Translate this page into:
Silicone in Dermatology: An Update
Address for correspondence: Dr. Simplepreet Kaur, Department of Dermatology, Venereology & Leprosy, Government Multispeciality Hospital, Sector 16, Chandigarh, India. E-mail: simple.warraich@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Silicones aka siloxanes are synthetic compounds, which contain siloxane bonds, i.e., the repeat unit –Si-O– with organic side groups such as methyl, ethyl, propyl, phenyl, fluoroalkyl, aminoalkyl, hydroxy, mercapto, hydrogen, and vinyl attached to the silicon atoms. They have ability to create short, long, or complex organosilicone oligomer and polymer particles. The siloxane bond in silicone is very strong and highly stable with nontoxic, noncarcinogenic, and hypoallergic properties. Silicone compounds have become one of the key ingredients in various skin care products namely moisturizers, sunscreen, color cosmetics, hair shampoos, etc. This review focuses on an update on various indications of silicone in dermatology. For this review, the literature search was conducted using keywords such as silicone and role of silicone.
Keywords
Silicone
silicone in dermatology
siloxanes
INTRODUCTION
Silicones aka siloxanes are synthetic compounds that were discovered in 1901 by British chemist F.S. Kipping.[1] Silicone is a long-chain inert polymer that contains siloxane bonds, i.e., the repeat unit –Si-O– with organic side groups such as methyl, ethyl, propyl, phenyl, fluoroalkyl, aminoalkyl, hydroxy, mercapto, hydrogen, and vinyl attached to the silicon atoms. Since they have a structure analogous to the ketones Si=O, they were called silicones. The basic structure is shown in Figure 1. This review focuses on an update on various indications of silicone in dermatology. For this review, the literature search of PubMed-indexed journals was conducted using keywords such as silicone, role of silicone, uses of silicone in dermatology, and silicone in dermatology.
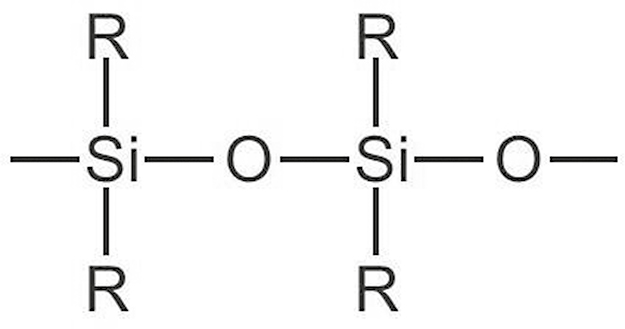
- Basic structure of silicone
Structure
Silicones have ability to create short, long, or complex organosilicone oligomer and polymer particles. The silicone structure may be linear, cyclic, branched, cross-linked first network and cross-linked second network.[2] The structure of most commonly used silicones, i.e., dimethicone, cyclopentasiloxane, and silsesquioxane, is depicted in Figure 2A–C, respectively.
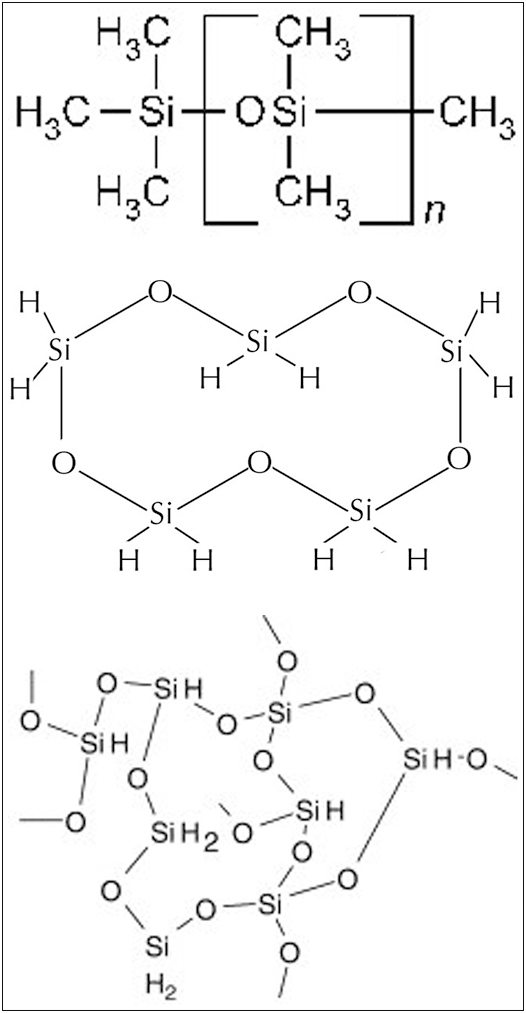
- (A) Structure of dimethicone. (B) Structure of cyclopentasiloxane. (C) Structure of silsesquioxane
Silicones are classified into various groups.[3]
-
-
Silanes
-
-
Hydroxyl-containing compounds (silanols): e.g., dimethiconol
-
-
Linear polysiloxanes: Dimethicone aka polydimethylsiloxane
-
-
Cyclic dimethyl siloxanes: Cyclomethicone aka decamethylcyclopentasiloxane
-
-
Silicates (inorganic)
-
-
Silsesquioxanes (RSiO3/2)n
CHARACTERISTIC PROPERTIES OF SILICONES
-
1.
