Translate this page into:
Therapeutic Plasma exchange therapy in Burns
Address for correspondence: Dr. Ravi Kumar Chittoria, Department of Plastic Surgery & Telemedicine, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry 605006, India. E-mail: drchittoria@yahoo.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Severe burn injury affects the body in many devastating ways, the most severe being systemic inflammatory response syndrome. This results in a myriad of effects like increasing capillary permeability, thereby fluid loss. It also causes a surge in inflammatory mediators like interleukin (IL)-6, which further increases the capillary leak and fluid loss. This results in refractory hypotension in patients despite adequate fluid resuscitation. Plasma exchange has been used in the management of a number of illnesses with a significant inflammatory component, and, therefore can be considered to have a role in burn injury. In our article, we would like to share our experience of using therapeutic plasma exchange therapy in burn patient
Keywords
Burn
sepsis
therapeutic plasma exchange
INTRODUCTION
Burn injury, apart from the wound itself, results in extensive fluid loss. Hence, fluid resuscitation is an important part of the burn management protocol. Although the survival rate of increased percentage burns has increased over years, fluid resuscitation seems to be inadequate in a subset of patients.[1] There has also been an increase in morbidity due to fluid overload as well.[2] The varied fluid requirements are due to a surge of inflammatory mediators due to systemic inflammatory response due to burn injury.[3] There is an increase in tumor necrosis factor-, interleukin (IL)-1, IL-6, platelet-activating factor, IL-10, complement 5, and reactive oxygen and nitrogen species.[4] Therapeutic plasma exchange (TPE) is a technique of extracorporeal blood purification that removes large-molecular-weight particles such as inflammatory mediators from the circulating blood volume.[5] We would like to share our experience of using TPE in a burn patient with sepsis and refractory hypotension.
MATERIALS AND METHODS
The study was conducted in the tertiary burn care center. The patient was a 1-year-old girl with 17% (10% superficial partial-thickness + 7% full-thickness burns) scald burns. She was immediately managed with fluid resuscitation according to Parkland’s formula and was started on a prophylactic antibiotic. Wound management was done by heterografting with collagen and RONPT every alternate day. The child developed persistent fever spikes on admission day 2. Urine routine and blood culture were sent and were found to be sterile. On admission day 5, the child was hypotensive, and the condition deteriorated. Hence, fluid bolus was given. As the child was not responding to the fluid bolus and the condition continued to deteriorate, the child was started on vasopressors (adrenaline, noradrenaline, vasopressin) and the child was intubated. Empirically started on injections Meropenam and Cloxacillin. Repeat blood culture showed Enterococcus faecalis growth and was started on injection Vancomycin. Wound culture showed Acinetobacter and pseudomonas growth, for which the child was started on minocycline. Arterial line secured in the right upper limb and central venous line in the left groin. Wound condition progressively worsened. As the child was not responding to fluid challenges and vasopressors, with persistent hypotension, the child was taken up for continuous renal replacement therapy (CRRT) and TPE. TPE was done using Gambro/Fresinus machines [Figure 1] and Fresinius Plasmaflux plasma filters (P1 = 0.3 m2, P2 = 0.6 m2). In patients requiring concurrent CRRT, CRRT was done with PrismaFlex, and Fresinius PlasmaFlux [Figure 2] with plasma filters attached to the CRRT circuit for the duration of TPE. Plasma volume was estimated with the following formula: 0.065 × weight × (1-hematocrit). 1.5 times the estimated plasma volume was exchanged with the blood flow rate started at 3–5 mL/kg/min. Exchange was completed within 4 h of starting. Two-thirds of the volume was replaced with fresh frozen plasma and one-third with albumin 5%. One cycle of TPE was done.

