Translate this page into:
Retiform Hemangioendothelioma: A Rare Tumor in the Medial Canthus: Case Report and Review of Literature
Address for correspondence: Dr. Meenakshi Rao, Department of Pathology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India. E-mail: drmeenakshirao@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Retiform hemangioendothelioma (RH) is a rare vascular neoplasm with intermediate malignant potential mostly occurring in extremities. It is important to differentiate this neoplasm from malignant conditions as RH has a good prognosis. As it has a tendency to recur locally, it may be misdiagnosed as a malignant tumor. Herein, we report a rare case of RH occurring in the medial canthus.
Keywords
Retiform hemangioendothelioma
medial canthus
CD31
INTRODUCTION
Retiform hemangioendothelioma (RH) is a rare tumor with only about 59 reported cases till date. The first case of RH was described in 1994 by Calonje et al.[1] as a vascular neoplasm with intermediate malignant potential and referred it to as low-grade angiosarcoma.
The most common site associated with RH is the distal extremities especially lower limbs.[2] It is rarely seen in unusual sites like penis, scalp, pleural nodule, and mons pubis. RH occurring in the medial canthus has been reported only in two cases earlier.
Herein, we report a case of RH occurring in the medial canthus, which is a rare site.
CASE PRESENTATION
A 36-year-old woman presented with a swelling involving the right medial canthus and the bridge of the nose for 1 year. Initially, the lesion was nodular, which progressively ulcerated and was associated with surrounding swelling for which the patient visited the outpatient department. The lesion measured 3 × 2 cm and appeared ulcerated with violaceous, erythematous inflamed margins and undermined edges with necrotic debris. The base of the lesion was erythematous and necrotic admixed with granulation tissue. The surrounding skin showed cellulitis with an expansion of the ulcer into the right orbit [Figure 1]. On the basis of appearance of the lesion, a clinical diagnosis of malignancy, most likely basal cell carcinoma, was made. The patient did not have any other significant medical history.

- Gross clinical appearance of the lesion in the medial canthus of the right eye showing a nodular, ulcerated growth
An incisional biopsy taken from the ulcer showed an infiltrative lesion in the mid and lower dermis, composed of numerous variably dilated to compressed, arborizing vascular channels [Figures 2 and 3]. The vessels were lined with endothelial cells exhibiting hobnailing, and the lesion resembled rete testis [Figure 4]. Occasional vessels showed pseudopapillary tufts within the lumen. Focally, solid nests of round-to-oval cells with pale eosinophilic cytoplasm were seen. Surrounding stroma showed neutrophils and lymphocytes. There was no significant atypia or mitotic figures. Papillary dermis was uninvolved. On immunohistochemistry, lesional cells were positive for CD31 [Figure 5]. On the basis of histopathological examination, a diagnosis of RH was made. The patient was advised radiology to determine the extent of lesion and was explained the possible role of surgery as the treatment. However, the patient refused any possible surgery on the face for cosmetic reasons and did not come for follow-up.
