Translate this page into:
Rapid Resolution of Subcutaneous Phycomycosis in a Child: A Case Report
Address for correspondence: Dr. Balachandra Suryakant Ankad, Department of Dermatology, S. Nijalingappa Medical College, Near APMC, Navanagar, Bagalkot 587102, Karnataka, India. E-mail: drbsankad@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Subcutaneous phycomycosis is a rare saprophytic fungal infection. We herein report a case of subcutaneous phycomycosis with stony hard swelling on the chest wall as an unusual site of infection. Diagnosis was made based on the clinical, histopathological, and culture studies. Oral treatment with itraconazole resulted in rapid resolution of lesion.
Keywords
Itraconazole
resolution
subcutaneous phycomycosis
treatment
INTRODUCTION
Subcutaneous phycomycosis, also known as subcutaneous zygomycosis, is a rare chronic granulomatous infection of subcutaneous tissue caused by a saprophytic filamentous fungus Basidiobolus ranarum or Conidiobolus coronatus.[1] It has been reported in tropical countries. Here we report a case of subcutaneous phycomycosis in a girl child to give an emphasis on early recognition and administration of itraconazole for faster resolution.
CASE REPORT
A 9-year-old girl came to dermatology clinic with painless swelling over the anterior chest wall since 15 days. Swelling was asymptomatic and non-tender. There was no history of trauma. There was no discharge from the lesion. Cutaneous examination revealed a subcutaneous nodule over the left side of the anterior chest measuring 5 × 7 cm [Figure 1A]. Skin over the nodule was shiny and slightly erythematous with mild crust, and desquamation was observed. Skin was pinchable over the nodule. The nodule was firm to stony hard in consistency. No regional lymphadenopathy was noted. Systemic examination was unremarkable. No abnormality was detected in chest X-ray. Fine needle aspiration cytology revealed round cell tumor.
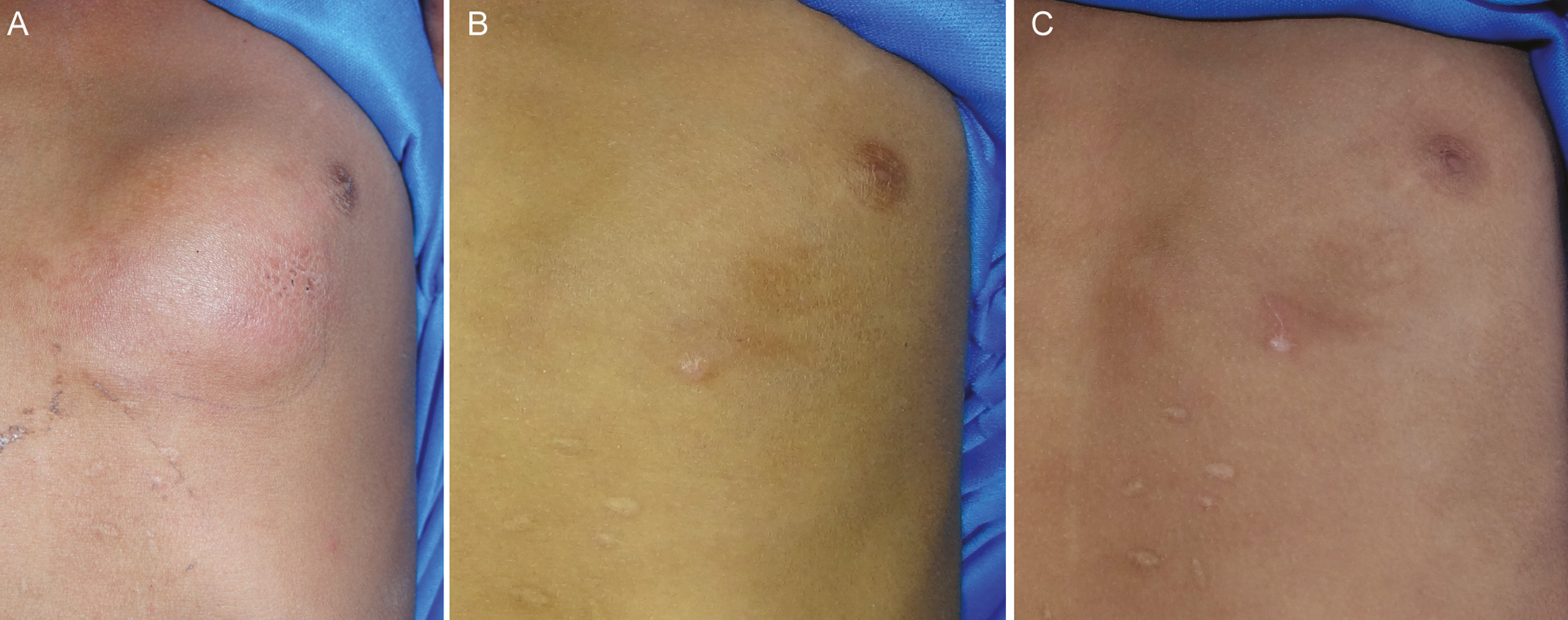