- Continuous renal replacement therapy machine
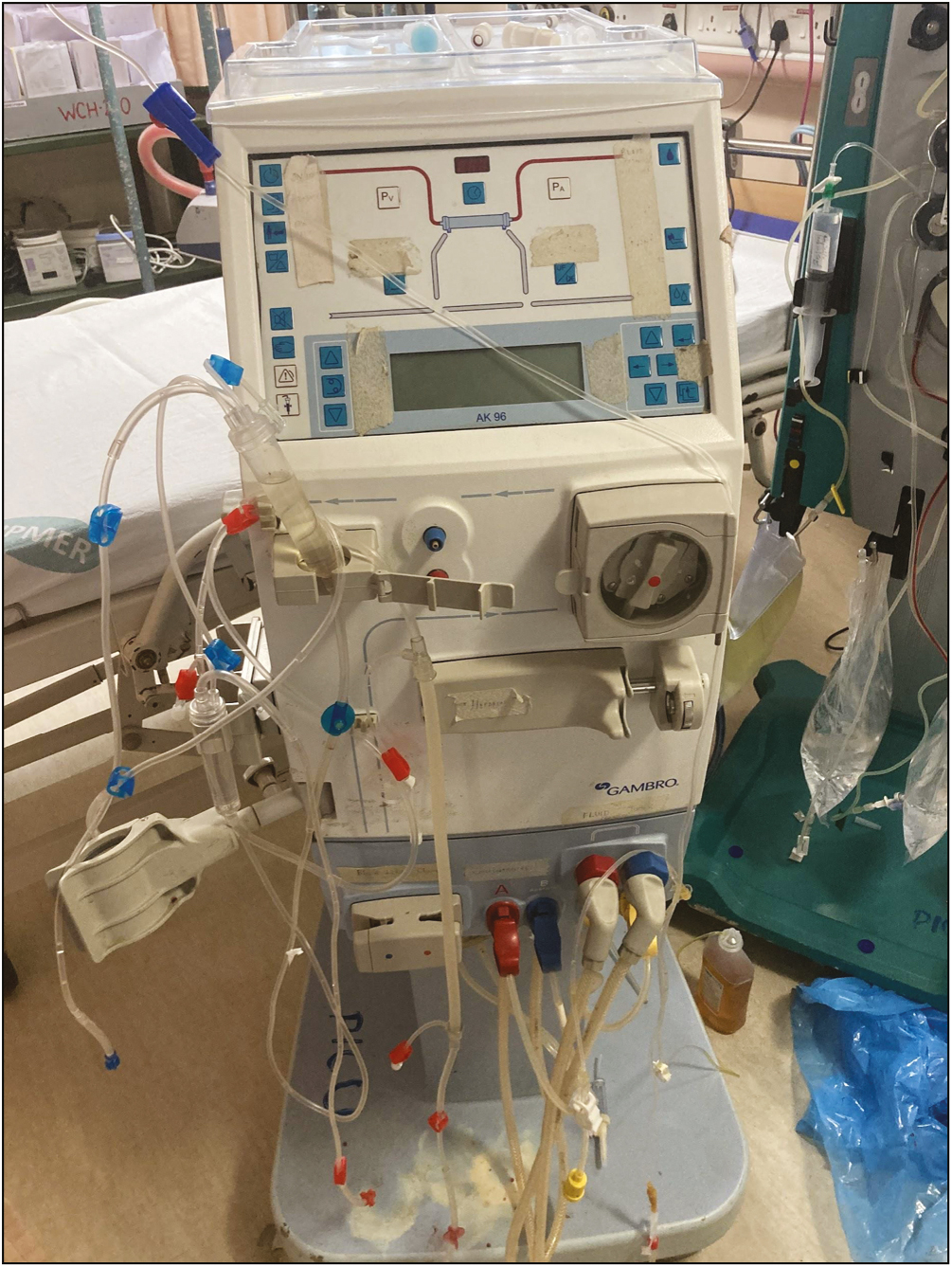
- Plasma exchange machine
Despite adequate treatment, due to overwhelming sepsis, the child succumbed to the injuries.