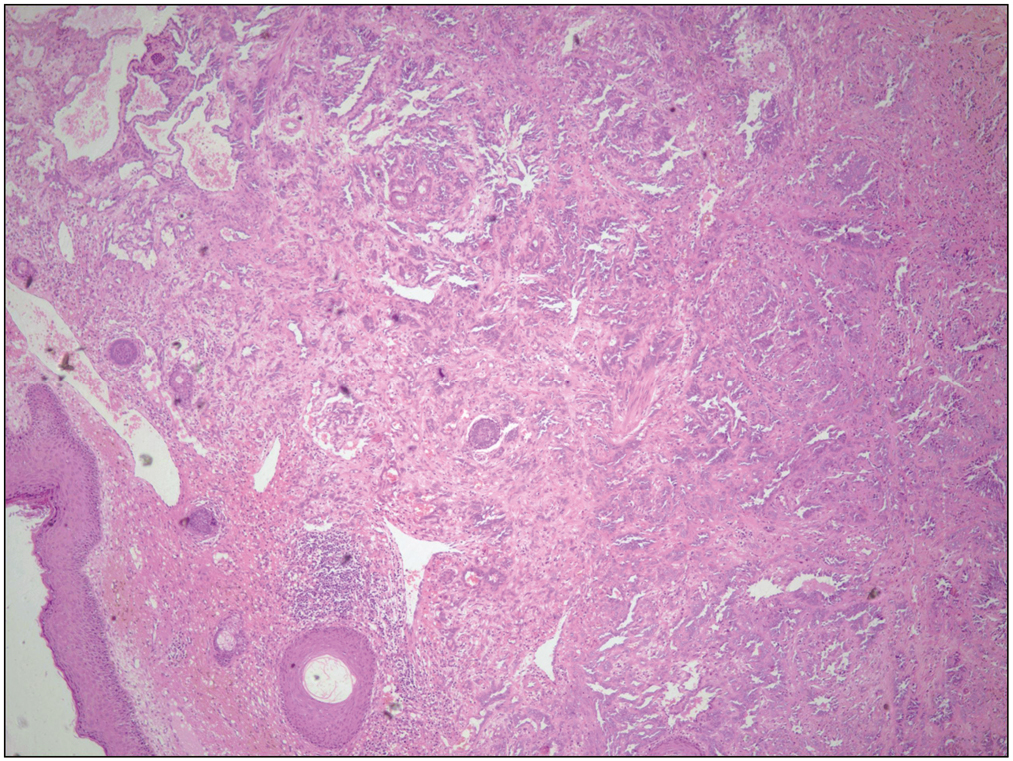
- Biopsy showing an infiltrative lesion in the mid and lower dermis, resembling rete testis at scanner view (H&E, ×4)
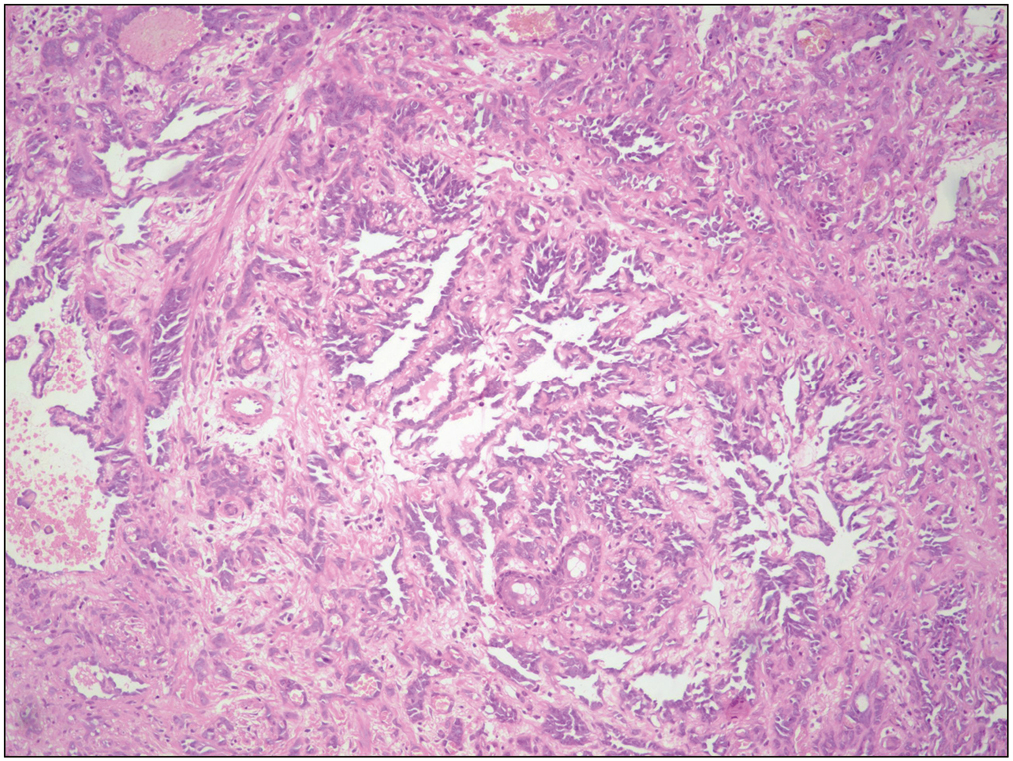
- Low power view shows a vascular lesion composed of numerous, variably sized, arborizing vascular channels (H&E, ×10)
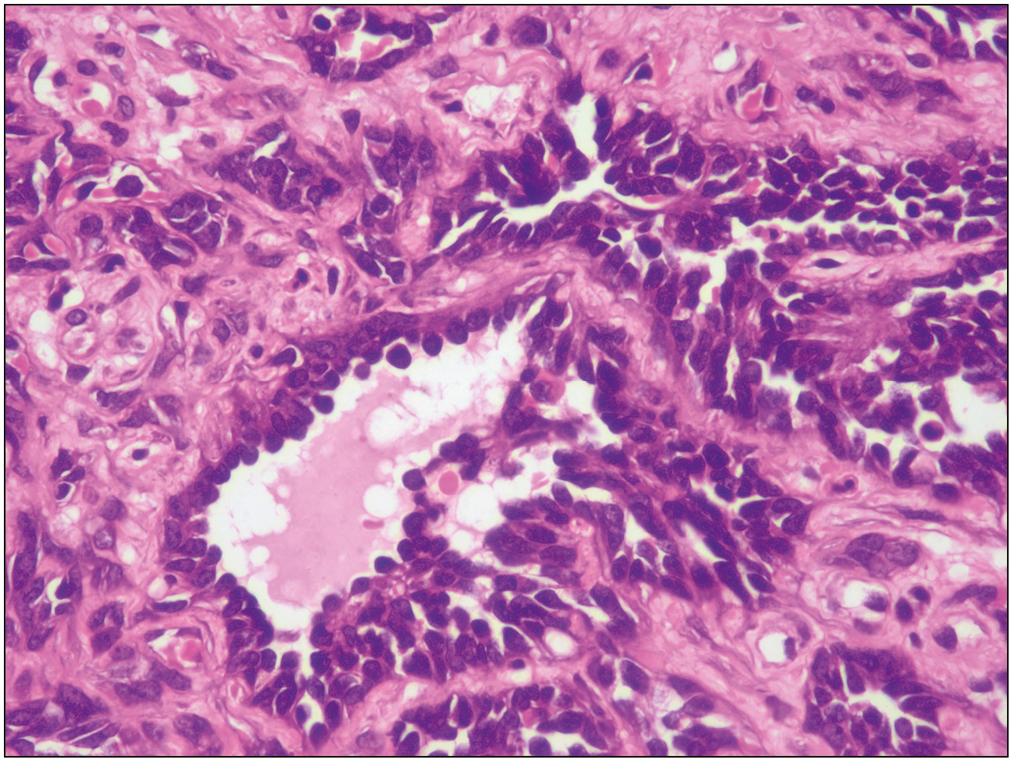
- High power view shows the vascular channels lined with endothelial cells exhibiting hobnailing and absent to minimal cytological atypia. No mitoses were noted (H&E, ×40)
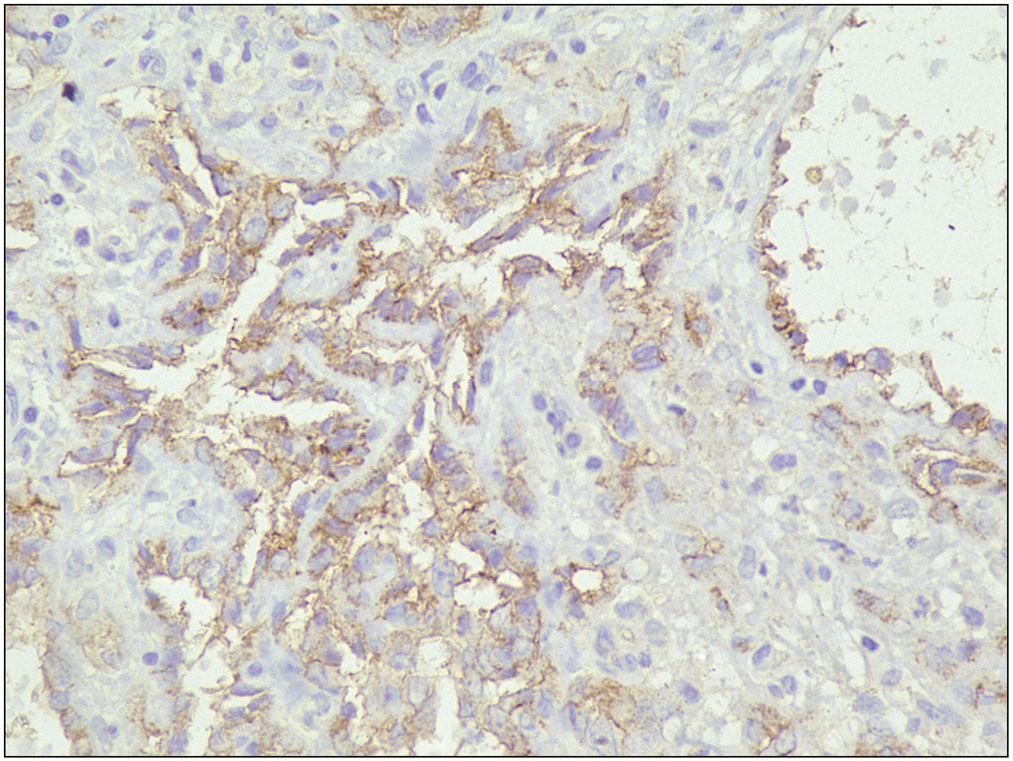
- The lesional cells lining the channels show immunoreactivity for CD31 (IHC, ×40)
DISCUSSION
RH is a rare vascular neoplasm, first described by Calonje et al. in the year 1994 in a case series of 15 patients. World Health Organization (WHO) classification 2001 included RH as a rare entity with an intermediate malignant potential.[3] Since the first diagnosis of RH in the year 1994, very few cases have been reported in the literature [Table 1]. The etiological factors leading to the formation of RH have not been clearly established, but it has been associated with lymphedema, prior radiation exposure, nonepidermal malignant tumor, human herpesvirus-8, etc.[3]