The siloxane bond in silicone is very strong but at the same time highly flexible.
-
2.
The addition of different organic groups to the siloxane backbone renders diverse properties to silicones.
-
3.
Silicones can become hydrophobic by the addition of methyl groups as well as longer-chain hydrocarbons, whereas the addition of polar groups can produce water-soluble silicone.
-
4.
The Si-O bond is not easily oxidized.
-
5.
Nontoxic, noncarcinogenic, colorless, and odorless.
-
6.
Hypoallergenic.
-
7.
Water-repellent property.
-
8.
Incapable of being absorbed in body.
-
9.
Impermeable to bacteria.
-
10.
Does not interact with skin breathability.
-
11.
Highly stable:
Resistance to temperature (−100 to 250°C).
Resistance to moisture.
Resistant to decomposition from ultraviolet radiation, acids, alkalis, and ozone.
Aging resistance.
-
12.
No effect on immune system.
Dimethicone
It is the oldest and most extensively used silicone. It has a highly flexible polymer backbone. The change in the length and molecular weight of dimethicone polymer imparts different physical properties to dimethicone.[1] They are used in combination with emollients and moisturizers.
Silsesquioxanes
These are called polyhedral oligosilsesquioxanes (POSS) or cage silicones due to their 3D multiarmed structure.[3] The simplest form of POSS with hydrogen attached to the cage has low stability and solubility in formulations, but the attachment of organic groups to its core makes POSS more soluble and chemically stable.[3] In the chemical structure of silsequioxanes (RSiO3/2)n, the “R” groups used as substituents in the corners of the POSS cage include quaternary nitrogen, zwitterionic compounds, and different functional organic groups.[3] Silsesquioxanes are environment-friendly, recyclable, biocompatible, odorless, nonvolatile, and nontoxic under normal conditions.
SILICONE USE IN DERMATOLOGY
Moisturizers
Dimethicone is a key moisturizing ingredient in various formulations due to its ability to act as an occlusive, emollient, and artificial barrier.[4] It makes a thin layer on skin as it is a nongreasy occlusive agent. Dimethicone has the property of being insoluble in water but at the same time it is permeable to water vapor; thus, it will not reduce transepidermal water loss.[5] It has an aesthetic value for patients as it smoothens skin by filling in gaps where damaged corneocytes are missing from the stratum corneum.[4] There is an added advantage that dimethicone is hypoallergenic, noncomedogenic, colorless, and nonodorous.[5] Dimethicone is an ideal agent for incorporation into antiacne medications because of the moisturizing and barrier-enhancing benefits without creating a greasy shine undesirable in patients with acne.[4] Dimethicone and glycerin were the most common ingredients in a literature review of 52 online available moisturizers for acne.[6] The synergistic role of dimethicone in antiacne medications may increase compliance and tolerability to antiacne medications among patients with acne. So, facial moisturizers, which are silicone-based, are suitable for oily skin.[7]
Antiperspirants
Antiperspirants contain highly concentrated aqueous aluminum chlorohydrate emulsified in silicones. The silicone in the formulations facilitates application and easy spreadibility, reduces the tackiness of chlorohydrate, and evaporates without giving a chilling feeling.[8] Cyclomethicones in aerosol formulations are used in antiperspirants due to their dry feel and volatility, and the newer elastomer formulation has better aesthetic appeal. Silicones like cyclopentasiloxanes are used in antiperspirant stick formulations, where they provide the typical lubricating silicone feel.[1]
Color cosmetics
Silicones are used in color cosmetics as spreading agents for pigments as they have good spreadability, are nongreasy, and then evaporate, thus leaving a pigment film. The pigment/cyclomethicone combination is effective for producing wear-resistant cosmetics.[1]
Hair conditioners and shampoos
