Translate this page into:
Dermoscopic Findings of Herpes Zoster in a Toddler: A Case Report
Address for correspondence: Dr. Balachandra Suryakant Ankad, Department of Dermatology, S N Medical College, Bagalkot 587102, Karnataka, India. E-mail: drbsankad@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
Herpes zoster (HZ) commonly occurs in adults and geriatric population. Rarely, it is encountered in pediatric patients with a diagnostic challenge for the treating physician.[1] Dermoscopy facilitates in vivo diagnosis of skin tumors, and recent advances indicate its usefulness in the diagnosis of common skin infections and infestations. Here, we describe dermoscopic features in the case of HZ in a toddler.
A 14-month-old female child was brought by her mother with painful blisters over right buttock since 3 days. History of mild fever since 5 days was noted. Cutaneous examination revealed grouped vesicular lesions on an erythematous base. Few coalesced vesicles showed hemorrhagic crusting. Few aberrant vesicles over lower back were also noted [Figure 1]. There was no history of chickenpox previously in the child and the mother also denied history of varicella infection during the antenatal period. Hematological reports were within normal limit. Varicella zoster, herpes simplex, impetigo, and contact dermatitis were considered differentials.

- Clinical image of herpes zoster showing crops of vesicular lesions on an erythematous base over the upper and lower quadrants of right gluteal area. Note the evolving (box) and mature lesions (arrow)
The dermoscopic examination was done with DermLite Foto II Pro Plus with an attached Nikon D 500 camera in the polarized mode. Evolving lesions showed pale pink polylobular cloudy structures. Each lobule consisted of central brown globules with a grayish zone, which in turn was surrounded by a pale pink area with a grayish rim. Many coalesced lobules demonstrated brown and gray dots in the center [Figure 2]. Few white lines were noted because of superimposition of edges of vesicles. Fully developed lesions demonstrated dark red areas in the center with a darker gray zone that is surrounded by a pale pink rim. Few gray dots were noted in the center [Figure 3].