| S. no. | Study | Age | Site | Recurrence | Metastasis |
|---|---|---|---|---|---|
| 1 | Calonje et al. (1994)[1] | 9–78/9F, 6M | Lower limbs (six), upper limbs (four), trunk (three), penis (one), scalp (one)/2.0–9.0 cm | 8/15 | 1/15 |
| 2 | Fukunaga et al. (1996) | 75/F | Lower thigh/3.5 cm | Y | N |
| 3 | Duke et al. (1996) | 30/F | Trunk, breast, and extremities | N | N |
| 4 | Dufau et al. (1997) | 29–40/2F | Lower limb/1.0–1.5 cm | N | N |
| 5 | Sanz-Trelles et al. (1997) | 11/M | Toe/1.5 cm | N | N |
| 6 | Mentzel et al. (1997) | 40/F | Right great toe and right lower leg/ND | Y | N |
| 7 | Schommer et al. (2000) | 73/F | Trunk/30 cm | Y | N |
| 8 | El Darouti et al. (2000) | 32/F | Left upper thigh/3.5 cm | N | N |
| 9 | Ulrich and Hrynyschyn (2002) | 17/M | Upper limb/0.5 cm | Y | N |
| 10 | Escudero et al. (2003) | 31, 82/F | Sole, dorsum of hand | ND | ND |
| 11 | Aditya GS (2003) | 36/M | Skull bone/5.0 cm | ND | ND |
| 12 | Tan et al. (2005) | 19/F | Lower limb/4.5 cm | N | N |
| 13 | Botros et al. (2005) | 30/F | Scalp | Y | N |
| 14 | Ioannidou et al. (2006) | 55/F | Left middle finger/1.2 cm | N | N |
