Translate this page into:
Use of Intralesional Deoxycholic Acid for Antiretroviral Treatment Associated Lipohypertrophy: A Qualitative Open-Label Study of an Innovative Indication
Address for correspondence: Dr. Tejaswini S. Salunke, Department of Dermatology, Deenanath Mangeshkar Hospital and Research Center, Erandwane, Pune 411004, Maharashtra,, India. E-mail: winialways@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
With the advent of antiretroviral treatment (ART), human immunodeficiency virus/AIDS has become a chronic manageable disease. Though life expectancy has improved, it brings alongside effects of long-term medical treatment. One of the major side effects is body dysmorphism, which leads to esthetic problems. Problems of lipodystrophy (LDS), especially facial lipoatrophy as well as facial and upper back lipohypertrophy are perceived by patients as highly stigmatizing manifestations of their human immunodeficiency virus infection. It has been reported to affect mood and quality of life, as well as reduced adherence to antiretroviral medications. Patients feel discomfort while sleeping, dressing, and during day-to-day activities.
Aim:
The aim of this study was to test a relatively cost-effective and efficacious treatment modality for long-standing ART-associated lipohypertrophy of the submental fat and dorsocervical fat.
Materials and Methods:
This was a prospective open-label clinical study, in which 21 patients on regular ART with associated lipohypertrophy were enrolled in this open-label study. Deoxycholic acid (DCA) was given intralesionally once every 4–6 weeks. Patients were assessed for response, any adverse events, and patient satisfaction during every visit.
Results:
Intralesional DCA seems to be a promising treatment modality for long-standing ART-induced LDS with better cost-benefit in comparison with surgical interventions.
Limitations:
It was a small-sized sample that was studied. The lag time between starting the treatment and optimum results was long in comparison with liposuction. The result is better appreciated at the end of treatment rather than after every session implying that it has a cumulative effect. Neither pre- and post-ultrasonography nor metric documentation was done.
Conclusions:
Intralesional DCA seems to be a promising treatment modality for long-standing ART-induced LDS with better cost–benefit in comparison with surgical interventions.
Keywords
ART induced lipohypertrophy
buffalo fat
dorsocervical fat
double chin
HIV-induced lipohypertrophy
intralesional deoxycholic acid
submental fat
INTRODUCTION
With the advent of antiretroviral treatment (ART) human immunodeficiency virus (HIV)/AIDS has become a chronic manageable disease.
Apart from longevity, good quality of life has become an important goal of treatment. Though life expectancy has improved, several long-term side effects due to long-term medical treatment have been observed. The most apparent one is the development of characteristic changes in body fat redistribution, known as the HIV-associated adipose redistribution syndrome (HARS) or HIV-induced lipodystrophy (HIV-LDS)[1] which leads to esthetic problems. Problems of LDS, especially facial lipoatrophy as well as facial and upper back lipohypertrophy are perceived by patients as a highly stigmatizing manifestation of their HIV infection. It is more commonly seen in patients on protease inhibitors (PIs) or the old generation nucleoside reverse transcriptase inhibitors (NRTIs) such as Stavudine and Zidovudine. It has been reported not only to affect mood and quality of life, but also to reduce adherence to antiretroviral medications. Patient feels discomfort while sleeping, dressing, and during day-to-day activities. It is linked to depression, decreased self-esteem, sexual dysfunction, and social isolation. Injection lipolysis has been shown to be effective in treating localized fat over submental region (submental fat—SMF), flanks, bra-line, abdomen, etc., in obese individuals but there have been no studies which showed their efficacy in long standing lipohypertrophy such as HIV-LDS.
MATERIALS AND METHODS
Study design
This was a prospective qualitative open-label clinical study carried out on 21 HIV-positive patients.
Inclusion criteria
The inclusion criteria of the study included the following:
Patients who were on long-term ART, more than 15 years, and with prominent lipohypertrophy either over the dorsocervical region or submental region (SMF) were enrolled.
