Translate this page into:
Laser-Assisted Vascular Malformation Resection: A Novel Surgical Approach
Address for correspondence: Dr. Atilla Adnan Eyuboglu, Department of Plastic and Reconstructive Surgery, Bahcelievler Memorial Hospital, Altinbas University, Bahcelievler Mah. Adnan Kahveci Bulvari No: 227, 34188 Bahcelievler, Istanbul, Turkey. E-mail: atillaeyuboglu@yahoo.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Vascular malformations can be treated using sclerotherapy agents like alcohol, polidocanol, or sodium tetradecyl sulfate foam and embolization treatments. These endovascular treatments may cause severe complications as pulmonary embolism and thrombosis. 980-nm diode lasers (DLs) are common devices used by many specialties as plastic surgeons, dermatologists, and vascular surgeons. Laser energy is excellently absorbed in water and hemoglobin, which makes it ideal for adipose tissue and deep lesions. We treated our patient using a DL. Our surgical approach allowed total excision of the arteriovenous malformation (AVM), which decreased the size of the tumor allowing a smaller incision and eased the dissection plane. We believe that lasers will be used more frequently on AVM treatments.
Keywords
Arteriovenous malformation
diode laser
laser treatment
vascular tumor
Vascular malformations (VM) are present at birth and became apparent with aging. They can be classified according to their flow pattern as high or low and structures involved as venous, arteriovenous, capillaries, and lymphatic malformations.[1] Most VM have benign nature but they may bleed or cause serious pain. They became life threatening if located on vital organs or cause compartment syndromes on hand or feet.[2]
VM can be treated using sclerotherapy agents like alcohol, polidocanol, or sodium tetradecyl sulfate foam, and embolization treatments can be performed using coils, plug, and glue which were reported to be effective.[3] These endovascular treatments may cause severe complications as transitory pulmonary hypertension, pulmonary embolism, deep venous thrombosis, and nerve and deep tissue damage.[2] These complications force surgeons for other treatment options.
A 10-year-old boy consulted with continuous pain and pulsation on left foot applied to our clinic [Figure 1]. Magnetic resonance imaging (MRI) showed that a tumor was located between first and second metatarsal bone reaching on the plantar region (see Video, Supplemental Digital Content 1, which shows the MRI of the tumor from transversal plane). Three-dimensional image was created for clarifying the margins of the tumor (see Video, Supplemental Digital Content 2, the 3D video image of the tumor on MRI). Angiography examination of the tumor identified this lesion as an AVM (see Video, Supplemental Digital Content 3, which shows the angiography of the tumor). It was prepared for embolization aiming to reduce the size of the tumor and avoid surgery. Embolization was not successful due to the small calibration of dorsal plantar branch, and it was ceased for avoiding further vessel damage.

- Preoperative image of the lesion on the medial aspect of left foot
Total excision of the lesion was planned using a diode laser (DL) to reduce the size of the AVM lesion and decrease the chance of bleeding. Operation was performed under complete anesthesia without leg tourniquet for better tumor identification. Tumescent solution using 1/10 diluted adrenalin (0.5 mg/1 mL) was injected intralesionally to avoid thermal damage of DL on surrounding tissues and for hemostasis. 980-nm Velas® DL was prepared on 15W on lipolysis mode without using its metal cannula over fiber optic cable, which gave us ability to manipulate into deeper AVM tissue avoiding further bleeding [Figure 2]. Laser was applied inside the tumor to reduce its size, which made it easier to be removed (see Video, Supplemental Digital Content 4, method of intraoperative laser application). Dissection ceased for tissue cooling as recommended in the literature.[4] 4450 joule energy was used and the operation ended with total excision of the AVM without any complications.