| 15 | Serel et al. (2007) | 27/M | Left foot | N | N |
| 16 | Parson et al. (2008)[8] | 17–71/F | Back, upper extremity, medial canthus, foot | ND | ND |
| 17 | Bhutoria et al. (2009) | 35/F | Mons pubis/4.0 cm | Y | Y |
| 18 | Emberger et al. (2009)[9] | 17/M | Back/2.5 cm | N | N |
| 19 | Kajo et al. (2009) | 8/F | Calf | ND | ND |
| 20 | Zhang et al. (2010)[10] | 61/F | Scalp and ear/8.0 and 2.0 cm | Y | N |
| 21 | Aydingöz et al. (2010) | 60/F | Left ankle/6.0 cm | N | N |
| 22 | Hirsh et al. (2010) | 44/M | Scrotum/NA | N | N |
| 23 | Keiler SA (2011) | 11/F | Left fourth finger/0.7 cm | N | N |
| 24 | Albertini et al. (2011) | 6/F | Neck/NA | N | N |
| 25 | O'Duffy et al. (2012) | 18/M | Left pinna rim/NA | Y | Y |
| 26 | Choi et al. (2012) | 20/M | Left index finger/1.5 cm | Y | N |
| 27 | Couceiro J (2013) | 42/F | Small finger/1.0 cm | N | N |
| 28 | Mota A (2013) | 26/F | Right flank/3.0 cm | N | N |
| 29 | Al-Faky et al. (2014)[7] | 9/F | Right medial canthus/0.8 cm | N | N |
| 30 | Ezhil Jothi (2014) | 58/M | Right ear/4 cm | N | N |
| 31 | Zheng LQ (2014) | 71/F | Right foot/12.0 cm | Y | N |