Exclusion criteria
The exclusion criteria of the study included the following:
Psychological factors: Unrealistic expectations, indecisiveness, dysmorphophobia, family members disapproving of the treatment.
Allergy to soy protein [as deoxycholic acid (DCA) is derived from soy] and topical anesthetic agent were excluded.
All patients were counseled about the use, benefits, anticipated results, and the duration that would be required to achieve the results.
Routine tests such as hemogram, lipid profile, Cluster of differentiation 4 cell counts, and HIV viral load tests done < 6 months were considered.
Most of our patients were on lipid lowering agents like statins or fibrates but with no significant change in the localized fat.
Photographic imaging was done before starting the intervention and on every follow-up visit, which was 4–6 weeks apart.
After informed consent, patients were again counseled regarding the expectations, side effects, and duration of the treatment.
Treatment
Injection DCA (10 mg/mL) in a 5 mL vial was used for individual patient.
Procedure
Area to be treated was selected for each patient. As many of our patients had both SMF and dorsocervical fat accumulation, the choice which one to select was left solely to the discretion of the patient, keeping in mind his or her needs.
The area was marked by palpating the border outlines. Topical anesthetic cream was applied for 45 min, for patients with low threshold of pain. Cold compress using an ice pack was given for 15–20 min before the procedure.
After all aseptic precautions 1 square cm grid was made covering the entire area [Figure 1]. 0.2–0.4 mL DCA was injected in each grid tangentially at an angle of 45° using a tuberculin syringe, 26 number needle ½ inch length with depth enough to reach the middle of the fat pad, about 6–10. Maximum of 5 mL was used in each session. Vibratory anesthesia was used to reduce the pain during injecting DCA. Patients were assessed for response, any adverse events, and patient satisfaction during every visit. Photographic documentation was done during every treatment session. This was repeated after 4–6 weeks to maximum of eight sessions in total. Topical 2% Mupirocin ointment was applied after procedure. In case of pain, patient was advised to take oral paracetamol tablet 500 mg twice a day or as per requirement. Adverse events such as pain, tenderness, and lumpiness and their duration were asked and noted.

- Showing grid marking before injecting DCA intralesionally
RESULTS
Patients’ demographic and baseline characteristics
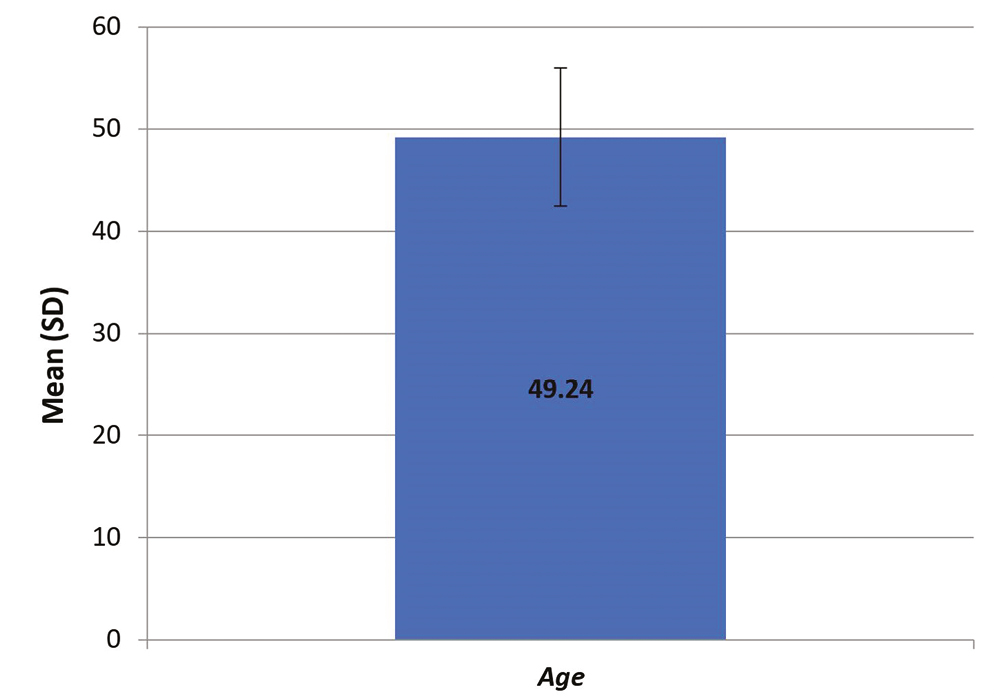
In total, 21 patients were enrolled, of which 8 were female and 13 were male. The mean age was 49.24 years. Age range was 33–58 years [Graph 1].
