed number in the upper part of the image was deleted to protect the identity of the patient)

- Patient 5 at approximately 5 months after therapy

- Patient 6 before therapy

- Patient 6 at approximately 5 months after therapy

- Patient 7 before therapy

- Patient 7 at approximately 8 months after therapy
Patients
In the period from 2013 to 2018, a total of seven patients (6 females and 1 male) with allergic tattoo reactions to red dye were treated in our clinic. The youngest patient was 21 years old at the first presentation and the oldest was 66 years old. The tattoo colors used came from the USA, Hungary, and Germany.
Medical history and clinical picture
The patients’ medical histories and findings were reviewed, and photo documentation was carried out. Classification of objective findings by clinical examination was done according to the already mentioned diagnostic algorithm by Serup et al.[8]
Pre-therapies
All patients underwent pre-therapy consisting of highly potent topical steroids and triamcinolone injections. One patient (P1) also received systemic steroid therapy which had to be discontinued because of the ineffectiveness and significant side effects (weight gain, steroid-induced acne). Patient 5 (P5) unsuccessfully underwent a trial laser treatment with CO2 laser in fractional mode.
Histology
A biopsy was taken from all patients prior to starting treatment.
Epicutaneous test
In six of the seven patients, allergological tests of the tattoo colors used were carried out before the treatment, and in some cases, other components of the DKG series (Deutsche Kontaktallergie Gruppe, German Contact Allergy Research Group) were also tested. In one patient, the used color could not be determined, because the tattoo was made abroad.
OP technique
In three of the seven patients, a classic surgical removal of the tattoos was carried out by means of complete excision of the fatty tissue and subsequent defect closure by means of transposition flap (P1), multiple advancement flaps (P3), full-thickness skin grafts (P1), or secondary healing (P4). In patient 2, the tattoo was completely removed by means of an electrodermatome; the healing occurred by secondary intention. For the patients treated in 2018 (P5, P6, and P7), only the mostly sharply demarcated, plaque-like red raised areas were removed with a scalpel or Biopsy Blade® (Kai Europe GmbH, Solingen, Germany). An attempt was made to preserve the shape of the tattoo as well as the surrounding tattoo and parts of the red dye. Healing by secondary intention was observed.
RESULTS
Time interval
The interval from the tattooing to the appearance of the first symptoms was quite different and ranged from 0 (immediate symptoms after the tattoo was applied) to 20 months.
Pre-existing tattoos
Two of the patients had pre-existing tattoos (P3 had red and black tattoos; P4 had a black tattoo). While the black tattoo of P4 did not react, P3 showed a co-reaction between the pre-existing red tattoo parts.
Epicutaneous tests
Two of the patients tested had a positive reaction to the dye used. Three nickel and one cobalt sensitizations were also found. The relevance of the demonstrated sensitization appears to be unclear; sensitization may have been acquired both in the private sphere and via the tattoo needles used.[9]
Clinical pattern
The size of the tattoos varied greatly and ranged from a few centimeters (in P7) to a large tattoo on the forearm (in P5) to multiple tattoos on both forearms and on the back (P3). The majority of the tattoos were found on the lower extremity. All tattoos had multiple colors, and the allergic reaction was limited to the area with the red dye.
The patients in our cohort could be easily assigned to one of the patterns using the classification proposed by Serup et al.[8] According to this definition, most patients showed a plaque-like structure, whereas P4 had an excessively hyperkeratotic clinical picture, which makes an allergic reaction likely.
Histology
Overall, a very heterogeneous histological picture with different inflammation patterns was observed. However, they all had in common a more or less pronounced lymphohistiocytic inflammatory reaction. In two patients, pseudoepitheliomatous epidermal hyperplasia was observed in addition to the inflammatory infiltrates. In three of seven patients, a lichenoid and additionally granulomatous picture was observed.
Post-operative outcome
Post-operative healing was fastest in patients with transposition or advancement flap plasty (P1 and P3). Patient 2, whose tattoo was removed by means of a dermatome, presented to us again 3.5 years after the procedure for a chronic inflammatory lesion within the shaved area. A definite relation to the tattoo could not be proven; however, the dye in small amounts and in the histological staining was mostly not visible.
In P3, the star-shaped tattoos on the forearms were removed step-by-step by serial excisions at intervals of 4–6 weeks. Interestingly, the remaining inflammatory changes decreased by themselves after the third series excision. Furthermore, the older tattoos that reacted together with the newly made tattoos were without symptoms; hence, further series excisions could be avoided.
