Translate this page into:
Efficacy of Fractional Carbon Dioxide Laser versus Fractional Carbon Dioxide Laser with Platelet-Rich Plasma in Treatment of Striae Distensae in a Tertiary Care Center: A Comparative Study
Address for correspondence: Dr. Hemalatha Mullagura Naidu, Department of Dermatology, Mandya Institute of Medical Sciences (MIMS), Nehrunagar, Mandya 571401, Karnataka, India. E-mail: Hemanaidu21@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Striae distensae are atrophic scars that are often cosmetically distressing. The efficacy of fractional carbon dioxide (CO2) laser and platelet-rich plasma (PRP) in treating striae individually has been evaluated previously. However, not many studies described the combined efficacy of both.
Aims and Objectives:
The aim of this study was to compare the efficacy and safety of fractional CO2 laser alone and in combination with PRP.
Materials and Methods:
Twenty-four patients with striae presenting bilaterally in the abdomen, upper limbs, and lower limbs were included. PRP was prepared by double-spin method and cell count was done to ensure at least fourfold concentration of platelets. The patients were treated CO2 laser on both sides and PRP on the left side along with laser, every month for three sessions. Digital photography and dermoscopy were done at baseline, every treatment session, and 6 months after treatment. Clinical improvement was assessed by comparing photographs and patient satisfaction before and after treatment.
Results:
All patients showed improvement on both sides. In CO2-laser-treated patients, responses in 6 patients (25%) were moderate, 14 (56%) were good, and 4 (16.6%) were excellent. In CO2-laser and PRP-treated patients, responses in 5 patients (20.8%) were moderate, 11 (45.8%) were good, and 8 (33.3%) were excellent. Hyperpigmentation was the most common side-effect seen (19 patients) on both sides, which resolved spontaneously by 6 months.
Conclusion:
These results support the use of ablative CO2 fractional laser as effective and safe treatment modalities for striae. However, slightly better efficacy was noted with the addition of PRP.
Keywords
Laser
platelet-rich plasma
striae
Ablative fractional CO2 laser is an effective method of treatment for reducing striae, having satisfactory results, and its combined use with platelet-rich plasma increases its effectiveness

INTRODUCTION
Striae distensae (SD, stretch marks) are atrophic dermal scars caused due to rapid mechanical stretching of the skin.[1] They are of two types: striae rubra (initial stage) and striae alba (evolved late-stage) and are usually associated with a pubertal growth spurt, obesity, and pregnancy. However, some pathological conditions such as Marfan’s syndrome, Cushing’s syndrome, and exogenous steroids are known to be associated with it.[23] The incidence of striae ranges from 5% to 35% in the general population and 50% to 90% in pregnancy (striae gravidarum).[34] Although striae do not cause any significant medical problems, many people seek treatment as they are of cosmetic concern.
Treatment options for SD are diverse with no gold standard therapy and inconsistent improvements, making its treatment very challenging. Recently, the fractional carbon dioxide (CO2) laser and platelet-rich plasma (PRP) gained importance in the treatment of SD.[567] However, their efficacy when combined has not been explored.
Therefore, this study aimed to evaluate and compare the efficacy of fractional CO2 laser alone and when combined with PRP.
MATERIALS AND METHODS
This was a prospective, comparative study conducted in the outpatient block, Department of Dermatology, after approval from the ethical committee. The study took place between March 2021 and October 2021, over 8 months. A total of 32 patients were assessed for eligibility to be included in the study, by consecutive sampling. Twenty-four patients who fulfilled the inclusion and exclusion criteria were recruited for the study.
Inclusion criteria
All the patients aged 18 to 40 years who gave informed consent and had striae present bilaterally were included in the study.
Exclusion criteria
Pregnant and lactating women.
Patients previously treated for striae in the last 6 months.
Patients with preexisting dermatological conditions in the treatment area.
Patients taking medications that affect bleeding and clotting mechanisms, corticosteroids.
Patients on topical or systemic retinoids.
History of hypertrophic scars or keloids, diseases affecting collagen, and elastic tissue
Patients with active infection, bleeding disorders, and atrophic lesions.
Patients with autoimmune diseases.
Patients with chronic debilitating disorders, chronic liver disease, anemia, and cardiac diseases.
Data collection
The patients were subjected to complete history taking and thorough cutaneous examination. Routine investigations to rule out platelet dysfunction were done in required patients. Evaluation of the striae regarding its stage, site, and skin texture was performed.
Preparation of platelet-rich plasma
Twenty milliliters of venous blood was collected from the anti-cubital vein under complete aseptic condition, into tubes with Anticoagulant Citrate Dextrose (ACD) as an anticoagulant. It was subjected to centrifugation by the double spin method. The first spin (soft spin) was done at 1000 rotations per minute (rpm) for 10 min. The separated plasma was gently aspirated and transferred to another vacutainer, which was subjected to second centrifugation (hard spin) at 3000 rpm for 10 min. The upper two-thirds of the plasma (platelet-poor plasma) was discarded, and the lower one-third of plasma was re-suspended to get the final PRP. The cell count was done, and a minimum fourfold increase in the platelet concentration was ensured. The final PRP was activated by adding calcium chloride (0.1 mL to 1 mL PRP), immediately before injection.
Treatment protocol
The striae sites in each patient were divided into right and left sides keeping the umbilicus as midline. The lesions on the right side were treated with ablative fractional CO2 laser (Futura RF 40, Derma India) and lesions on the left side were treated with ablative fractional CO2 laser and PRP. Before the laser procedure, a topical anesthetic was applied under occlusion, for 60 min. All the striae areas on the right and left sides were treated with an ablative fractional CO2 laser. The fractional CO2 laser was used in static mode, with pulse energy of 140 mJ, pulse duration of 500 µs, density 0.1–1 mm, and standard scanning mode with size 3 mm × 3 mm to 20 mm × 20 mm. The lesions on the left side will then be injected intradermally with PRP using an insulin syringe, in the SD, with 1 cm between the sites of injection. The treatment procedure is repeated once monthly for 3 months.