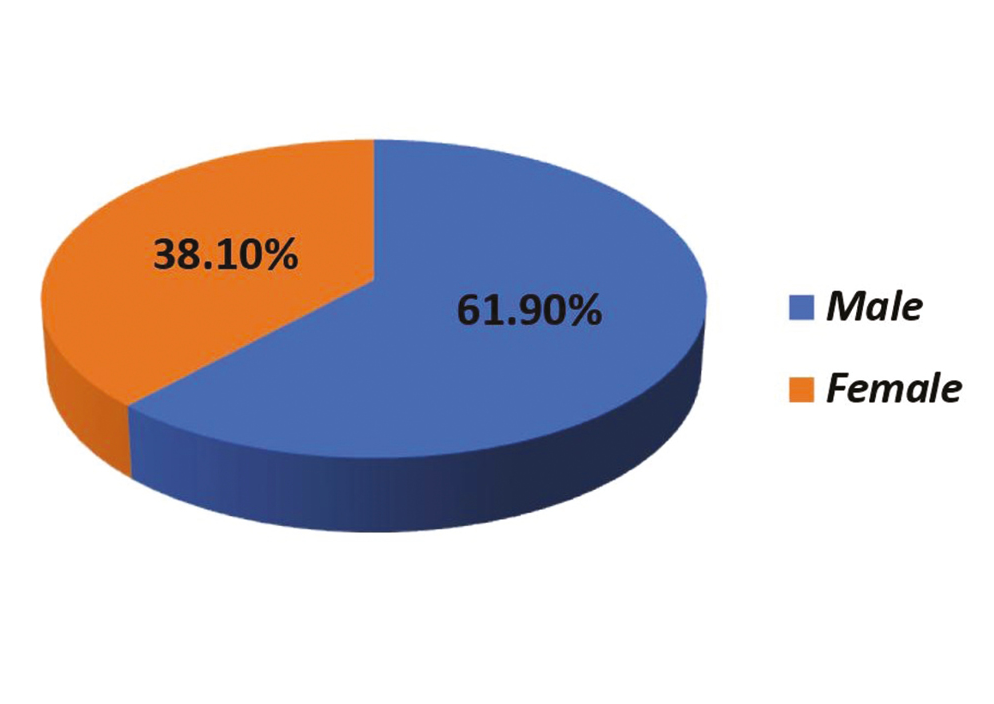
- Age distribution
Procedural outcome
A total 21 patients were treated using DCA intralesionally with 168 sessions.
Eight patients required six sessions, five required seven sessions and six required eight sessions to be satisfied by the outcome, and two patients were not satisfied in spite of eight sessions [Graph 2].
Last follow-up was done 6 weeks after the last session.