The tattoo on the lower leg of P4 was removed by complete excision, because based on the histological image of a pseudoepitheliomatous epidermal hyperplasia, a well-differentiated squamous cell carcinoma could not be excluded. The patient wished for secondary healing of the defect extending into the subcutis. A healing process over several weeks can be assumed. Unfortunately, the patient did not present herself for further check-ups.
In P5, P6, and P7 only the raised parts of the tattoo were removed with a scalpel or biopsy blade while leaving some of the red dye intact. Healing was usually achieved within 14 days.
Aesthetic results
In P1, the transposition flap and full-thickness skin transplant had healed well, leaving visible scars and a color deviation in the area of the transplants. In P2, the result was a square depigmented area. Patient 3 had multiple line and star-shaped scars on both forearms at the end of the treatment with serial excisions. Unfortunately, P4 did not attend subsequent follow-ups and hence could not be assessed further. The best cosmetic result was achieved in P5, P6, and P7, where the tattoo could be preserved at least in parts. Patient 7 presented again about 6 months after the tattoo removal because of a remaining nodule in the border area of the tattoo. This was removed with a scalpel blade, and the tattoo healed completely.
DISCUSSION
The spectrum of the colors used for creating red tattoos has changed in the last few decades. Earlier, inorganic salts were used as dyes; however, azo dyes are almost exclusively used now, which are also used in the automobile industry. The azo dyes Pigment Red (P.R.) 22, 170, and 210 have specifically been identified as being responsible for chronic allergic tattoo reactions.[10] However, the confirmation of an allergy is often frustrating, as the allergen is in most cases only formed in the skin after the tattooing process. It is suspected that the triggering allergen could be a photodegradation product of the color pigments that have formed in the skin over time by UV or laser irradiation.[11] Accordingly, the epicutaneous tests with the dyes used are usually negative.[11] Contrary to this theory, a positive reaction could be detected in 2/5 of the patients tested for the dyes used in our group of patients, which means that the allergen must have already been present in the dye mixture in these cases. Despite the fact that the triggering allergen or hapten was already contained in the tattoo color, the allergic reaction did not develop faster in these patients than in those that tested negative.
In case of negative allergological tests, the medical history, clinical findings, and histology are important for the correct diagnosis of an allergic reaction. All of our cases could be assigned to an allergic reaction to red tattoo dye based on the medical history and clinical pattern described by Serup.[3]
Patients with an allergic reaction to red tattoo dye often show no response to local therapy,[12] so removal of the allergen is the only therapeutic option. Normally, tattoos without inflammatory changes can be removed by pico- or nanosecond Q-switched Nd:YAG, ruby, or even alexandrite lasers. According to reports on partly systemic reactions in the course of laser treatment for allergic tattoo reactions to red dye,[13] many authors consider it to be relatively contraindicated.[6] Moreover, the possibility of fractional tattoo ablation by means of CO2 laser,[13] which was initially described as a new paradigm, is now associated with a generalized allergic reaction.[5]
Therefore, surgical excision is the gold standard in the treatment of allergic tattoo reactions. During shave excision, as described by Sepehri et al.,[7] the allergen is completely removed by removing the corium in slices, thereby removing the trigger of the allergic reaction. However, this procedure leaves an area of hypo- or hyperpigmented skin. Depending on the depth of the pigment and the thickness of the corium, a sunken or hypertrophic scar may also result, along with varying healing times. Therefore, patients are left with a scar instead of the tattoo originally intended as body decoration and associated with considerable costs.
The clinical course of P5, P6, and P7 suggests that complete removal of the pigment may not be necessary. Patient 5 is particularly interesting in this context. In her case, the inflammatory reaction decreased after removal of parts of the tattoos, both in the newly created tattoos and in the older tattoos that also triggered an allergic reaction.
In the three patients treated with superficial shaving, the tattoos could also be partially preserved, even if the color was no longer as intense. Interestingly, Mlakar[141516171814] also reported a single case of superficial tattoo removal by shaving, which confirms our observation.
We therefore postulate that a reduction of the allergen by superficially removing the raised plaque may be sufficient for healing of the allergic reaction. The mechanism remains unclear; it is possible that the amount of the allergen is important, but it is also conceivable that the removal of the epidermis and superficial corial parts of the corium may improve dye drainage.
The main limitation of the study is the small number of cases to generalize our results. More number of patients should be treated this way to validate our results.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- [Tattoos in Germany: Prevalence, demographics, and health orientation] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2019;62:1077-82.
- [Google Scholar]
- How to diagnose and classify tattoo complications in the clinic: A system of distinctive patterns. Curr Probl Dermatol. 2017;52:58-73.