Hair conditioners are agents used to improve the feel and texture of hair and to decrease friction, hair tangling, and frizziness of hair. Silicones are the most active and used ingredient in hair conditioners.[9] Silicones by their film-forming action reduce interfiber friction and give shine, slip, and smoothness to hair that make them effective hair conditioning agents.[1] Silicones can be used for all hair types and in different hair care products like shampoos, rinse-off conditioners, hair masks, hair sprays, hair serums, hair oils, cuticle coats, hair styling products, and dye creams. Asian people have large hair diameters; therefore, a higher concentration of silicone is used as compared with that for Caucasian hair (3–5% vs. 0.5%).[10] Dimethicone, aminosilicones, and siloxysilicates are a few of the main ingredients in two-in-one shampoos.[9] Dimethicone has the effect of protecting the hair shaft from abrasive actions, whereas siloxysilicates increase hair body. Adding silicone to shampoos has its own challenges: (i) surfactants in shampoos remove silicone hair conditioning agents and (ii) water-insoluble silicones like dimethicone can reduce the amount of lather produced by the shampoo. These formulation challenges are addressed by the use of silicone polyethers that are water-soluble or water-dispersible in shampoos.[1] Another option is the use of amodimethicone, in which the amine groups become positively charged in aqueous solutions and can then deposit onto the hair due to the electrostatic force between amodimethicone and the negatively charged protein surface of the hair cuticle.[11] Silicones are also typically used in antidandruff shampoos as part of scalp care, where they have shown to increase compliance and also improved the feel and appearance of hair.[12]
Sunscreens
The challenge with an ideal sunscreen formulation is to provide the functional benefits of a sunscreen along with better acceptability so that sunscreens are applied in sufficient amounts to provide adequate protection. Silicones reduce the oiliness of sunscreen formulations and impart a light, nongreasy silky feel, which improves the consumer’s acceptance. Silicone emulsifiers have very low toxicity after topical application and have ability to impart a noticeable water resistance, which makes them quite beneficial.[13] Silicone elastomers, because of their cross-linked structure, swell in presence of certain solvents. This property enables them to take up adequate quantities of various oils, glycerides, sunscreens, and still remain dry to the touch, which makes them ideal therapeutic delivery agents for skin.[1] Alkyl-modified silicones such as stearyl dimethicone and cetyl dimethicone improve sunscreen performance by producing a thicker sunscreen film, thereby improving protection.[1] Phenyl silicones have shown good compatibility with organic sunscreens.[1] There are reports that adding 4% silicone elastomer can increase the sun protection factor value of a sunscreen formulation from ~5 to 18.[14] Silicones add more flexibility to a sunscreen formulation by increasing wash-off resistance and reducing oily and sticky feel of organic ultraviolet filters in sunscreens.[14]
Moisturizing body washes and cleansers
Moisturizing body washes are formulated to deposit skincare ingredients (moisturizers) onto the skin during and after the cleansing process. Dimethicone, silicone polyethers are added in body washes to improve the foam quality and create a creamier, more stable foam.[14] Similarly, nonrinsable makeup removers and cleansers also contain polydimethylcyclosiloxane and their derivatives since they act as good solvents for organic-based oils and, in addition, give a shiny, silken, and nongreasy feel on human skin.[14] Cyclomethicone and various properties of low molecular weight silicones such as low surface tension, good wetting properties, and the capacity to eliminate dirt or color cosmetic residues are utilized in makeup removal cleansers.[14]
Antiageing and age masking creams
While there are various topical pharmacological agents with antiageing properties in a dermatologist’s armamentarium, there is a need for products that mask the wrinkles and fine lines on skin and project the natural skin tone. In a young face, the reflection of light from the surface is largely diffused naturally giving a visual perception of softness and firmness, which is called natural soft focus. With increased age, this natural soft focus effect is lost, and the lines and furrows increase the skin contrast and negatively affect the perception of skin. The lines and wrinkles in an aging face trap light in crevices and cause the skin tone to look uneven. The pigments from makeup and foundation also tend to collect in skin crevices and accentuate fine lines and wrinkles. The silicone elastomer particles create a layer on the skin that scatters light, thereby obscuring the underlying shadow that the fine wrinkles create.[1] The soft focus effect created by silicon elastomeric particles makes the natural skin tone show through to give a natural glow and even out the skin by hiding imperfections.