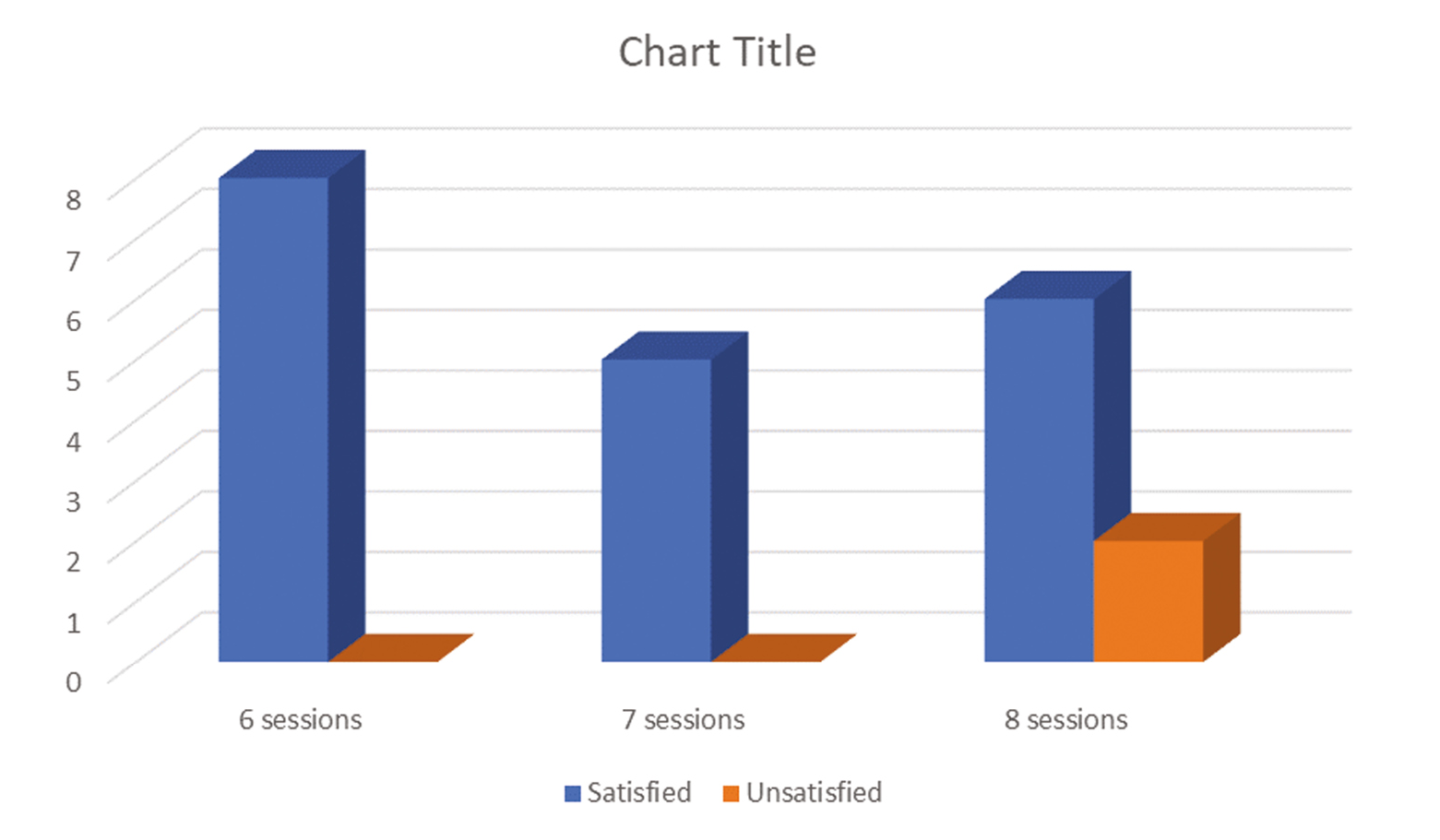
- Patient outcome score at 6, 7, and 8 sessions
Figures 2–4 show treatment outcome in comparison to the first visit and 6 weeks after last session.