Assessment of the efficacy of the therapeutic procedure
Photographs were taken at baseline, 4 weeks, 8 weeks, and 12 weeks and patients were further followed up at 24 weeks. Apart from serial photographic evaluation, the patients were also assessed using a dermlite DL3N dermoscope before treatment and at 4 weeks, 8 weeks, 12 weeks, and 24 weeks. Both physicians and patients’ clinical assessments were performed. Clinical improvement was evaluated by two independent physicians by comparing photographs. The criteria for evaluations using a quartile grading scale with respect to texture and color and size were as follows: 0 = no improvement, 1 = poor (percent improvement, <25%), 2 = fair (percent improvement, 26%–50%), 3 = good (percent improvement, 51%–75%), and 4 = excellent (percent improvement, >76%). In addition, a patient satisfaction score was rated using the following scale: 0 = not satisfied, 1 = slightly satisfied, 2 = satisfied, 3 = very satisfied, and 4 = extremely satisfied.
Statistical analysis
The data collected were entered in MS Excel (Bellevue, Washington) and analyzed using Statistical Package for the Social Sciences software (SPSS) (IBM Corp., Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, New York: IBM Corp.). Data of quantitative variables are presented as mean ± standard deviation (SD) and categorical variables are presented as number and percentage. Wilcoxon signed rank test was used to see the changes from baseline to various follow-ups. Chi-square test and Fisher’s exact probability test were used to see the association between categorical variables and treatment groups as well as changes within the groups from baseline to various follow-ups. A value of P < 0.05 was considered statistically significant after assuming all the rules of statistical tests.