DISCUSSION
Despite strictly following fluid resuscitation in burns, many patients still receive massive fluid volumes but show minimal hemodynamic response. These massive fluid loads can cause severe negative effects.[6] Therefore, a procedure that can reduce the fluid requirement as well as mitigate the systemic inflammatory response in burns would help in decreasing morbidity and mortality in the burn patient. Plasma exchange has been an accepted treatment modality for various diseases with a profound immune component.[7] Gårdlund et al.[8] reported that plasma exchange significantly increased the plasma clearance of tumor necrosis factors. Stratta et al.[9] similarly reported a blunting of acute-phase mediators of sepsis after plasma exchange. Thermal injury can initiate a systemic inflammatory response that gradually leads to multiorgan dysfunction.[10] Therefore, the removal of the portion of circulating blood volume that carries these cytokines should improve burn shock. A study done by Stratta et al.[11] evaluated 22 patients with severe burn injuries. They found that the patients treated with plasma exchange were resuscitated faster and their urine output was higher compared to patients without TPE. Schnarrs et al.[12] similarly observed a decrease in fluid resuscitation requirements as well as an increase in cardiac index after plasma exchange in a small group of burn patients with severe injury. Hematocrit, base deficit, and lactate levels as surrogate markers of resuscitation status—three serum markers of resuscitation status––were monitored.[13] Complications such as cardiovascular events (0.2%), respiratory events (0.2%), and anaphylactoid reactions (0.25%), and hemorrhage and infection (0.02%) have been reported.[14]
In our patient, though TPE was done, the child had unfortunately succumbed to the injury, the cause of death being overwhelming sepsis.
The limitation of this study is the availability of the equipment and the cost (2 lakh INR) of the equipment. The other limitation is that the effectiveness of the therapy in terms of reducing immune modulators was not quantified.
CONCLUSION
TPE is an effective method in reducing fluid volume in resuscitation in burn patients as well as decreasing the cytokine and immune mediators that play a devastating effect in contributing to the mortality of these patients. But as our study is a single-center report, a multicenter randomized controlled study is required to validate the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Predicting increased fluid requirements during the resuscitation of thermally injured patients. J Trauma. 2004;56:404-13; discussion 413-4.
- [Google Scholar]
- A biopsy of the use of the Baxter formula to resuscitate burns or do we do it like Charlie did it? J Burn Care Rehabil. 2000;21:91-5.
- [Google Scholar]
- Interleukin-1 mediates thermal injury-induced lung damage through C-jun NH2-terminal kinase signaling. Crit Care Med. 2007;35:1113-22.
- [Google Scholar]
- Cytokine expression profile over time in severely burned pediatric patients. Shock. 2006;26:13-9.
- [Google Scholar]
- Therapeutic plasmapheresis by continuous flow centrifugation. N Z Med J. 1980;92:145-8.
- [Google Scholar]
- The association between fluid administration and outcome following major burn: A multicenter study. Ann Surg. 2007;245:622-8.
- [Google Scholar]
- A controlled study of double filtration plasmapheresis in the treatment of active rheumatoid arthritis. J Clin Rheumatol. 2007;13:193-8.
- [Google Scholar]
- Plasma levels of cytokines in primary septic shock in humans: Correlation with disease severity. J Infect Dis. 1995;172:296-301.
- [Google Scholar]
- Immunologic parameters in burned patients: Effect of therapeutic interventions. J Trauma. 1986;26:7-17.
- [Google Scholar]
- The 1994 Lindbergh award: The production of tumor necrosis factor, interleukin-1, interleukin-6, and prostaglandin E2 by isolated enterocytes and gut macrophages: Effect of lipopolysaccharide and thermal injury. J Burn Care Rehabil. 1994;15:470-7.
- [Google Scholar]
- Plasma exchange for failure of early resuscitation in thermal injuries. J Burn Care Rehabil. 1986;7:230-3.
- [Google Scholar]
- The beneficial effects of plasma exchange after severe burn injury. J Burn Care Res. 2009;30:243-8.
- [Google Scholar]
- Therapeutic plasma exchange: Complications and management. Am J Kidney Dis. 1994;23:817-27.
- [Google Scholar]