Wound dressings
Silicone is an ideal material for wound contact layer dressings—dressings applied directly to a wound to protect it from direct contact with harmful substances and ensure an appropriately moist environment to promote healing without maceration. Silicone has a property to adhere to the periwound skin and not to the wound bed; thus, it is less likely to result in skin damage and pain on removing dressing.[15] The various silicone-based dressings include bistretch soft silicone, soft silicone mesh, soft silicone fixation tape, soft silicone foam, and soft silicone foam with superabsorber.[15] These have been used successfully in the treatment of pressure ulcers, burns, and blistering diseases, such as epidermolysis bullosa (EB), Bullous Pemphigoid, and Hailey-Hailey disease. In a randomized study of 366 patients in an intensive care unit, it was found that a soft silicone foam dressing applied over the sacrum lowered the incidence of pressure ulcers (0.7%) compared with the no-dressing control group (5.9%).[16] A systematic review done to evaluate the effectiveness of dressings in preventing pressure ulcers concluded that silicone dressings can reduce the incidence of pressure ulcers though the certainty of the evidence was low.[17] Silicone dressings have been recommended for wound care in patients with EB.[1819]
The soft silicone dressings are used for dry to lightly exudative chronic wounds of EB. These are porous, semitransparent, and provide gentle adhesion. They have a wear time of 3–4 days. The disadvantages are that the adherence may be too strong on fragile skin, and a risk of overgranulation can be there.[17]
The soft silicone foam dressing is used on exudative wounds as it can absorb exudate and provide a degree of protection to wound. It is an absorbent dressing made from polyurethane foam, the outer surface of which is bonded to a vapor-permeable polyurethane membrane that acts as a barrier to fluid and microorganisms.[18] The inner surface of the foam is coated with a layer of soft silicone that helps to hold the dressing in place without sticking to the surface of the wound or causing trauma to delicate new tissue on removal. The wear time is 3–4 days. There is a risk of adherence if placed directly on wound bed so used over soft silicone mesh.[18]
Soft silicon tape and adhesives
The soft silicone tapes and adhesives should be used in place of normal adhesive tape in patients of blistering disorders, e.g., EB and toxic epidermal necrolysis. If intravenous access is necessary, the cannula should be secured using silicone-based tapes instead of adhesive tapes. In contrast to conventional adhesives, silicone adhesives have lower surface tension; therefore, they hold onto skin’s natural lines and curves and create a steady bond.[15] The adhesion with silicone is rapid and remains constant with time compared with traditional adhesives.[15] These properties help reduce discomfort on removal due to less peel force and less susceptibility for epidermal cell stripping.[15] Besides the advantages of silicone adhesives, they adhere poorly to other silicone products and plastics, so should be avoided there, and also due to lack of evidence, silicone adhesives should be avoided in primary securement of critical tubing.[15]
Silicone medical adhesive removers
Medical adhesive removers are used to abet removal of adhesive products, but these can strip layers of the stratum corneum, causing skin injury and discomfort to the patient. It is used to remove adhesive materials such as tapes (used for securing intravenous canulae, central lines, and nasogastric tubes), clothing and bedding adhered to wounds and erosions. The different types of medical adhesive removers include alcohol or organic solvent-based, oil-based, or silicone-based.[15] Of these, the silicone-based removers are the newest, which have benefited the management of EB and are strongly recommended.[19] The disadvantage of oil-based solvents is that it results in persistant stickiness, which can impede the adhesion of the next appliance to be placed on the peristomal skin.[20] The silicone-based removers have been shown to reduce peel force by as much as 81% and are devoid of stinging sensation and pain associated with other alcohol-based medical adhesive removers.[20] There is a newer formulation of silicone medical adhesive remover as spray and sterile sachets.[20]
Silicone barrier films