- Showing before and after images of patients
Treatment outcomes
Degree of patient satisfaction is shown in Table 1 and Graph 2.
| Frequency | % | ||
|---|---|---|---|
| Valid | Not satisfied | 3 | 14 |
| Fairly satisfied | 9 | 43 | |
| Satisfied | 7 | 33 | |
| Very satisfied | 2 | 10 | |
| Total | 21 | 100 | |
The patients were asked to gauge their satisfaction level, whether they were very satisfied, satisfied, fairly satisfied, or not satisfied at all. Two patients (10%) were very satisfied, seven patients (33%) were satisfied, nine patients (43%) were fairly satisfied, and three patients (14%) were not satisfied.
Of the three unsatisfied patients, two had completed the planned number of eight sessions of DCA injection, and one completed six.
Treatment outcome was assessed with visual analog scale (VAS) score from 1 to 10 [Table 2]. Each case was assessed by two dermatologists who did not perform the treatment and those who did not know the characteristic of the treatment and gave their own assessment in terms of physician assessment scale [Table 3 and Graph 3]
| Frequency | % | ||
|---|---|---|---|
| Valid | 2 | 1 | 4.8 |
| 4 | 1 | 4.8 | |
| 5 | 3 | 14.3 | |
| 6 | 2 | 9.5 | |
| 7 | 5 | 23.8 | |
| 8 | 7 | 33.3 | |
| 9 | 2 | 9.5 | |
| Total | 21 | 100.0 | |
| Frequency | % | ||
|---|---|---|---|
| Doctor’s view 1 | |||
| Valid | 2 | 1 | 4.8 |
| 4 | 1 | 4.8 | |
| 5 | 1 | 4.8 | |
| 6 | 6 | 28.6 | |
| 7 | 3 | 14.3 | |
| 8 | 7 | 33.3 | |
| 9 | 2 | 9.5 | |
| Total | 21 | 100.0 | |
| Doctor’s view 2 | |||
| Valid | 1 | 1 | 4.8 |
| 4 | 1 | 4.8 | |
| 6 | 4 | 19.0 | |
| 7 | 5 | 23.8 | |
| 8 | 8 | 38.1 | |
| 9 | 2 | 9.5 | |
| Total | 21 | 100.0 | |
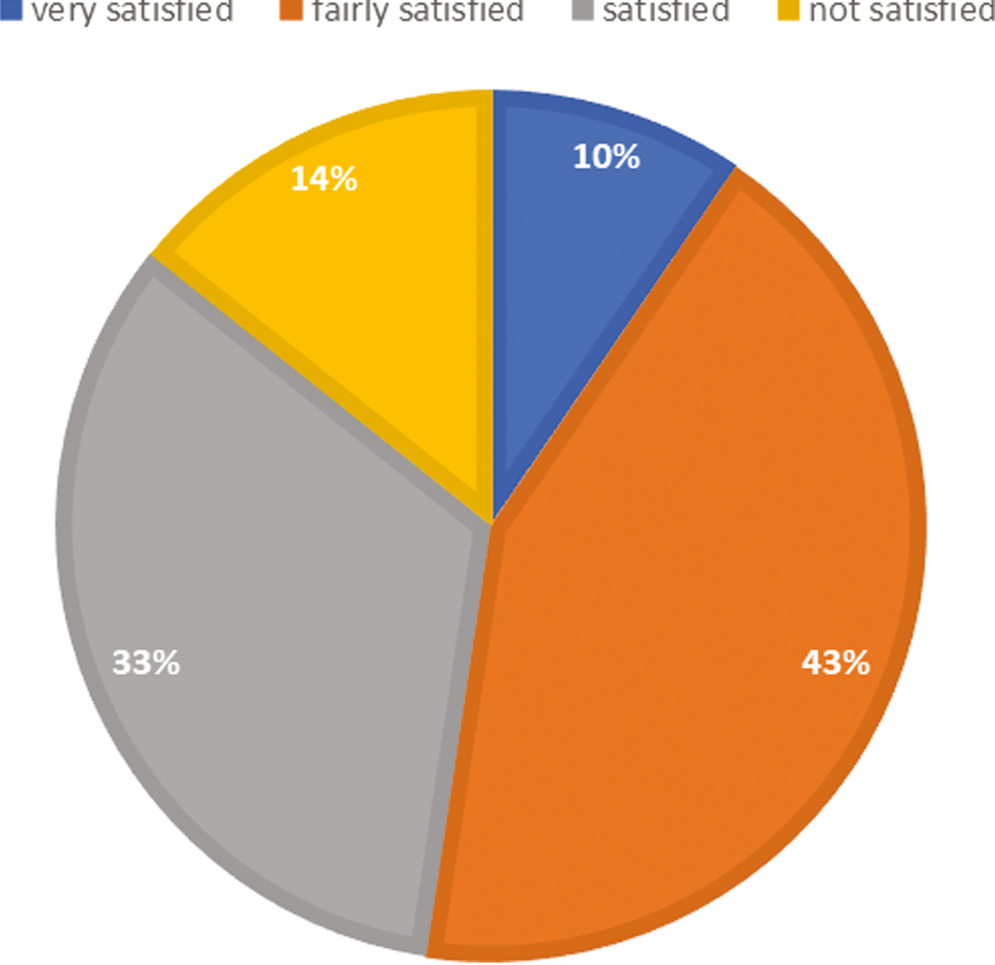