RESULTS
A total of 24 patients were included in the study. Among them, 66.7% (16 out of 24) were women and 33.3% (8 out of 24) were men. The age of the patients ranged from 19 to 35 years with a mean of 25.71 and an SD of 5.34 [Table 1]. The baseline parameters (age, sex, and distribution of the lesions) between the two groups were the same as it is a split-body comparative trial.
| Age group | Number of patients | % |
|---|---|---|
| ≤20 | 5 | 20.8 |
| 21–25 | 8 | 33.4 |
| 26–30 | 6 | 25.0 |
| ≥31 | 5 | 20.8 |
| Total | 24 | 100 |
Most of the study subjects were students (50%) followed by homemakers (33.3%). Thirteen patients had Fitzpatrick skin type IV (54.2%) and 11 patients (45.8%) had type III skin type. Of the 24 study subjects, 16 (66.7%) had striae rubra and 8 (33.3%) had striae alba. Pregnancy was the most common cause of striae among the subjects (45.8%), followed by puberty (37.5%), exercise (12.5%), and obesity (4.2%). The lesions had an acute onset in 17 patients (70.8%) and were progressive in 45.8% of the subjects. The duration of the lesions ranged from 4 months to 60 months, with a mean of 25.92 (SD = 16.93). The most common site of lesions was abdomen (25%), shoulders (25%) followed by thighs and buttocks (17% each), and arms and forearms (8% each).
The improvement was assessed every at 4th, 8th, 12th, and 24th week. The grades of improvement on both the sides, that is, the right side treated with fractional CO2 laser and the left side treated with fractional CO2 laser and PRP, at 4 weeks and 8 weeks were comparable, with no statistical differences [Table 2]. At 4 weeks, although 25% of the patients showed no improvement in either of the groups, 75% showed a poor response (P = 1.000). At 8 weeks, 33.3% showed a poor