The most common peristomal skin complication is contact dermatitis, which occurs due to prolonged exposure of skin to potential irritants (urine, feces, and wound exudates) from stoma. This can manifest as irritation, redness, burning sensation, and pain. The barrier films are available as powder, paste, wipes, or sprays, and are applied directly to the peristomal skin before the appliance is fitted.[21] Barrier seals or rings made of silicone and hydrocolloid can be molded around the stoma and they fit in uneven skin contours around the stoma and on the peristomal skin.[21] Silicone-based barrier films are long-lasting and pain-free, and various formulations have been developed that protect the skin from chemical irritants like stomal effluent, urine, and feces, and soothen the damaged skin. The silicone-based barrier films have an advantage over alcohol-based peristomal products since it causes negligible pain on application. Dimethicone being permeable to water vapor allows evaporation of perspiration and minimizes the risk of miliaria, and it is easy to spread and feels less greasy on skin.[22]
Silicones in treatment of hypertrophic scars and keloids
Silicone gels (SGs) and SG sheeting are both used to help reduce scarring. It has been reported to produce 86% reduction in texture, 84% in color, and 68% in height of scars.[23] The international advisory panel for hypertrophic scar and keloid management recommend SG sheeting as a reasonable first-line treatment choice for hypertrophic scars and keloids.[23] The exact mechanism of action of SG is not known but numerous studies have cited improved occlusion and hydration to wound bed to play a key role.[24] SG acts as a flexible hydrophobic barrier, causes temperature regulation, and increases hydration at site of scar, which is responsible for reduced capillary activity, hyperemia, and collagen deposition.[24] According to Gilman et al., [25] silicone sheets decrease the water vapor evaporation rate causing a buildup of moisture on the skin surface. Tumor growth factor (TGF) encourages fibroblasts to produce fibronectin and collagen. Fibroblast growth factor (FGF) increases the number of collagenases, which breaks down the extra collagen, and normalizes the collagen synthesis in an aberrant scar. FGF and TGF expressions are both modulated by silicone. Eventually, the balance between fibrogenesis and fibrolysis is restored.[23] It protects the scarred tissue from bacterial invasion and prevents the excessive collagen production in the scar tissue induced by bacteria.[23]
Method of application
Silicone can be applied to the skin in the form of a topical SG applied twice a day or an SG sheet for 12–20 h/day with daily washing for a period ranging from 3 to 6 months.
Advantages
Topical SG is nonocclusive, waterproof, and gas permeable, and has ease of application. It can be applied on even sensitive skin, children, any irregular skin or scar surfaces, the face, moving parts (joints and flexures), and any size of scars.[23]
A new alternative to topical silicone is a combination of silicone oil with hypochlorous acid (HOCL); it is a gel or spray that can be applied twice daily. HOCL has an antimicrobial, antipruritic, and anti-inflammatory role by increasing oxygenation and disrupting biofilm formation. So for scar management and wound healing in immediate postoperative period, the combination hydrogel of HOCL and silicone can be useful.[26]
Treatment of pediculosis capitis
Dimethicone 4% lotion is a physically acting pediculicidal compound based on 4% high molecular weight dimeticone in a cyclomethicone base.[27] Burgess and Burgess[28] demonstrated a good ovicidal and pediculicidal action of dimethicone 4% gel after a single 15-min application. The limitation in its use is the excessive fluidity of the dimethicone lotion and dripping of the active agent away from hair root, thereby rendering it ineffective.[27] Another study found dimethicone product to be safe and more efficacious than permethrin.[29] Resistance to dimethicone is unlikely due to its physical mode of action.[30]
Silicone granulomas and liquid injectable silicone