- Patient satisfaction score
Statistical analysis
Descriptive and inferential statistical analyses were carried out. Results on continuous measurements were presented on mean ± standard deviation and results on categorical measurement were presented in number (%). Level of significance was fixed at P = 0.05 and any value less than or equal to 0.05 was considered to be statistically significant.
Analysis of variance (ANOVA) was used to find the significance of study parameters between the groups (inter-group analysis). Further post hoc analysis was carried out if the values of ANOVA test were significant [Tables 4 and 5, Graphs 4 and 5].
| Group | N | Mean | Standard deviation | F value | P value |
|---|---|---|---|---|---|
| Patient’s view | 21 | 6.76 | 1.758 | 0.083 | 0.921 |
| Doctor’s view 1 | 21 | 6.76 | 1.700 | ||
| Doctor’s view 2 | 21 | 6.95 | 1.802 | ||
| Total | 63 | 6.83 | 1.728 |
| Patient’s view | Doctor’s view 1 | Doctor’s view 2 | |
|---|---|---|---|
| Patient’s view | – | 1.000 | 0.934 |
| Doctor’s view 1 | 1.000 | – | 0.934 |
| Doctor’s view 2 | 0.934 | 0.934 | – |
- With visual analog scale (VAS) score from 1 to 10 and physician assessment score by two dermatologists who did not perform the treatment and those who did not know the characteristic of the treatment
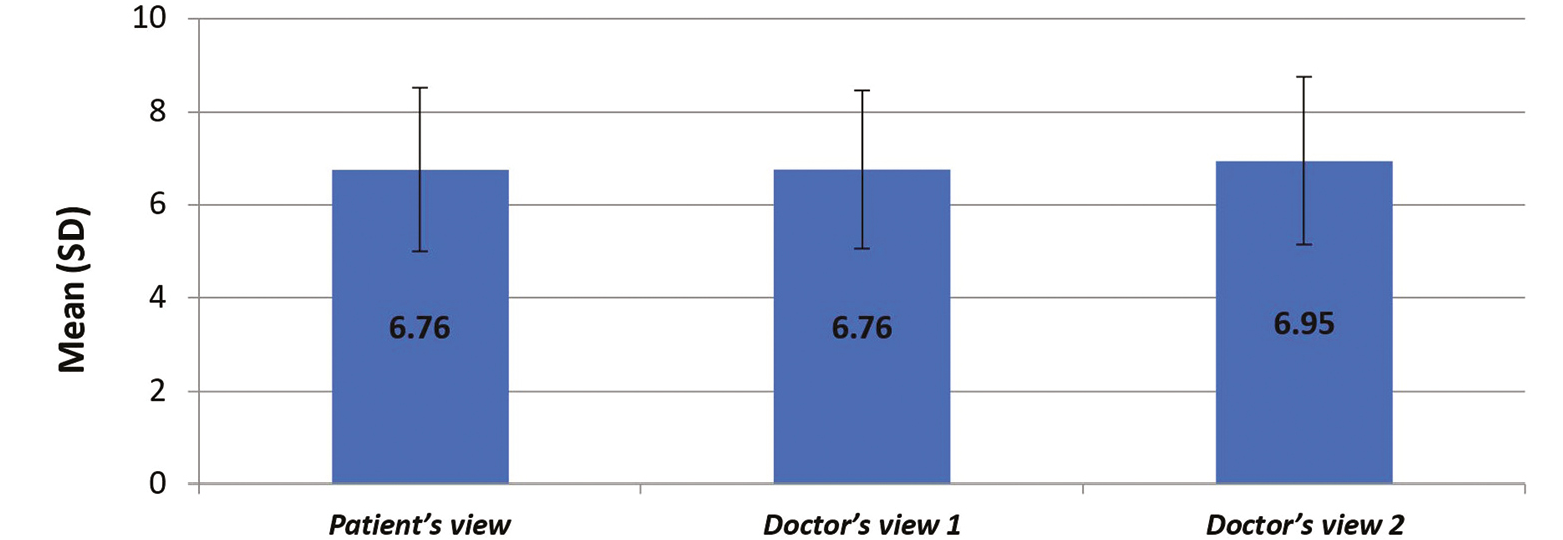
- Showing analysis of variance (ANOVA) showing significance of study parameters between the groups
The statistical software IBM SPSS Statistics 20.0 (IBM Corporation, Armonk, NY) was used for the analyses of the data, and Microsoft Word and Excel were used to generate graphs, tables, etc.