response, and 66.7% showed a fair response with fractional CO2 laser alone. However, 25% showed a poor response, 66.7% showed a fair response, and 8.3% showed a good response with fractional CO2 and PRP (P = 0.319). At the end of 12 weeks, 16.7% had a poor response, 33.3% had a fair response, and 50% had good improvement with fractional CO2 laser alone. However, 33.3% had fair, 50% had good improvement, and 16.7% had excellent improvement with fractional CO2 and PRP (P = 0.046). At the end of 24 weeks, 25% had a fair response, 58.3% had a good response, and 16.7% had excellent improvement with fractional CO2 laser alone. However, 16.7% had fair, 50% had good improvement, and 33.3% had excellent improvement with fractional CO2 and PRP (P = 0.389) [Graphs 1 and 2]. All the patients showed statistically significant improvement in the lesions from the baseline to 24th week on both sides (Wilcoxon signed-rank test = –4.399 and –4.371 on right and left side, respectively, with P = 0.001) [Graph 3 and Figures 1,2,3,4,5,6].
| Follow-up | Percentage of improvement | Side | Pearson chi-square (χ2), degree of freedom (df) P value |
|
|---|---|---|---|---|
| Right side treated with fractional CO2 laser (%) | Left side treated with fractional CO2 laser +PRP (%) | |||
| 4 weeks | No improvement 0% | 6(25) | 6(25) |
χ2 = 0.000 df = 1 P = 1.000 |
| Poor 1 to 25% | 18 (75) | 18 (75) | ||
| Fair 26 to 50% | 0 (0) | 0 (0) | ||
| Good 51 to 75% | 0 (0) | 0 (0) | ||
| Excellent 76 to 100% | 0 (0) | 0 (0) | ||
| 8 weeks | No improvement 0% | 0 (0) | 0 (0) |
χ2 = 2.286 df = 2 P = 0.319 |
| Poor 1 to 25% | 8(33.3) | 6(25) | ||
| Fair 26 to 50% | 16(66.7) | 16(66.7) | ||
| Good 51 to 75% | 0 (0) | 2(8.3) | ||
| Excellent 76 to 100% | 0 (0) | 0 (0) | ||
| 12 weeks | No improvement 0% | 0 (0) | 0 (0) |