- [Google Scholar]
- Treatment of reaction to red tattoo ink with intralesional triamcinolone. An Bras Dermatol. 2017;92:748-50.
- [Google Scholar]
- Generalized eczematous reaction after fractional carbon dioxide laser therapy for tattoo allergy. J Cosmet Laser Ther. 2016;18:456-8.
- [Google Scholar]
- Guide to treatment of tattoo complications and tattoo removal. Curr Probl Dermatol. 2017;52:132-8.
- [Google Scholar]
- Introduction of dermatome shaving as first line treatment of chronic tattoo reactions. J Dermatolog Treat. 2015;26:451-5.
- [Google Scholar]
- Classification of tattoo complications in a hospital material of 493 adverse events. Dermatology. 2016;232:668-78.
- [Google Scholar]
- Distribution of nickel and chromium containing particles from tattoo needle wear in humans and its possible impact on allergic reactions. Part Fibre Toxicol. 2019;16:33.
- [Google Scholar]
- Identification of pigments related to allergic tattoo reactions in 104 human skin biopsies. Contact Dermatitis. 2020;82:73-82.
- [Google Scholar]
- Patch test study of 90 patients with tattoo reactions: Negative outcome of allergy patch test to baseline batteries and culprit inks suggests allergen(s) are generated in the skin through haptenization. Contact Dermatitis. 2014;71:255-63.
- [Google Scholar]
- Treatment of tattoo allergy with ablative fractional resurfacing: A novel paradigm for tattoo removal. J Am Acad Dermatol. 2011;64:1111-4.
- [Google Scholar]
- Successful removal of hyperkeratotic-lichenoid reaction to red ink tattoo with preservation of the whole tattoo using a skin grafting knife. Acta Dermatovenerol Alp Pannonica Adriat. 2015;24:81-2.
- [Google Scholar]
- Azo pigments and quinacridones induce delayed hypersensitivity in red tattoos. Contact Dermatitis. 2015;72:97-105.
- [Google Scholar]
- Tattoo complaints and complications: Diagnosis and clinical spectrum. Curr Probl Dermatol. 2015;48:48-60.
- [Google Scholar]
- Histopathology and immune histochemistry of red tattoo reactions. Interface dermatitis is the lead pathology, with increase in T-lymphocytes and Langerhans cells suggesting an allergic pathomechanism. Skin Res Technol. 2015;21:449-58.
- [Google Scholar]
- Pseudoepitheliomatous epidermal hyperplasia in tattoos: Report of three cases. Am J Clin Dermatol. 2008;9:337-40.
- [Google Scholar]
APPENDIX
| Patient | Year of birth/sex | Date, place, and motive of the tattoo | Colours used | Pre-existing tattoos | First signs | Epicutaneous tests | Histology | Pre-therapy | First presentation at the clinic/ Skin findings | Treatment | Results |
|---|---|---|---|---|---|---|---|---|---|---|---|
| P1 | 1992, female | 08/2012 Right foot back, 3 hearts (fig. 1) | Red and black (Dark Red and Light Red, Code: 3002, 3003), Magic Moon Tattoo Inc. GmbH/Erkelenz | Not known | Immediately after tattooing: Inflammation limited to the red colour part with redness and weeping | Patch test DKG (German contact allergy research group) Standard series: neg. 3+ reaction to the red dye used (Dark Red and Light Red) | Superficial and deep perivascular, periadnexal, and interface dermatitis of the lichenoid type in combination with superficial to deep granulomatous dermatitis | Initially local steroids (betamethasone dipropionate, mometasone) and systemic steroids over several months (side effects: weight gain, acne, flush) | 03/2013: Three to 4.5 × 4.0 cm large, erythematous infiltration, partly weeping plaques on the back of the right foot | 09/2013 excision of one of 3 tattoos, wound closure with transposition flap plasty 02/2014 excision of the two remaining tattoos, wound closure with full skin graft (groin) | Scars with hyperpigmentation (fig. 2) |
| P2 | 1960, female | 05/2012, left lower leg, Rose (fig. 3) | Red, green, black (manufacturer not identifiable) | No | 01/2014 | Not tested | Partly lichenoid, partly epitheloid cellular granulomatous dermatitis | Local steroids (mometasone) for several months | 02/2014, infiltrated plaque in the red area, partially with hyperkeratoses (approx. 3.0 × 3.5 cm) | 12/2014, tangential Shaving with the electrodermatome (figs. 4. 5); complete removal of the pigment down to the deep dermis | Superficial scarring with hypopigmentation (fig. 6) |