| 32 | Ranga SM (2014) | 9/M | Chest | Y | N |
| 33 | Tamhankar et al. (2015)[6] | 48/F | Forehead | N | N |
| 34 | Liu et al. (2015)[5] | 30/F | Pleural nodule | N | N |
| 35 | Kim et al. (2016)[2] | 13/M | Buccal region | N | N |
| 36 | Seema Rani (2016) | 23/F | Scalp/1–2 cm | N | N |
| 37 | Yang Tan (2017) | 42/F | Left leg/1–3 cm | N | N |
| 38 | Pan et al. (2017)[3] | 56/F | Left forearm and right neck/4.0 cm and 2.0 cm | Y | N |
| 39 | Shagufta Quadri (2018) | 76/F | Right gluteal region/9 cm | N | N |
| 40 | Mondal et al. (2020)[4] | 35/M | Postauricular/3 cm | N | N |
| 41 | Present case | 36/F | Medial canthus |
F = female, M = male, N = no, NA = not available, ND = not documented, Y = yes
RH involves a wide age group but predominantly occurs in adults during the second to fourth decade of life[4] and shows a female predilection.[3] The most common location of this tumor is skin and subcutaneous tissue of the extremities, mostly the lower limb. Other rare sites reported included penis, scalp, pleural nodule, and mons pubis.[56] Two cases reported by Al-Faky et al.[7] and Parson et al.[8] demonstrated RH occurring in the medial canthus, similar to our case.