χ2 = 8.000 df = 3 P = 0.046 |
| Poor 1 to 25% | 4(16.7) | 0 (0) | ||
| Fair 26 to 50% | 8(33.3) | 8(33.3) | ||
| Good 51 to 75% | 12(50.0) | 12(50) | ||
| Excellent 76 to 100% | 0 (0) | 4(16.7) | ||
| 24 weeks | No improvement 0% | 0 (0) | 0 (0) |
χ2 = 1.887 df = 2 P = 0.389 |
| Poor 1 to 25% | 0 (0) | 0 (0) | ||
| Fair 26 to 50% | 6(25) | 4(16.7) | ||
| Good 51 to 75% | 14(58.3) | 12(50) | ||
| Excellent 76 to 100% | 4 (16.7) | 8(33.3) | ||
| Wilcoxon signed rank test = –4.399 P = 0.001 |
Wilcoxon signed rank test = –4.371 P = 0.001 |
|||
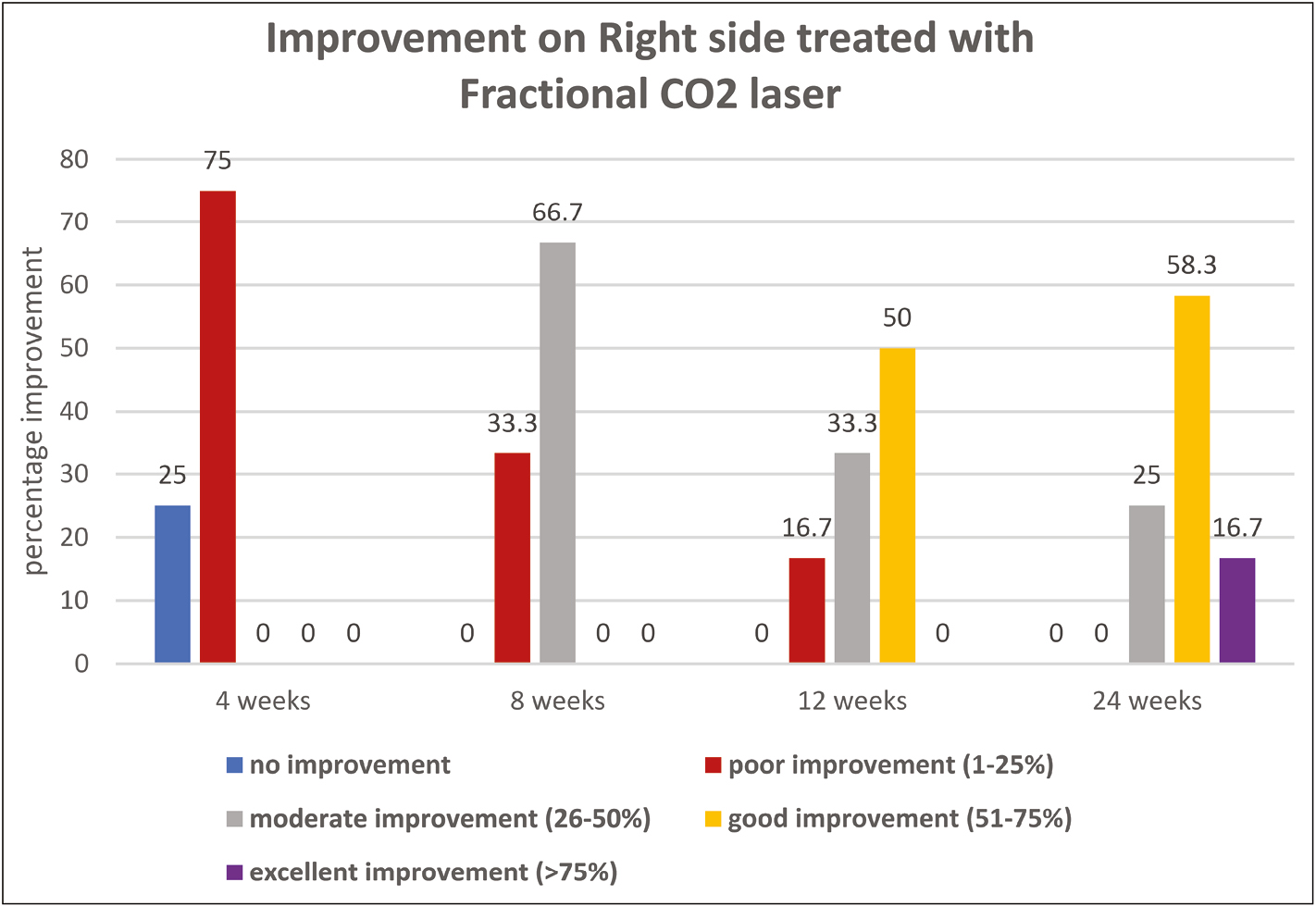
- Improvement on right side treated with fractional CO2 laser
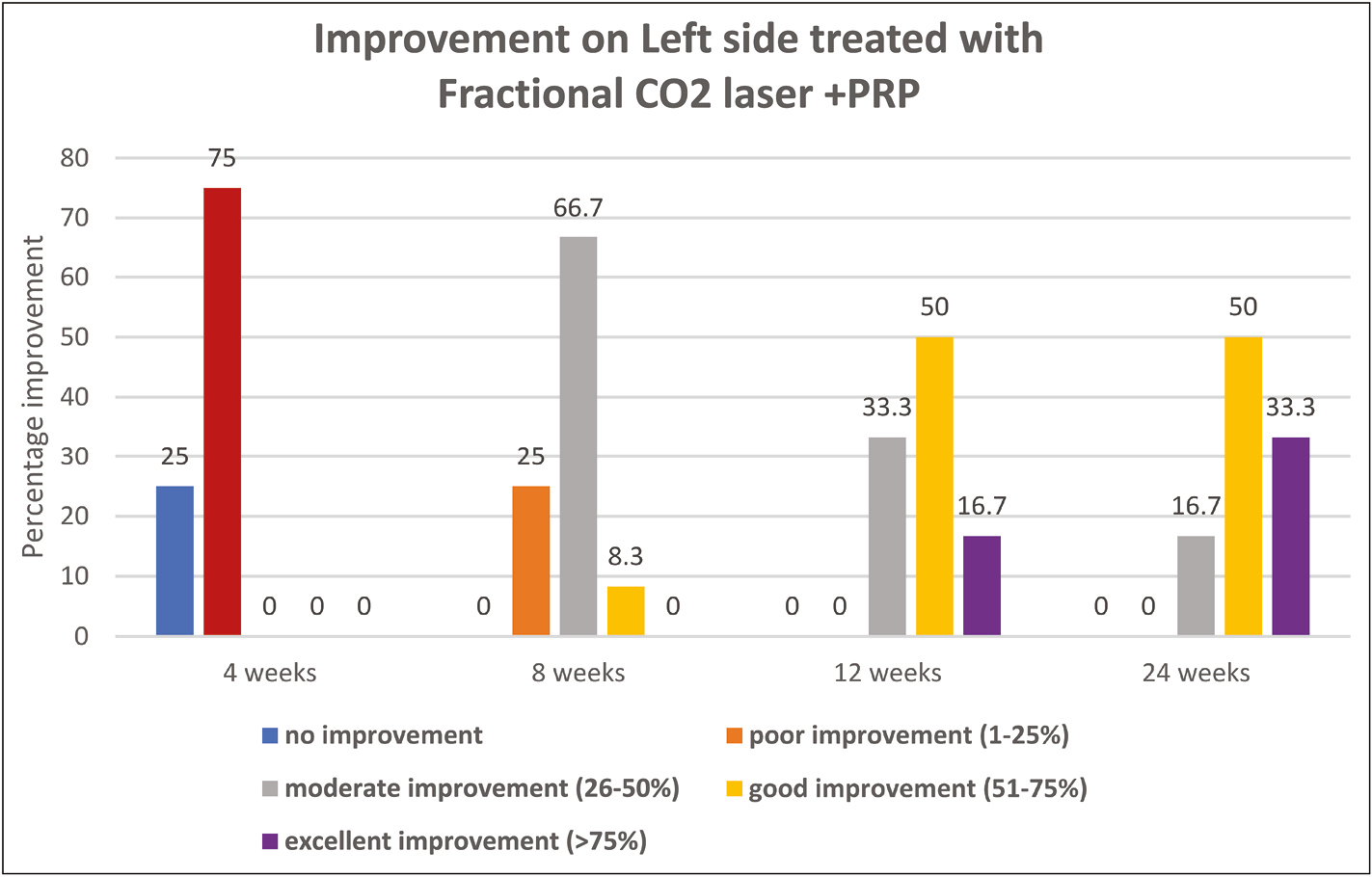
- Improvement on left side treated with fractional CO2 laser and PRP
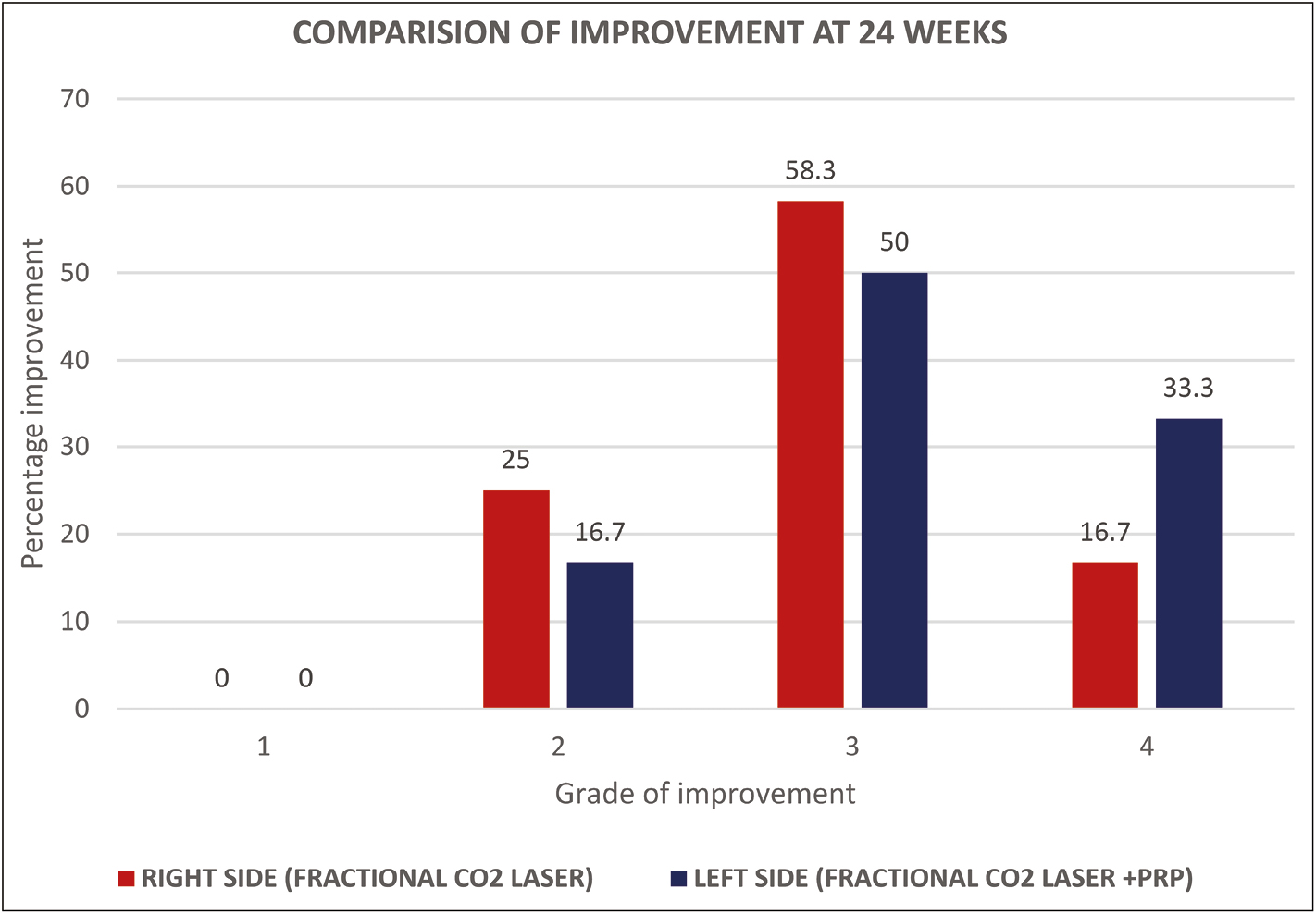
- Comparison of improvement with both the modalities at 24 weeks (final follow-up)
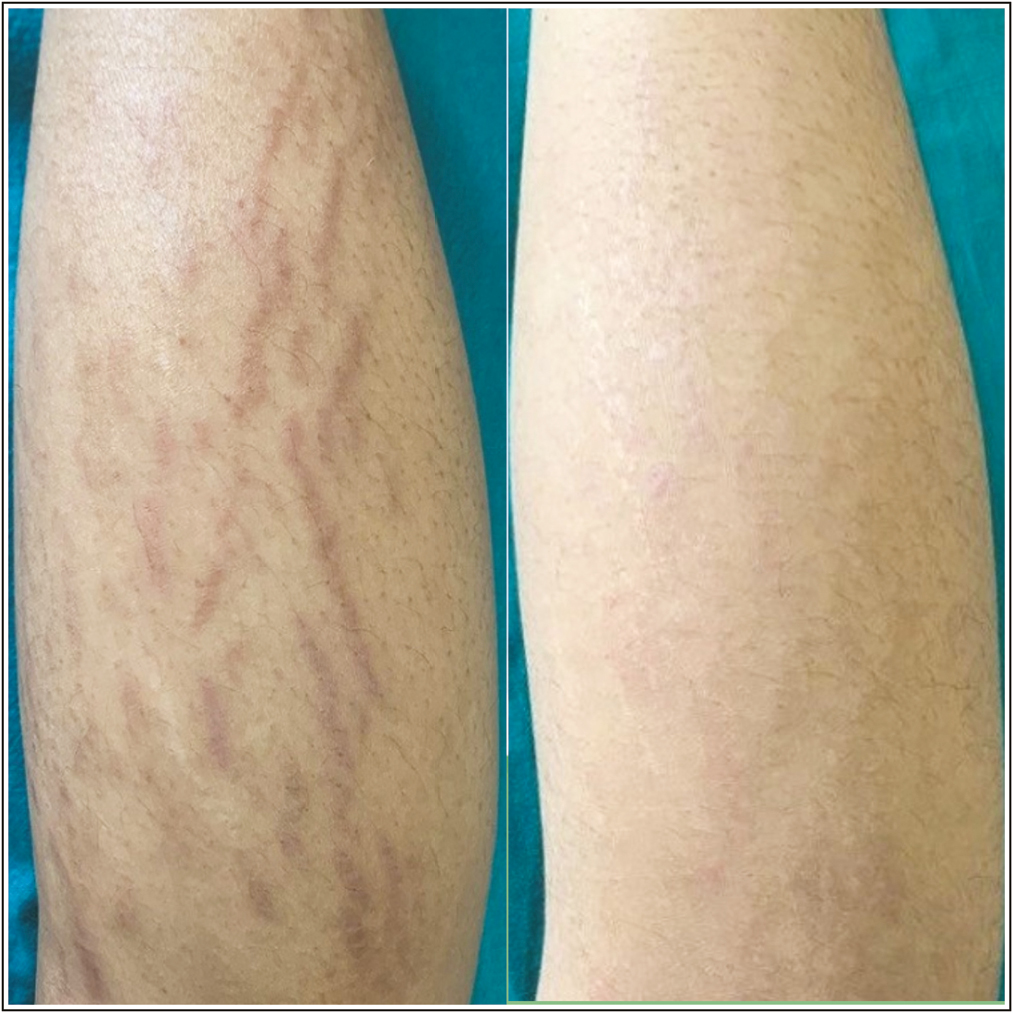
- Striae over left posterior leg: before and after treatment with fractional CO2 laser and PRP, showing grade 4 improvement
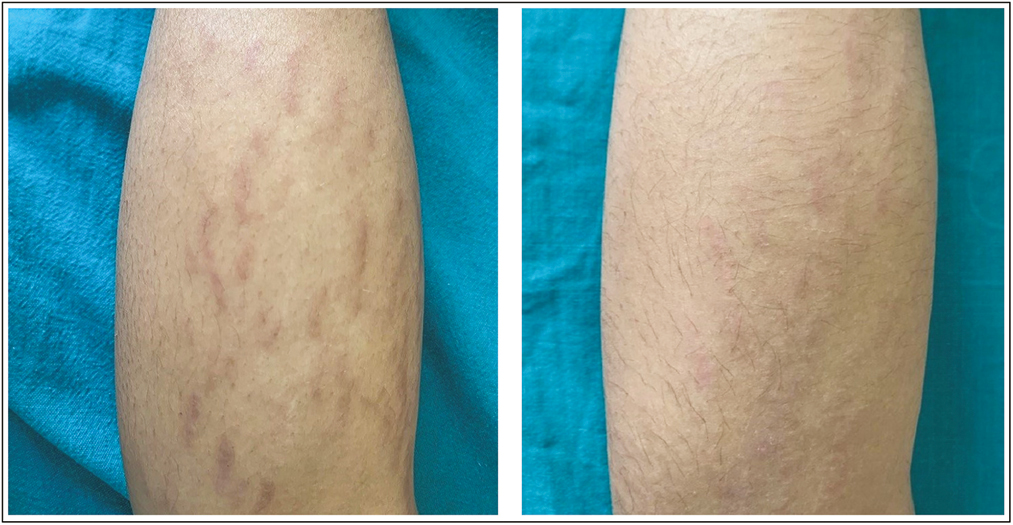
- Striae over right posterior leg: before and after treatment with fractional CO2 laser alone, showing grade 4
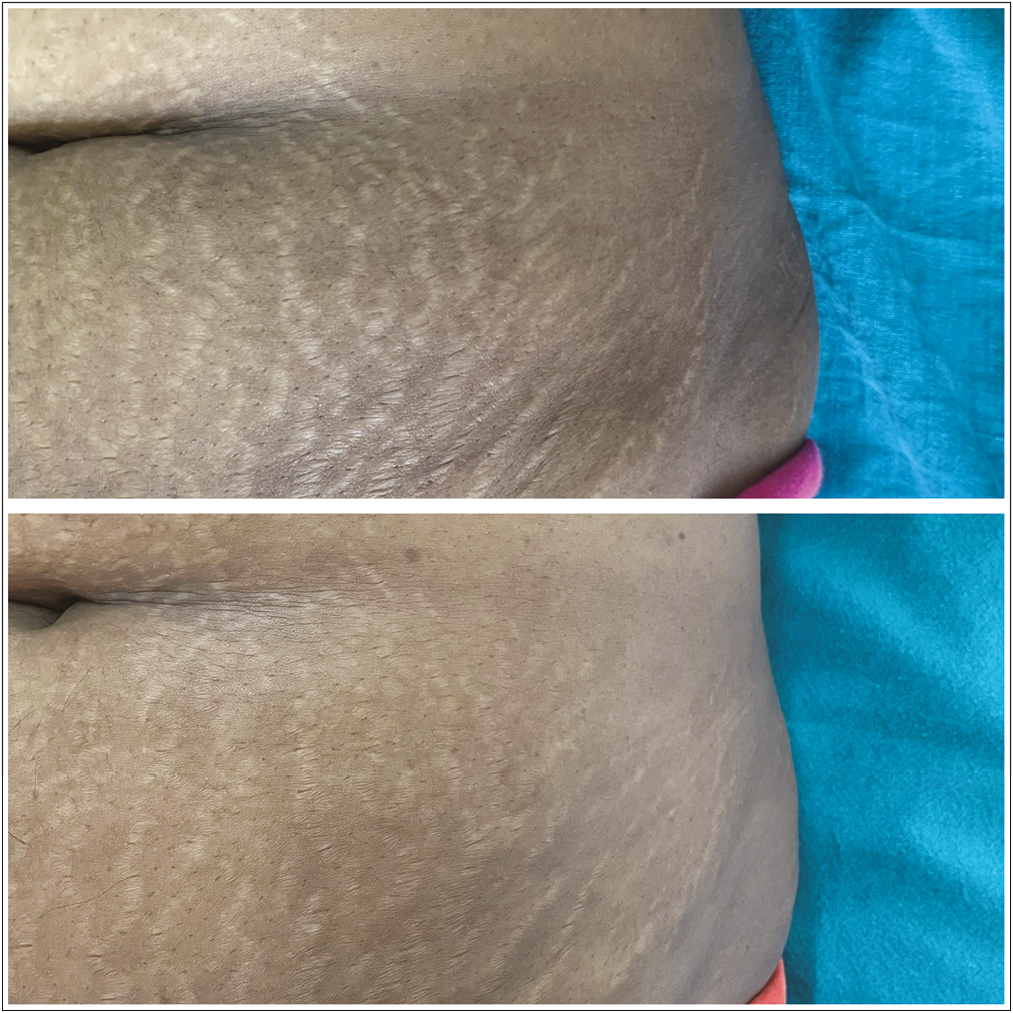
- Striae over left abdomen: before and after treatment with fractional CO2 laser and PRP, showing grade 3 improvement

- Striae over right abdomen: before and after treatment with fractional CO2 laser alone, showing grade 3 improvement

- Striae over right shoulder: before and after treatment with fractional CO2 laser and PRP, showing grade 3 improvement

- Striae over left shoulder: before and after treatment with fractional CO2 laser alone, showing grade 3 improvement