A short questionnaire was filled by the patients to monitor their side effect profile including erythema, pain, nodules, swelling, necrosis, etc.
Most common side effect noticed was pain (50.%) but with the use of topical anesthesia and vibratory anesthesia, it was substantially reduced. The pain was mostly due to the needle prick and subsided immediately. Heaviness was noticed for 24–48 h, which subsided with or without paracetamol tablet 500 mg orally [Table 6].
| Frequency | % | ||
|---|---|---|---|
| Valid | A | 3 | 8.33 |
| Pain | 18 | 50.0 | |
| Erythema | 11 | 30.55 | |
| Nodules | 4 | 11.11 | |
DISCUSSION
HIV-LDS includes hypertrophy in the (buffalo hump), SMF, increased fat in abdominal region, gynecomastia, and loss of fat in the mid face and extremities.[2] It is considered as a major side effect of the therapy. Evidence suggests that HIV-LDS affects up to half or even more HIV infected patients receiving ART.[3]
Its hallmark is dyslipidemia with changes in lipid profile, which presents before distinctive clinical features of fat redistribution become apparent.[4] Most common drugs causing it are NRTIs and PI. There have been studies showing increased cholesterol and triglyceride levels in HIV negative patients receiving ritonavir for 2 weeks.[5] Direct dyslipidemia induced by PIs can develop rapidly in comparison to NRTIs in highly active antiretroviral therapy.[6] The drugs also influence adipose tissue. Ritonavir, lopinavir, and saquinavir inhibit adipocyte differentiation. Nelfinavir has also shown an effect on adipocytes, thus could result in abnormal functioning of subcutaneous tissue. Hypertriglyceridemia in HIV patients could be a response to systemic inflammatory response against persistent viral infection in the body.