Clinically, RH usually presents as a painless reddish or bluish slow-growing, indurated nodule or papule. Though many lesions are solitary and painless, multiple, painful lesions are also known to occur.[7]
On histological examination, RH is characterized by elongated, arborizing vascular channels lined with uniform endothelial cells having a “hobnail” appearance. These vascular channels appear similar to normal rete testis. Stromal lymphocytic infiltration is often present.[46] Histopathological and immunohistochemical examination is important to make a definitive diagnosis, as the clinical features are nonspecific. The extensive sampling of this lesion is also important as RH can be a part of composite hemangioendothelioma consisting of varied components such as RH, epithelioid hemangioendothelioma, low-grade angiosarcoma, lymphangioma, and hemangioma.[5]
RH expresses immunoreactivity for endothelial markers such as CD31, CD34, factor-VIII, and Ulex europaeus agglutinin-1.[6] Few reported cases in the literature have shown RH to be immunoreactive for D2-40, which is a marker for endothelium of lymphatic vessels.[89]
Cutaneous angiosarcoma remains the main differential diagnosis of RH.[6] Angiosarcoma is an aggressive neoplasm having poor prognosis and high recurrence. Clinically, RH can have a variegated appearance, which may mimic angiosarcoma. On histology, angiosarcoma demonstrates marked atypia, mitotic activity, and particularly the absence of hobnail morphology.[10] Although an infiltrative pattern is common to both angiosarcoma and RH, vascular channels of angiosarcoma are more irregular than those of RH. Other differentials for RH include the vascular neoplasms: Dabska tumor and hobnail hemangioma. The Dabska tumor is papillary intralymphatic angioendothelioma and shares some histological features with RH including the presence of lymphocytes in vessel lumina. It is characterized by the presence of “hobnail” cells, irregular papillary endothelial projections and lacks arborizing rete testis-like architecture. The Dabska tumor mainly occurs in children with a tendency to occur in head and neck.[10] Targetoid hemosiderotic hemangioma (hobnail hemangioma) appears brown to violaceous papule with surrounding pale area and an ecchymotic rim, because of the deposition of hemosiderin. These lesions are histologically characterized by the presence of hobnail cells, but the lack of arborizing pattern.[3] Angiomatosis can also be considered differential diagnosis. It usually involves a large part and histologically shows large venous, cavernous, and capillary-sized vessels.[6]
Local recurrence is known to occur in RH, but distant metastasis is infrequent.[4] Wide local excision with free margins of 2–3 cm remains the treatment of choice for RH whenever feasible. Radiation therapy has also been reported to be successful for local as well as regional nodal cases.[1] One case has also been reported to be effectively treated with low-dose Cisplatin and moderate radiotherapy. It is difficult to establish a treatment guideline as of now because of scarce number of reported cases. Other treatment modalities of this tumor are still being investigated.
To conclude, RH is a rare vascular tumor with the medial canthus being even a rarer site. It can present in uncommon locations and can clinically mimic malignancy. Histopathological examination proves to be an important diagnostic tool in this regard.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Retiform hemangioendothelioma. A distinctive form of low-grade angiosarcoma delineated in a series of 15 cases. Am J Surg Pathol. 1994;18:115-25.
- [Google Scholar]
- Retiform hemangioendothelioma in the infratemporal fossa and buccal area: A case report and literature review. J Korean Assoc Oral Maxillofac Surg. 2016;42:307-14.
- [Google Scholar]
- Unusual multiple cutaneous retiform hemangioendothelioma on forearm and neck misdiagnosed as angiosarcoma with metastasis. Clin Diagnostic Pathol. 2017;1:1-5.
- [Google Scholar]
- Retiform hemangioendothelioma: An uncommon vascular neoplasm. Indian J Pathol Microbiol. 2020;63:122-4.
- [Google Scholar]
- A case report of retiform hemangioendothelioma as pleural nodules with literature review. Diagn Pathol. 2015;10:194.
- [Google Scholar]
- Retiform hemangioendothelioma over forehead: A rare tumor treated with chemoradiation and a review of literature. J Cancer Res Ther. 2015;11:657.
- [Google Scholar]
- Retiform hemangioendotheliomas usually do not express D2-40 and VEGFR-3. Am J Dermatopathol. 2008;30:31-3.
- [Google Scholar]
- Retiform hemangioendothelioma: Presentation of a case expressing D2-40. J Cutan Pathol. 2009;36:987-90.
- [Google Scholar]
- A case of retiform-hemangioendothelioma with unusual presentation and aggressive clinical features. Int J Clin Exp Pathol. 2010;3:528-33.
- [Google Scholar]