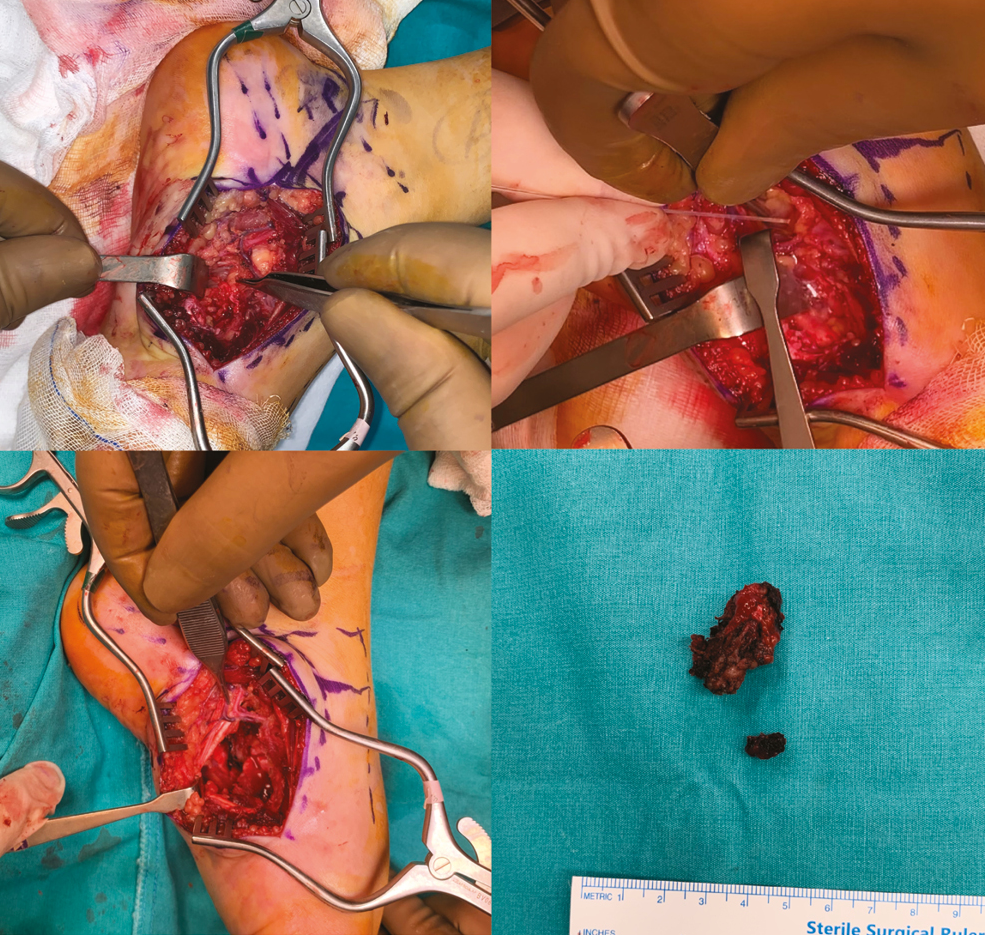
- Arteriovenous malformation excision. (A) Tumor identification, (B) diode laser application, (C) excision of the tumor, (D) Tumoral tissue after excision
The effects of lasers and intense pulse light sources are based on the principle of selective photothermolysis, which causes elective vascular injury with coagulation, vessel wall necrosis, and perivascular collagen damage. The theory of selective photothermolysis states that a specific chromophore (hemoglobin in the case of vascular lesions) can be selectively targeted.[5]
Absorption of laser energy is affected by the level of oxygen in red blood cells. Oxyhaemoglobin contained in red blood cells has a maximum peak of absorption around 540 nm (alpha peak) and 580 nm (beta peak). This holds true of small superficial vessels mainly on face. Vessels on the legs are usually located deeper and contain more deoxyhemoglobin. This situation moves the absorption curve from 800 to 1200 nm.[56]
Studies shown that intralesional laser treatments using 1470 nm DL were effective for diffuse VM correction.[4] There is not an restriction for dosing and timing on recent literature.[234] It was reported that DL usage is a minimally invasive procedure, which has less complication rates than other treatment options and should be considered as first-line treatment.[4]
980-nm DLs are common devices used by many surgeons for lipolysis. 980-nm DL is excellently absorbed in water and hemoglobin, which makes it ideal for adipose tissue and deep lesions.[25] Versatility of DLs led us usage of it on an arteriovenous malformation (AVM) treatment.