Injected silicone is food and drug administration -approved only for intraocular injections in the treatment of retinal detachment.[31] Although it is not food and drug administration-approved for soft tissue augmentation, it is used off-label by some practitioners to correct human immunodeficiency virus-associated facial lipoatrophy.[31] In surveys done in transgender population in the United States, the prevalence of illicit silicone use has been reported to be 16.7% in a 2013 population-based sample of trans women in San Francisco.[31] Silicone injections are often administered on breast, hips, and buttock regions by male to female transsexuals to achieve a more feminized appearance. Illicit “silicone”, which is industrial grade as opposed to medical-grade silicone, is used in various cases. The dermatologist needs to be aware of the complications postsilicone injections, which might take days to years to manifest.[31]
The major drawback of silicone injection is a high rate of foreign body granuloma after both industrial-grade and medical-grade fluid silicones. Tables 1 and 2 mention the various complications of injected silicone and treatment options for silicone granuloma, respectively.31323334
| Time gap from injection | Complications |
|---|---|
| Immediate: Seconds to minutes | Arterial occlusion |
| Venous occlusion | |
| Discoloration of the skin | |
| Postinjection papules and pain | |
| Redness | |
| Ecchymosis | |
| Swelling | |
| Hypersensitivity reaction | |
| Early: Days to weeks | Pain |
| Ecchymosis | |
| Pigmentation | |
| Inflammatory nodules | |
| Pruritus | |
| Late: Months to years | Inflammatory nodules |
| Silicone granuloma |
| Treatment options | Indication |
|---|---|
| First-line therapy | |
| Antibiotics for 4–6 weeks – | These target delayed inflammatory nodules, granulomas, and sterile abscesses |
| • Minocycline: 100 mg PO BID | |
| • Tetracycline: 500 mg PO BID | |
| • Combination of tetracycline with Clarithromycin 500 mg PO BID for 2 weeks | |
| Refractory therapy | |
| NSAIDs | Added along with oral antibiotics to dampen granulomatous inflammatory reaction |
| Oral and intralesional steroids (recommended dose of 2.5–10 mg/mL every 3–4 weeks) | Used if refractory to oral antibiotics and NSAIDS for 4–6 weeks |
| Novel therapy | |
| Imiquimod | Antiproliferative action |
| Etanercept: 25–50 mg subcutanceous twice a week | TNF-α inhibition |
| Adalimumab: 40 mg subcutaneously every 2 weeks | |
| Tacrolimus: 0.8–1.0 mg/kg PO BID | Inhibit T-cell activation, interferon, and the release of preformed mediators from mast cells and basophils |
| Allopurinol: 300 mg PO daily | Inhibits granuloma formulation by targeting xanthine oxidase |
| Isotretinoin: 0.5 mg/kg/day PO | Anti-inflammatory property |
| Surgical excision | If nodules are well circumscribed, and clear margins exist to ensure feasible removal |
Silicone toxicity and environmental concerns
The fast spread of silicone use in various fields raises concern about any toxic adverse effects of these compounds on environment. Studies on safety of cyclomethicones have shown the products tested to be safe as cosmetic ingredients.[1] The cyclic siloxanes in the atmosphere rapidly break down when exposed to oxygen and ultraviolet radiation from sunlight and produce silica and carbon dioxide.[1] There is concern about few silicones, which are nonbiodegradable and have potential to accumulate in food chain but studies have been inconclusive so far. The silicones added in wash-off personal care products are considered to have the highest environmental risk. Since a big share of our cosmeceutical products contains silicone, regular surveys and scientific research should be done to be mindful of the various environmental and ecological risks associated with unrestricted use of silicone.
CONCLUSION
Silicone compounds have become one of the key ingredients in various skin care products in the last 1 decade. This fast growth of silicone compounds is large because of the better understanding of the various properties: bio inertness, stability, flexibility, nontoxicity, good tissue compatibility, and antiadhesive properties. Silicone polymers have revolutionized various skin and hair care products besides being used in specific dermatological therapies for scar management and wound healing. With the advancement in technology and research, silicones may play a greater role in skin therapies in the form of newer formulations, newer derivatives, and multifunctional silicones. The growing demand for aesthetically pleasing products may boost the development of more silicon-based skin products in the future.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Formulating skin care products with silicones: Approaches and strategies. In: Dayan N, ed. Handbook of formulating dermal applications: A definitive practical guide (2nd ed). Hoboken, NJ: Wiley; 2017. p. :59-114.