| P3 | 1993, female | 03/2015, left forearm, Motif: Stars (fig. 7) | Tattoo ink bright red, Firma: Professional Tattoo Colours | 6 years before, tattoos with red parts on right arm and back | About 4 weeks after stitching the tattoo's, occurrence of itchy skin changes in the red parts of the newly created tattoo. The red colour parts in the tattoos created about 6 years ago also showed inflammatory changes. | DKG-standard-series: Nickel-II sulphate ++ positive red tattoo dye: +positive | Pronounced dermal lymphocyticand partly granulomatous inflammatory reaction | Local steroids (betamethasone dipropionate) and intralesional steroids (triamcinolone with dermojetR) over several months | 04/2015: On the left forearm within the red parts of a tattoo measuring approximately 30 × 8 cm, distinctly infiltrated plaque, partly weeping with blistering was noted On the right forearm and back, infiltrated plaque, also in the area of the red pigmented parts of the existing tattoos was seen. | 01-09/2016: multiple excisions of the inflammatory foci on the left upper and lower arm, in the course of the partial excisions complete regression of the inflammatory reaction in the area of the remaining new and old tattoos despite remaining parts of the red dye in the skin | Noticeable multiple star and line scarring, cosmetically rather unsatisfactory (fig. 8). |
| P4 | 1968, female | 02/2015, lower leg left, flower motif (fig. 9) | Red, Black, manufacturer unknown (Tattoo Fair in Hungary) | Black tattoos an right lower leg and on both upper arms (without Inflammation) | 08/2015 Onset of inflammation, limited to red dye | Known type IV sensitization to cobalt and nickel (already known before tattooing, testing in 1996 and 2013) Used paint not to be provided | Pseudoepitheliomatous epidermal hyperplasia with marked mixed cellular, partly nodular, partly lichenoid lymphocytic inflammatory response | Local steroids for several months (drug not known) | 08/2016: On the left lower leg in the area of the originally red pigmented lily leaves, erythematous nodi with central erosion on an area of about 8 × 8 cm was seen. | 10/2016, complete excision down to the subcutaneous fatty tissue, also to exclude a squamous cell carcinoma, secondary healing was facilitated at the wish of the patient (fig. 10) | Not assessable, as not presented again |
| P5 | 1963, male | 02/2017, left forearm: football team emblem (fig. 11) | Red and black dye (Boris Tattoo from Hungary), bright red | no | Approximately 3 months after tattooing: inflammation/itching/wetting limited to red dye | Various dyes, including those from hairdressing products: negative Tattoo colours used: negative | Dense dermal lymphocytic inflammatory reaction with involvement of histiocytes and plasma cells | Local steroids (Clobetasol) over 8 weeks, fractional CO2 laser as a one-time treatment (without effect) | 07/2017: Large erythematous plaque on the left forearm | 01/2018, Shave excision with the scalpel | After superficial removal of the tattoo complete reduction of the inflammation despite partially remaining red dye, good cosmetic result (fig. 12) |
| P6 | 1952, female | March 11, 2017, lower leg left, Motive: 3 flowers (fig. 13) | Red, black, green, yellow Dark Red, Eternal Ink Inc., Brighton, USA | no | 05/2017 Increasing thickening of the red parts of the tattoo with itching | Tattoo colours negative | Pseudoepitheliomatous epidermal hyperplasia with pronounced partially lichenoid dermal lymphoplasmocellular inflammatory reaction | Local steroids (betamethasone dipropionate, FucicortR) for several weeks | 09/2017: Significant infiltration and scaling in the red tattooed areas. Green and black tattoo areas were inconspicuous. | 01 and 03/2018 Superficial shave excision of the red parts with a scalpel | Complete resolution of inflammation despite partially remaining red dye, good cosmetic result (fig. 14) |
| P7 | 1983, female | 04/2017 right foot (stick figure); (fig. 15) | Magenta, black. Eternal Ink, Brighton, USA | No | Itching after 14 days, which aggravated after 3 months | tattoo dye: negative | Partly diffuse, partly nodular dense lymphohistiocyte inflammatory cell infiltrates with detection of pink pigment within histiocyte cells | Local steroids (preparation and duration not available) | 08/2018 foot right: sharply bordered hypertrophic itchy reaction in the area of the magenta-coloured tattoo site | 09/2018 Superficial shave excision with Biopsy-Blade 05/2019 again shave excision of the remaining inflammatory area | After the last session, complete decrease of inflammation was seen, despite retained red dye, with good cosmetic result (fig. 16). |