Our surgical approach allowed total excision of the AVM without further bleeding, which is a limiting factor for AVM treatments leading to incomplete resection, failure, and further complications.[2] In this study, a cheek cavernous hemangioma presenting a chronic acenocoumarol medication and high blood pressure was treated using diode 810 nm laser in the dental office completely without any complications. Protocol complied DL, with specific fiber tip, specific power, and operation mode, for 1 min/1 cm2 irradiated area.[7] Another study by Sivolella et al. showed that multiple sessions of DL application can be a safe, effective, and minimally invasive treatment for oral mucosa VM, even if characterized by high flow.[8] These various studies support the usage of laser in vascular lesion treatments as a supportive option.
Priorly done radiologic examinations helped us to detect the margins of the tumor clearly thus decreased the unnecessary incisions which could have increased the healing period. Direct application of laser decreased the size of the tumor allowing an easier dissection from surrounding healthy tissues. After total excision of the tumor, the patient had a chance of early mobilization and had a shorter recovery time plane, which leads to a better healing scar [Figure 3]. In this study, a patient was treated under local anesthesia, with a 1.5-month interval in four sessions using DL. The resting period between sessions played an important part in treatment by allowing a time for the recovery of the patient and the shrinking of the lesion which showed that the treatment can be repeated which resulted in no complications during 2.5-year follow-up.[9]

- Postoperative second year image after laser treatment assisted excision
Downside of this method was that the DL changed the histopathologic properties of the tumor by thermal effects, but it can be diagnosed by an experienced pathologist. Surgeons should check the surrounding vital structures from thermal injury in the application period. Cold application, meticulous water application, and aspiration are important.[5]
In literature, a retrospective study showed that laser-assisted aesthetic treatment of vascular lesions can be considered effective regardless of the wavelength used (Er,Cr:YSGG, CO2, Nd:YAG, and DLs), and there was no significant difference in patient and practitioner satisfaction with esthetic outcome at 6 months follow-up time.[10] These ideas lead us to use DLs as they are cheap and practically found in any hospitals. In conclusion, using laser energy on vascular lesions is promising as they decrease the chance of complications and increases the quality of wound healing. We believe that DL will used more frequently on AVM and other vascular tumor treatments.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
All videos available online www.jcasonline.com
Acknowledgement
Surgery was performed in Bahcelievler Memorial Hospital.
REFERENCES
- Vascular lesions of the head and neck: An update on classification and imaging review. Insights Imag. 2020;011:19.
- [Google Scholar]
- Diode endovascular laser treatment in venous malformations of the upper aerodigestive tract. J Craniomaxillofac Surg. 2016;44:533-7.
- [Google Scholar]
- Percutaneous treatment of low flow vascular malformations. J Vasc Interv Radiol. 2004;15:431-45.
- [Google Scholar]
- Effectiveness and safety of 1470-nm diode laser fulguration in the management of diffuse venous malformations. J Vasc Surg Venous Lymphat Disord. 2020;8:423-434.
- [Google Scholar]
- Vascular lasers and IPLS: Guidelines for care from the European society for laser dermatology (ESLD) J Cosmet Laser Ther. 2007;9:113-24.
- [Google Scholar]
- Specific absorption spectra of hemoglobin at different PO2 levels: Potential noninvasive method to detect PO2 in tissues. J Biomed Opt. 2012;17:125002.
- [Google Scholar]
- Diode laser management of cheek cavernous hemangioma in dental office. J Craniofac Surg. 2022;33:e470-e472.
- [Google Scholar]
- Diode laser for the treatment of a high flow lip vascular malformation. Minerva Dent Oral Sci. 2022;71:248-53.
- [Google Scholar]
- Management of an extensive vascular lesion on the lip by photocoagulation with high-intensity diode laser. Open Dent J. 2017;11:242-6.
- [Google Scholar]
- Aesthetic treatment outcomes of capillary hemangioma, venous lake, and venous malformation of the lip using different surgical procedures and laser wavelengths (Nd:YAG, Er,Cr:YSGG, CO2, and diode 980 nm) Int J Environ Res Public Health. 2020;17:8665.
- [Google Scholar]