- [Google Scholar]
- Direct human contact with siloxanes (silicones) - Safety or risk part 1. Characteristics of siloxanes (silicones) Front Pharmacol. 2016;7:132.
- [Google Scholar]
- Silsesquioxanes in the cosmetics industry-Applications and perspectives. Materials (Basel). 2022;15:1126.
- [Google Scholar]
- The effect of vehicle formulation on acne medication tolerability. Cutis. 2008;82:281-84.
- [Google Scholar]
- Moisturizers for acne: What are their constituents? J Clin Aesthet Dermatol. 2014;7:36-44.
- [Google Scholar]
- Shampoo and conditioners: What a dermatologist should know? Indian J Dermatol. 2015;60:248-54.
- [Google Scholar]
- Shampoo compositions. In: Preedy VR, ed. Handbook of hair in health and disease (1st ed). Wageningen, The Netherlands: Academic Publishers; 2012. p. :435-47.
- [Google Scholar]
- A comparison of hair quality and cosmetic acceptance following the use of two anti-dandruff shampoos. J Investig Dermatol Symp Proc. 2005;10:201-4.
- [Google Scholar]
- Effects of silicone emulsifiers on in vitro skin permeation of sunscreens from cosmetic emulsions. J Cosmet Sci. 2004;55:509-18.
- [Google Scholar]
- Silicone copolymers for healthcare and personal care applications. In: He C, Li Z, eds. Silicon containing hybrid copolymers (1st ed). Weinheim, Germany: Wiley-VCH Verlag GmbH& Co.KGaA; 2020. p. :145-66.
- [Google Scholar]
- Medical adhesives and patient safety : State of the scienceconsensus statements for the assessment, prevention, and treatment of adhesive-related skin injuries. J Wound Ostomy Cont Nurs. 2013;40:365-80.
- [Google Scholar]
- Selection of appropriate wound dressing for various wounds. Front Bioeng Biotechnol. 2020;8:182.
- [Google Scholar]
- Wound management for children with epidermolysis bullosa. Dermatol Clin. 2010;28:257-64.
- [Google Scholar]
- A consensus approach to wound care in epidermolysis bullosa. J Am Acad Dermatol. 2012;67:904-17.
- [Google Scholar]
- Silicone-based adhesive removers for preventing peristomal skin complications caused by mechanical trauma. Gastrointestinal Nursing. 2019;17:S22-8.
- [Google Scholar]
- Ostomy 101 for dermatologists: Managing peristomal skin diseases. Dermatol Ther. 2021;34:e15069.
- [Google Scholar]
- Management of moisture-associated skin damage: A scoping review. Adv Skin Wound Care. 2017;30:494-501.
- [Google Scholar]
- The efficacy of silicone gel for the treatment of hypertrophic scars and keloids. J Cutan Aesthet Surg. 2009;2:104-6.
- [Google Scholar]
- The use of silicone adhesives for scar reduction. Adv Wound Care (New Rochelle). 2015;4:422-30.
- [Google Scholar]
- Silicone sheet for treatment and prevention of hypertrophic scar: A new proposal for the mechanism of efficacy. Wound Repair Regen. 2003;11:235-6.
- [Google Scholar]
- Topical stabilized hypochlorous acid. The future gold standard for wound care and scar management in dermatologic and plastic surgery procedures. J Cosmet Dermatol. 2020;19:270-7.
- [Google Scholar]
- Dimeticone 4% liquid gel found to kill all lice and eggs with a single 15 minute application. BMC Res Notes. 2011;4:15.
- [Google Scholar]
- A highly efficacious pediculicide based on dimeticone: Randomized observer blinded comparative trial. BMC Infect Dis. 2008;8:115.
- [Google Scholar]
- Nonmedical-grade injections of permanent fillers: Medical and medicolegal considerations. J Clin Aesthet Dermatol. 2013;6:22-9.
- [Google Scholar]
- A case of recalcitrant silicone granuloma treated with adalimumab: A case report. SAGE Open Med Case Rep. 2022;10:2050313X221093444.
- [Google Scholar]
- Siliconoma successfully controlled with low-dose oral isotretinoin: A case report with histopathologic and ultrasonographic findings. JAAD Case Rep. 2021;14:24-6.
- [Google Scholar]