Dermoscopic evaluation was done at baseline and at the end of 24 weeks and improvement in terms of color, texture, and vascularity was noted. On the right side, 25% had a fair response, 58.3% had a good response, and 16.7% had excellent improvement; whereas 16.7% had fair, 50% had good improvement, and 33.3% had excellent improvement on the left side (P = 0.389) [Figures 7 and 8].

- Dermoscopy of striae rubra: before and after treatment with fractional CO2 laser and PRP; the resolution of linear vessels arranged both along and perpendicular to the long axis of the striae before treatment have resolved with decreased atrophy
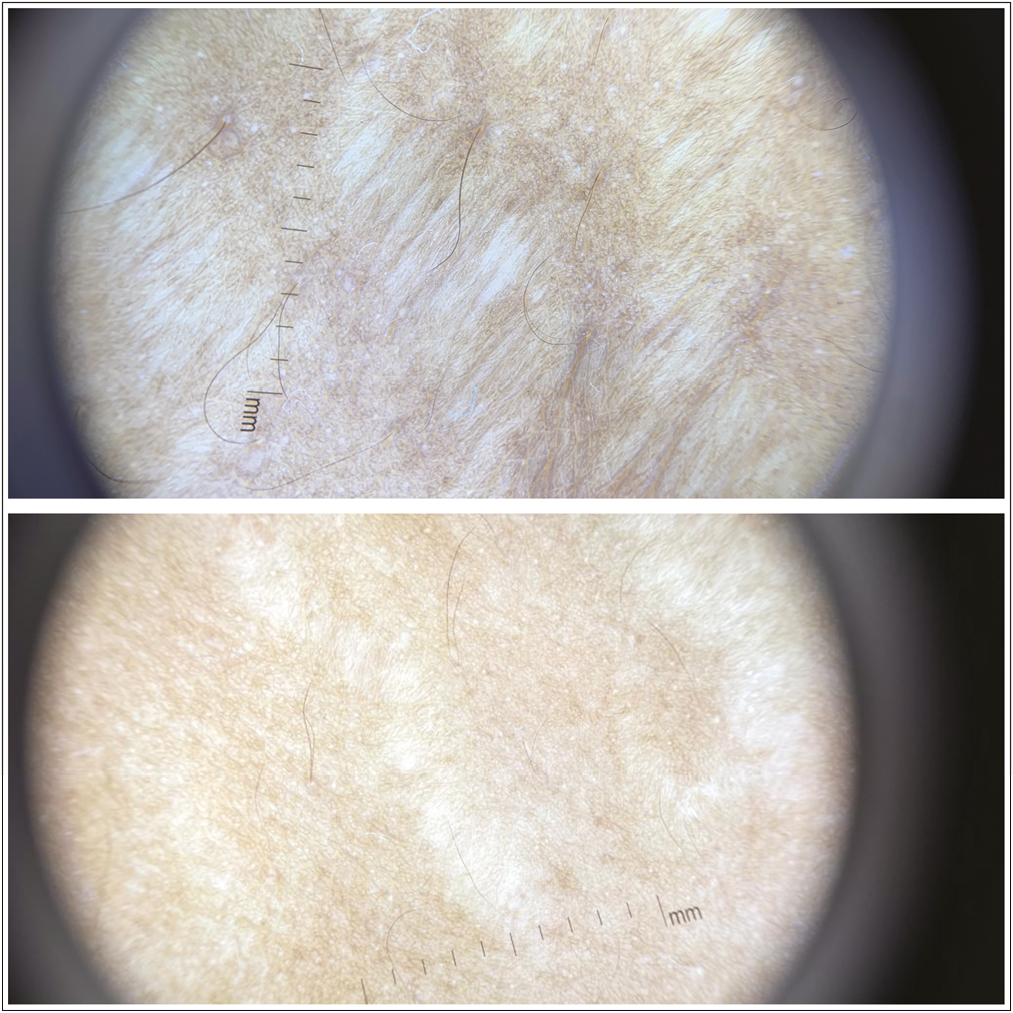
- Dermoscopy of striae alba: before and after treatment with fractional CO2 laser and PRP, showing the decrease in width, wrinkling and hypopigmentation of the striae
Patient satisfaction was evaluated at the end of 6 months. Majority of the patients were very satisfied or extremely satisfied with the improvement on both sides, with better satisfaction scores with fractional CO2 laser + PRP. (66.7% and 83.3% with fractional CO2 and fractional CO2+PRP, respectively) [Table 3].
| Patient satisfaction score | Right side (fractional CO2) | Left side (fractional CO2+PRP) | Pearson chi-square (χ2), degree of freedom (df) P value |
|---|---|---|---|
| 1 | 0% | 0% |
χ2 = 2.667 df = 2 P = 0.264 |
| 2 | 33.33% | 16.7% | |
| 3 | 50% | 50% | |
| 4 | 16.7% | 33.3% |
Hyperpigmentation was the most common side effect noted on both the sides. Eighteen patients (75%) developed hyperpigmentation with both the therapies, which resolved spontaneously or with topical depigmenting agents over 6 months. The other side effects noted include burning sensation (8% with laser and 25% with laser + PRP) and crusting (0% with laser alone and 8% with laser + PRP) [Figures 9 and 10].