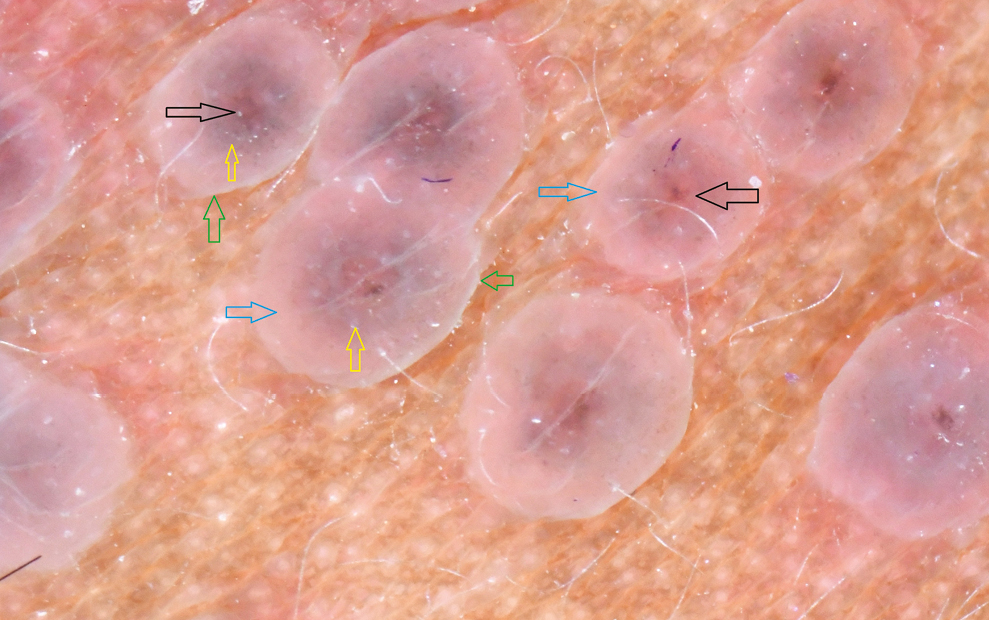
- Dermoscopy of early lesions of herpes zoster shows polylobular structures with central brown globules (black arrows), gray zone (yellow arrows), pale pink area (blue arrows), and grayish rim (green arrows). (DermLite Foto II Pro Plus, 10× magnification, polarized)
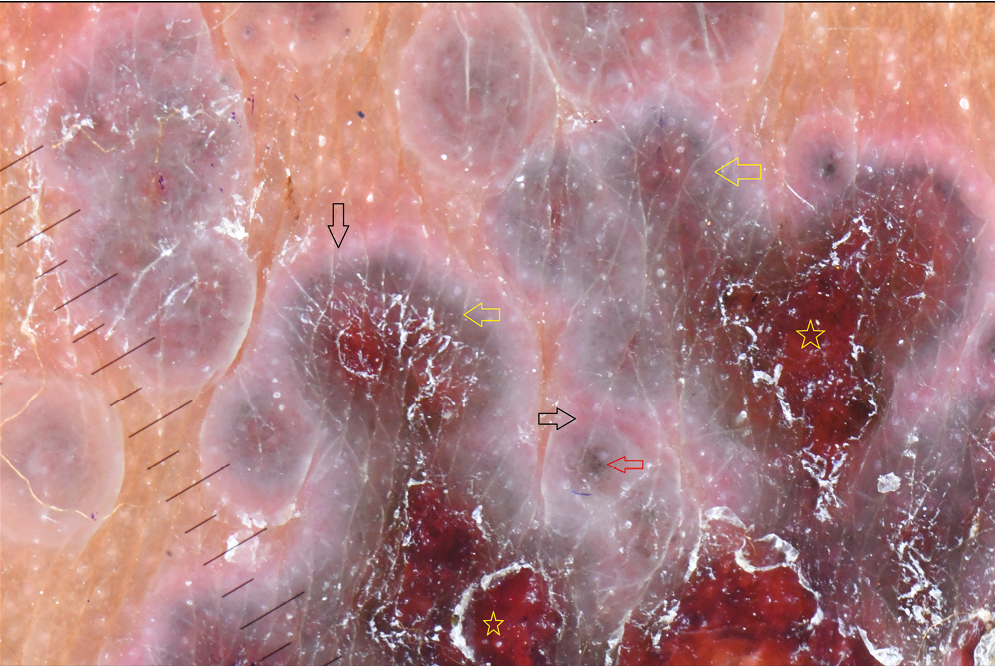
- Dermoscopy of matured lesions of herpes zoster shows dark red areas (yellow stars), darker gray area (yellow arrows), and pale pink area in the periphery (black arrows). Note the gray dots in the center of lobule (red arrow). (DermLite Foto II Pro Plus, 10× magnification, polarized)
Tzanck smear was taken and stained with Giemsa, which revealed characteristic multinucleated giant cells and acantholytic cells [Figure 4]. Skin biopsy could not be done since the mother did not consent for the same. Based on clinical, dermoscopic, and laboratory findings, we arrived at the diagnosis of HZ.
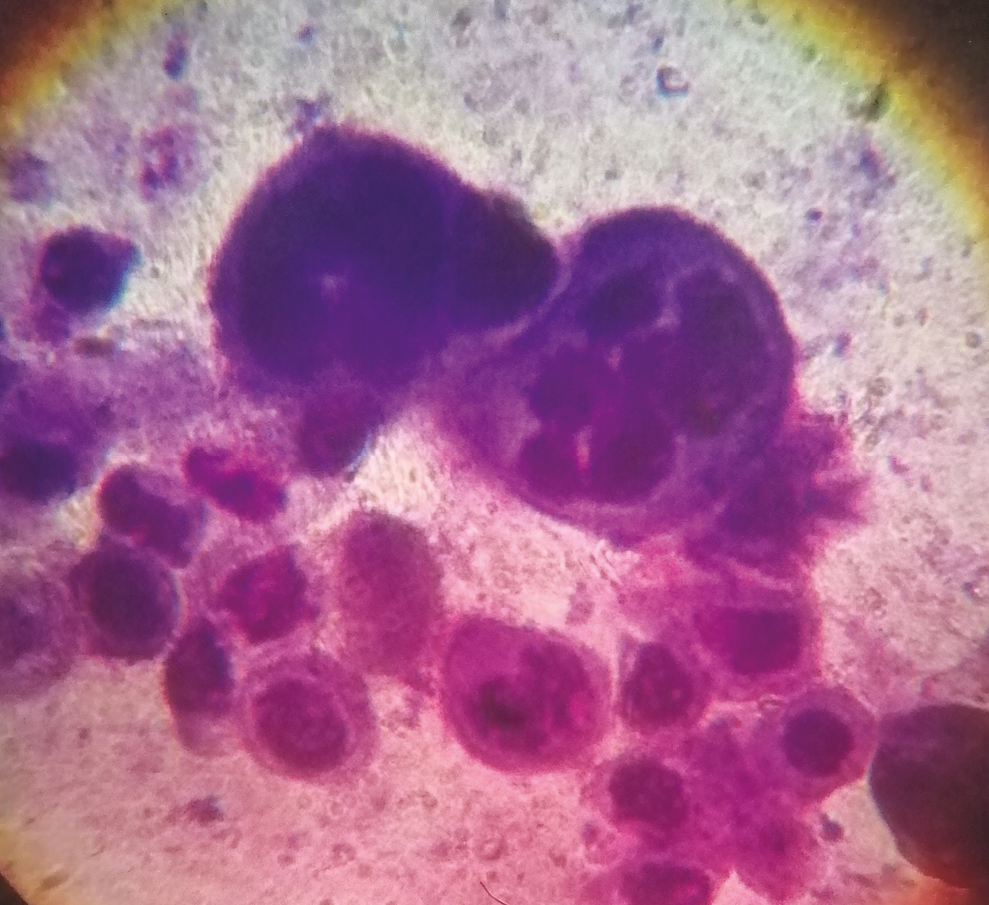
- Tzanck smear from the base of the vesicles showing multinucleated syncytial giant cells and acantholytic cells. (Oil immersion, 100×)
Dermoscopy is a well-established diagnostic method in skin tumors and inflammatory conditions.[2] Pink polylobular cloudy structures and central brown and gray globules are the characteristic dermoscopic features of HZ.[3] Vessels with erythematous base are described in early lesions by handheld reflectance confocal microscopy.[4] Herpes simplex reveals cloudy white globules on a pink background in early stage, whereas yellow globules with few white scales are noted in healing and late stages.[3]
Typical histopathological changes in HZ include intraepidermal blisters with multiple necrotic keratinocytes showing ballooning degeneration and few multinucleated giant cells seen at the base of blister. Small vessel vasculitis in dermis is a characteristic feature.