Despite this, withdrawal of ART is not an option. Managing of lipid abnormalities with current treatment guidelines for HIV-negative population is required using statins and fibrates. The effect of these antidyslipidemic drugs on visceral fat is noted but the effect on peripheral fat accumulation is doubtful.[7]
In such a situation, an interventional therapy is required. Liposuction carried out by plastic surgeons has been the mainstay of treating localized fat; however, it has not been effective in HIV-LDS as the quality of fat accumulated is different, and its consistency is thicker. It is an invasive procedure and performed under general anesthesia and expensive too. Moreover, fatal complications such as fat embolism and sepsis, though rare, are also a possibility. Localized injections of phosphatidyl choline and DCA have gained popularity to reduce the superficial deposits of fat in recent years without serious side effects. DCA is a naturally occurring bile salt that emulsifies the fat and causes disruption of the phospholipid bilayer of the adipocytes which leads to fat cell death, which is then slowly removed by macrophages. This results in reduction in fat in the area that is being treated.[8] It has a non-selective cell-lysis ability; however, the affinity is lower in proteinaceous tissues as against fatty tissue, thus making adipose tissue more susceptible to DCA in comparison to the surrounding tissue.[9] The rapid attenuation of DCA detergent activity by proteins and the transport of DCA to the endogenous bile pool, the activity of DCA is spatially limited and thus targeting the injected tissue. It is considered to be biocompatible detergent with potential use as a therapeutic agent. Various studies show its efficacy and safety in SMF in the obese population.[10] Our study has demonstrated, for the first time, to the best of our knowledge its use and implications in HIV-LDS. However, it was a small-sized sample that was studied. The lag time between starting the treatment and optimum results was long in comparison with liposuction. The result is better appreciated at the end of treatment rather than after every session implying that it has a cumulative effect. No pre and post ultrasonographic or metric documentation was done. As HIV-induced lipohypertrophy is almost always long-standing, the type of fat deposition is different, that is, it is not easily compressible or uniform and thus takes a longer time for complete resolution.
CONCLUSION
DCA is being used widely in obese population with rewarding results.
Its use in HIV-LDS is novel. It definitely has expanded the horizons. Our patients were on long-term ART with stubborn SMF and dorsocervical fat DCA injections gave symptomatic relief and cosmetic appeal too. Its efficacy needs to be explored on a larger scale with metric documentation either using calipers or ultrasonography of the fat accumulated to find the size and volume.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Lipodystrophy syndrome in HIV infection: what is it, what causes it and how can it be managed? Drug Saf. 2000;23:57-76.
- [Google Scholar]
- Biochemical manifestation of HIV lipodystrophy syndrome. Int J MCH AIDS. 2012;1:92-101.
- [Google Scholar]
- Prevalence of lipodystrophy and dyslipidemia among patients with HIV infection on generic ART in rural South India. J Int Assoc Physicians AIDS Care (Chic). 2012;11:329-34.
- [Google Scholar]
- Biochemical manifestation of HIV lipodystrophy syndrome. Int J MCH AIDS. 2012;1:92-101. 10.21106/ijma.6. PMID: 27621962; PMCID: PMC4948165
- [Google Scholar]
- Effect of ritonavir on lipids and post-heparin lipase activities in normal subjects. AIDS. 2000;14:51-7.
- [Google Scholar]
- Atherogenic dyslipidemia in HIV-infected individuals treated with protease inhibitors. The Swiss HIV cohort study. Circulation. 1999;100:700-5.
- [Google Scholar]
- Diagnosis and treatment of lipodystrophy: a step-by-step approach. J Endocrinol Invest. 2019;42:61-73.
- [Google Scholar]
- Lipodissolve for body sculpting: safety, effectiveness, and patient satisfaction. J Clin Aesthet Dermatol. 2012;5:16-9.
- [Google Scholar]
- The use of deoxycholic acid for the clinical reduction of excess submental fat in Indian patients. J Drugs Dermatol. 2019;18:266-72.
- [Google Scholar]
- Deoxycholic acid in the submental fat reduction: A review of properties, adverse effects, and complications. J Cosmet Dermatol. 2020;19:2497-504.
- [Google Scholar]