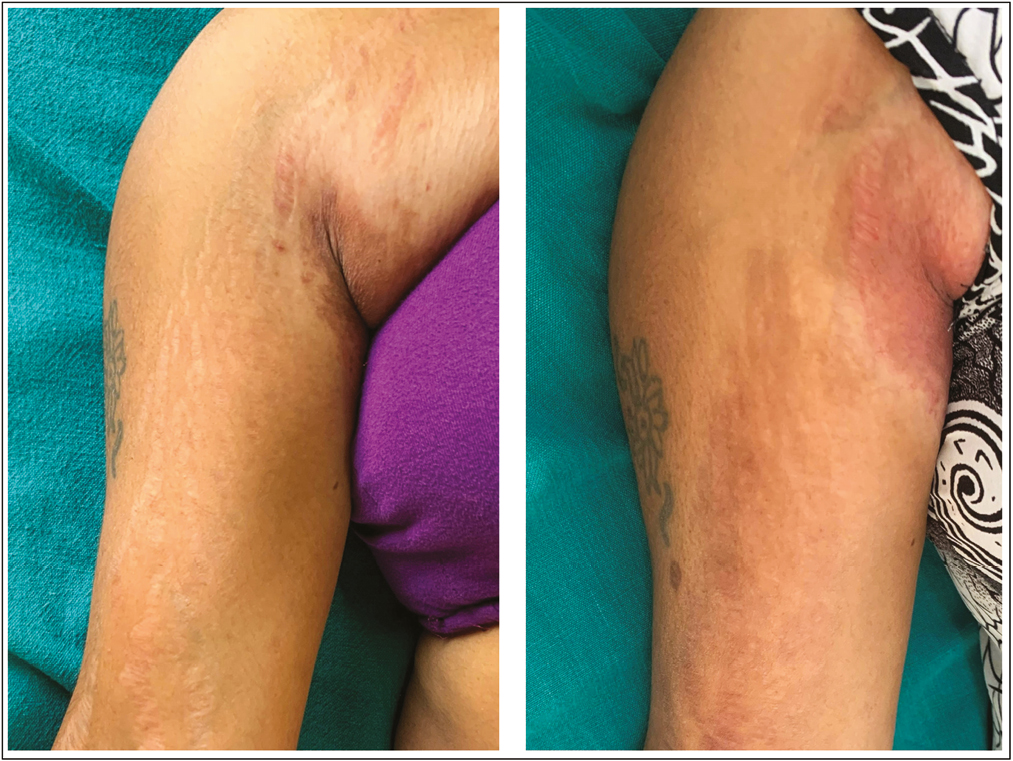
- Striae over right arm: before and after treatment with fractional CO2 laser alone, showing grade 2 improvement and hyperpigmentation
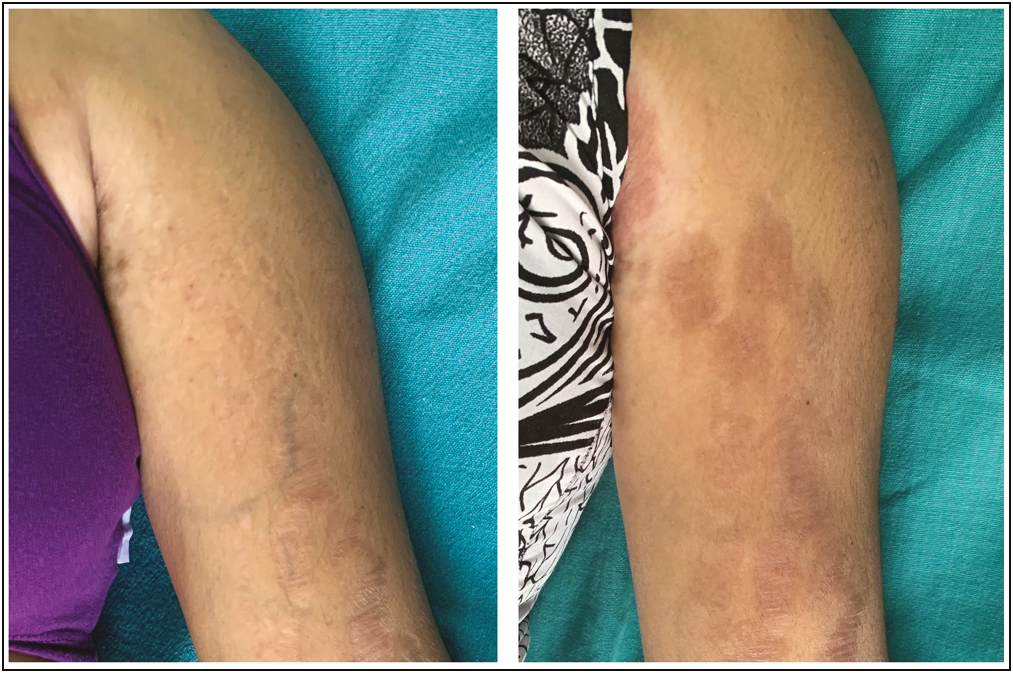
- Striae over left arm: before and after treatment with fractional CO2 laser and PRP, showing grade 2 improvement and hyperpigmentation
DISCUSSION
SD are one of the most common and cosmetically distressing conditions, commonly encountered in dermatology outpatient clinics. The lesions initially start as erythematous red, raised linear lesions (striae rubra) and later evolve into atrophic, white, wrinkled lesions (striae alba).[2] There are many causes for the striae, which can either be physiological or pathological. They include adolescent growth spurts, pregnancy, obesity, Cushing’s disease, topical or systemic steroids, and Marfan’s syndrome.[3] In our study, pregnancy was the most common cause of striae among the subjects (45.8%). Other causes such as obesity and puberty were also noted to be the causes. Similar findings were noted by Sobhi et al.,[8] who reported that 47.1% got striae due to pregnancy.