[5] Accordingly, pinkish background corresponds to widespread capillary dilatation. Brown dots and globules result from retained melanin in the epidermis, whereas gray globules are suggestive of necrotic keratinocytes, regenerating epithelium, and dermal melanin. Red area correlates with pronounced hemorrhage due to vasculitis changes. However, vessels were not appreciated under dermoscopic examination. Thus, dermoscopy can aid in the accurate diagnosis of HZ with compounding confirmation by laboratory test.
Although HZ is rare in children, it is noted in the pediatric age group due to primary intrauterine infection by varicella or in immunodeficient or transplant patients. Acquisition of HZ in immunocompetent children, as in this case, is explained on the basis of immature immune system.[6]
To conclude, dermoscopy demonstrates characteristic patterns in HZ, which would assist the physician to differentiate it from similar kind of lesions such as insect bite reaction, herpes simplex, and irritant contact dermatitis. Dermoscopic features are well correlated with histopathological changes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Tzanck smear: A useful diagnostic tool. Indian J Dermatol Venereol Leprol. 2005;71:295-9.
- [Google Scholar]
- Standardization of dermoscopic terminology and basic dermoscopic parameters to evaluate in general dermatology (non-neoplastic dermatoses): An expert consensus on behalf of the international dermoscopy society. Br J Dermatol. 2020;182:454-67.
- [Google Scholar]
- Dermoscopy of general dermatological conditions in Indian population: A descriptive study. Clin Dermatol Rev. 2017;1:41-51.
- [Google Scholar]
- Early diagnosis of herpes zoster by handheld reflectance confocal microscopy. J Am Acad Dermatol. 2015;73:e201-3.
- [Google Scholar]
- Disease caused by viruses. In: DE Elder, R Elenitsas, M Rosenbach, GF Murphy, AI Rubin, X Xu, eds. Lever’s Histopathology of the skin (11th ed). Philadelphia: Wolters Kluwer; 2015. p. :781-815.
- [Google Scholar]
- Increased incidence of herpes zoster in normal children infected with varicella zoster virus during infancy: Community-based follow-up study. J Pediatr. 1986;108:372-7.
- [Google Scholar]