- Clinical image of subcutaneous phycomycosis at first visit showing a subcutaneous nodule present over the left anterior chest region (A), marked improvement on 21st day (B), and complete resolution of lesion after 5 weeks of treatment (C)
Biopsy samples were sent for culture and histopathological study. Culture of skin tissue on Sabouraud dextrose agar at 37°C yielded expanding, waxy growth with cerebriform topography and radial furrows within 5 days. Lactophenol cotton blue tease mount on microscopy showed short broad hyaline pauci-septate hyphae with wide angle branching. Spherical primary conidia with papilla with single nucleus and pyriform secondary conidia were seen. Many thick-walled zygospores were seen and some had lateral protuberances of gametangial remains [Figure 2A]. Organism Basidiobolus ranarum was isolated. Histopathology showed a diffuse granulomatous infiltrate extending from the subcutaneous fat with lobular panniculitis. Infiltrate chiefly consisted of lymphocytes, histiocytes, plasma cells, eosinophils, and a few foreign body giant cells. Among the infiltrate, thin-walled hyphae were seen as ring-shaped, twisted, or as collapsed structures [Figure 2B].
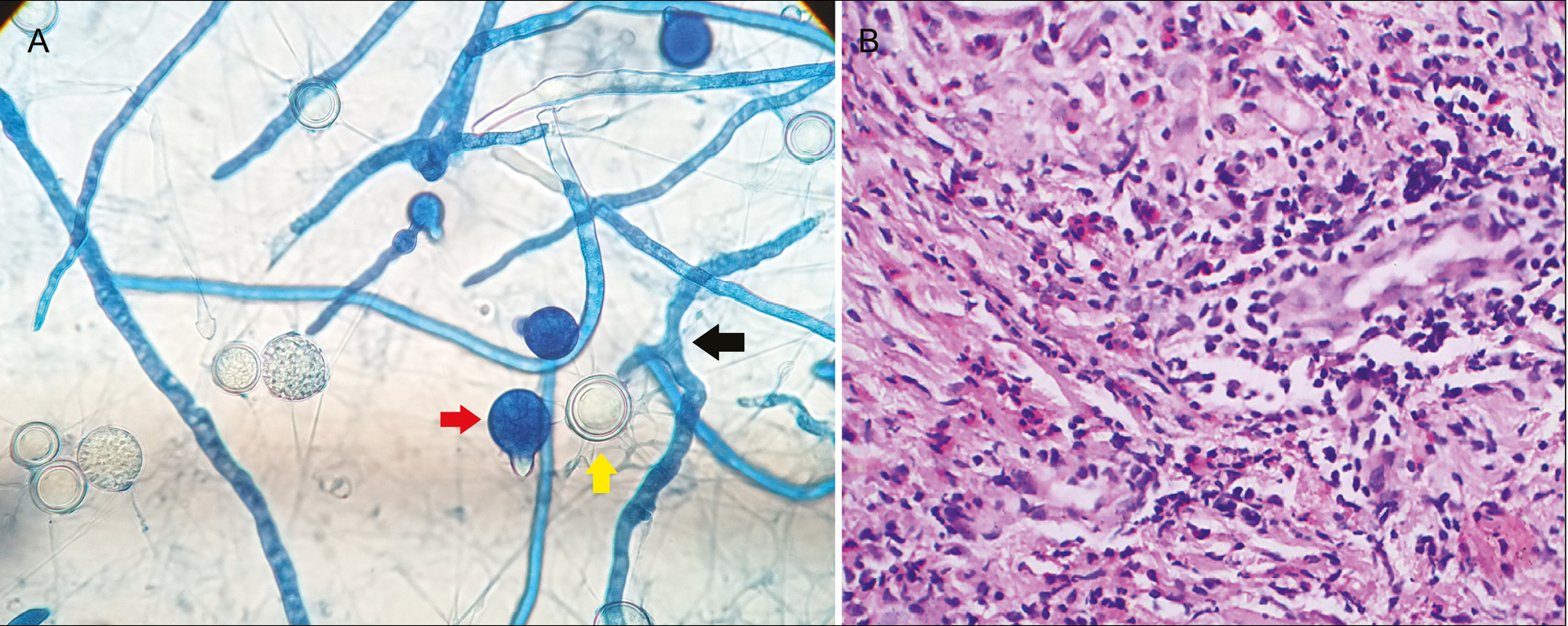
- Microscopy of lactophenol cotton blue wet mount from the culture shows short broad hyaline pauci-septate hyphae with wide angle branching (black arrow). Spherical primary conidia with papilla (red arrow) with single nucleus and many thick-walled zygospores (yellow arrow) seen (A). Histopathology of phycomycosis showed diffuse granulomatous infiltrate consisting of lymphocytes, histiocytes, plasma cells, eosinophils, and a few foreign body giant cells. Among the infiltrate, thin-walled hyphae were seen as ring-shaped, twisted, or collapsed structures (H&E, 100× magnification) (B)
A diagnosis of subcutaneous phycomycosis was made based on clinical features, histopathology, and culture. The child was started on oral itraconazole 100 mg once daily. Marked regression in the size of the lesion was noted by 21st day [Figure 1B] of treatment. Complete resolution was noted by 5th week [Figure 1C]. Itraconazole was continued for 4 more weeks to prevent relapse.