The therapeutic modalities for the treatment of SD are diverse. Various topical agents such as tretinoin, hyaluronic acid, silicone, ascorbic acid, cocoa butter, pirfenidone, olive oil, almond oil, and chemical peels such as glycolic acid and trichloroacetic acid peels have been used, with varying results. Several lasers are being used in the treatment such as fractional CO2 laser, erbium:yttrium aluminum garnet (Er:YAG) laser, diode laser, neodymium-doped yttrium aluminum garnet (Nd:YAG) laser, pulse dye laser, excimer laser, and copper bromide laser. Other modalities include light-based therapies, radiofrequency, microneedle radiofrequency, Galvano therapy, carboxytherapy, PRP therapy, and biofillers. Treating SD is challenging and though many treatment modalities are available, the results are subject to variations and there is no definite gold standard treatment.[59101112]
Recently, resurfacing of the skin using fractional CO2 laser in the treatment of SD is being ventured. When administered, this ablative laser causes micro-thermal zones (MTZ) of damage, which later becomes necrotic. The necrotic tissue is then expelled and there is stimulation of dermal collagen remodeling by the formation of new collagen. The fractional CO2 laser is also known to increase epidermal turnover. Many studies have been done which suggested that ablative fractional CO2 laser resurfacing is one of the most promising modalities of treatment of striae.[6] PRP is another treatment modality, which is being vastly explored in the treatment of SD. PRP is an autologous concentrate of human platelets in a small volume of plasma. High concentrations of growth factors and cytokines known to stimulate collagen synthesis are present in the PRP. It also has wound healing properties that reduce localized chronic inflammation, associated with striae.[79]
In our study, when treated with fractional CO2 laser alone (three sessions of therapy, 4 weeks apart), 25% had a fair response, 58.3% had a good response, and 16.7% had excellent improvement. In a study conducted by Soliman et al.,[13] when treated with fractional CO2 laser alone (three sessions of therapy, 4 weeks apart) 23.3% had no or mild improvement, 23.3% had a fair response, whereas 43.3% had a good response and 10% had excellent improvement. In a study conducted by Lee et al.,[14] 7.4% had grade excellent improvement, 51.9% had good improvement, 33.3% had moderate improvement, and 7.4% had a fair improvement. However, when treated with fractional CO2 and PRP alone (three sessions of therapy, 4 weeks apart), in our study, 16.7% had a fair, 50% had a good improvement, and 33.3% had excellent improvement. In a study conducted by Neinaa et al.,[15] 20% reported fair improvement, 56.7% reported marked improvement, and 23.3% reported excellent improvement with three treatment sessions at 6-week intervals. These results are in concordance with the results of our study. However, no studies were done to compare the efficacy of these two modalities.
In our study, in the lesions treated with fractional CO2 laser alone, 33.33% of patients were satisfied, 50% of the patients were very satisfied and 16.7% of the patients were extremely satisfied with the improvement. In the lesions treated with fractional CO2 laser and PRP, 16.7% of patients were satisfied, 50% of the patients were very satisfied and 33.33% of the patients were extremely satisfied with the improvement. In the study conducted by Soliman et al.,[13] 30.0% were not satisfied, 20.0% were somehow satisfied and 50.0% were very satisfied. Hyperpigmentation was the most common side effect noted in our study. Eighteen patients (75%) developed hyperpigmentation with both the therapies, which resolved spontaneously or with topical depigmenting agents over 6 months. In a study conducted by Sobhi et al.,[8] 52.2% of the patients developed hyperpigmentation with fractional CO2 laser. No additional side effects were noted due to PRP. However, pain was noted in more number of patients when treated with laser and PRP, when compared with laser alone. Hyperpigmentation was found to be a very common side effect in our study when compared with other studies. Our study was conducted on patients with Fitzpatrick skin type III and IV (Indian skin), which is more prone to hyperpigmentation.
In summary, fractional CO2 laser with PRP is a promising modality in the treatment of SD. However, hyperpigmentation is a major side effect that needs to be contained. Further studies with a larger sample size and longer follow-up periods are needed to ascertain the efficacy of this modality.
CONCLUSION
The results of our study support the use of ablative CO2 fractional laser as an effective and safe treatment modality for striae. However, slightly better efficacy was noted with the addition of PRP. Hyperpigmentation is the most common side effect observed, especially in Indian skin. This can be prevented by priming the patient with depigmenting agents before starting the treatment.
Financial support and sponsorship
Not applicable.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
References
- A double-blind controlled clinical trial assessing the effect of topical gels on striae distensae (stretch marks): A non-invasive imaging, morphological and immunohistochemical study. Arch Dermatol Res. 2013;305:603-17.
- [Google Scholar]
- Mast cell degranulation and elastolysis in the early stage of striae distensae. J Cutan Pathol. 1991;18:410-6.
- [Google Scholar]
- Striae distensae treatment review and update. Indian Dermatol Online J. 2019;10:380-95.
- [Google Scholar]
- Fractional CO2 laser versus intense pulsed light in treating striae distensae. Indian J Dermatol. 2016;61:174-80.
- [Google Scholar]
- Perspectives and challenges in regenerative medicine using plasma rich in growth factors. J Control Release. 2012;157:29-38.
- [Google Scholar]
- Comparative study between the efficacy of fractional micro-needle radiofrequency and fractional CO2 laser in the treatment of striae distensae. Lasers Med Sci. 2019;34:1295-304.
- [Google Scholar]
- Platelet-rich plasma (PRP): Current applications in dermatology. Skin Therapy Lett. 2019;24:1-6.
- [Google Scholar]
- Striae distensae (stretch marks) and different modalities of therapy: An update. Dermatol Surg. 2009;35:563-73.
- [Google Scholar]
- Intense pulsed light in the treatment of striae distensae. Dermatologic Surgery. 2002;28:1124-30.
- [Google Scholar]
- Therapeutic targets in the management of striae distensae: A systematic review. J Am Acad Dermatol. 2017;77:559-568.e18.
- [Google Scholar]
- Efficacy of fractional carbon dioxide laser versus microneedling in the treatment of striae distensae. J Cosmet Laser Ther. 2019;21:270-7.
- [Google Scholar]
- Treatment of striae distensae using an ablative 10,600-nm carbon dioxide fractional laser: A retrospective review of 27 participants. Dermatologic Surgery. 2010;36:1683-90.
- [Google Scholar]
- Synergistic effect of platelet-rich plasma in combination with fractional carbon dioxide laser versus its combination with pulsed dye laser in striae distensae: A comparative study. Photodermatol Photoimmunol Photomed. 2021;37:214-23.
- [Google Scholar]