DISCUSSION
Phycomycosis is caused by B. ranarum or C. coronatus belonging to class Zygomycota and order Entomophthoraceae of fungi.[1] The disease is mainly encountered in tropical countries of Africa, Indonesia, and with occasional reports from India.[2]B. ranarum is usually seen in plant debris. It causes subcutaneous zygomycosis and an acute systemic illness. Children are commonly affected.[3] The disease is seen in immuno-competent individuals. In this study, a girl child presented with nodular swelling which developed within a short period of 15 days.
The portal of entry is through minor trauma or after insect bites which goes unnoticed. Lesions are commonly found on limb girdles and buttocks. They present as a firm and woody swelling of subcutaneous tissue.[1] Disparity was observed in our patient; first there was no history of trivial injury and secondly, anterior chest wall was affected which is a rare site for subcutaneous phycomycosis.
Clinical features include painless, unilateral, well-circumscribed solitary swelling. It rarely involves the underlying bones or muscles.[4] In the same line, painless nodule was noted in our case without bone involvement.
Histopathology shows characteristic Splendore–Hoeppli phenomenon with broad aseptate hyphae surrounded by eosinophilic material and with extensive subcutaneous fibrosis.[5] Granulomatous inflammatory reactions are also present.[3] Classical Splendore–Hoeppli phenomenon was not seen in our case. However, other features were suggestive of subcutaneous phycomycosis. The organism is readily cultured in Sabouraud dextrose agar. Microscopy shows large, broad vegetative hyphae and zygospores with beak-like appendages which are characteristics of B. ranarum.[1] Identical features were recognized in our case too.
Subcutaneous phaeohyphomycosis is an important differential diagnosis. It is caused by dematiaceous fungi, Exophiala dermatitidis and Cladosporium cladosporoides. It presents as papulo-nodules, verrucous, hyperkeratotic, or ulcerated plaques or cysts involving the extremities. Histopathologically, brown-walled septate hyphae or yeast-like cells in the dermis and subcutis are noted,[6] thus differentiating from phycomycosis, which is a non-dematiaceous pauci-septate fungi.
As the diagnosis is delayed, the lesion is usually difficult to treat. Most of the patients usually respond well with potassium iodide and azoles.[3] Surgical intervention should be avoided as it hastens the rate of spread of infection and also the associated high relapse rates.[7] Our patient responded well with itraconazole, and a drastic improvement was observed within 5 weeks of treatment. The rapidity of recovery in our case is explained probably on the basis of duration of the lesion which was very short, around 15 days.
To conclude, subcutaneous phycomycosis is an uncommon deep fungal infection affecting children in tropical countries. Early recognition will prevent further disfigurement, and awareness of this entity eliminates the need of surgical intervention in these cases.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- A review of zygomycosis due to Basidiobolus ranarum. Eur J Epidemiol. 1999;15:923-9.
- [Google Scholar]
- Subcutaneous zygomycosis caused by Basidiobolus ranarum—A case report. Indian J Med Microbiol. 2003;21:205-6.
- [Google Scholar]
- An instance of excellent response of subcutaneous zygomycosis to itraconazole monotherapy. Med Mycol Case Rep. 2019;24:13-7.
- [Google Scholar]
- Subcutaneous phycomycosis: A review of 31 cases seen in Uganda. Br Med J. 1964;1:1669-72.
- [Google Scholar]
- Subcutaneous phycomycosis in a child. Indian J Dermatol Venereol Leprol. 2002;68:303-4.
- [Google Scholar]






