Translate this page into:
Surgical Correction of a Cicatricial Lagophthalmos
Address for correspondence: Dr. André Cerejeira, Department of Dermatology and Venereology, Centro Hospitalar São João, Alameda Prof. Hernâni Monteiro, 4200–319 Porto, Portugal. E-mail: cerejeira.andre@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
The eyelids are critical in protecting the cornea from injury and in maintaining tear film integrity. Lagophthalmos is the incomplete or abnormal closure of the eyelids and can lead to corneal exposure, excessive evaporation of the tear film, and subsequent exposure keratopathy. This can progress to corneal abrasion, infection, and, in extreme cases, ocular perforation and loss of the eye.[1] Therefore, early recognition and effective treatment of this condition is paramount.
The most frequent cause of lagophthalmos is facial nerve paralysis, which leads to paralytic lagophthalmos. On the contrary, a cicatricial lagophthalmos can arise after surgery or trauma resulting in excessive scarring and retraction of the eyelid. In such cases, release of scar tissue and repositioning of the levator palpebrae superioris are critical steps for a successful treatment.[2]
An 83-year-old man presented with cicatricial lagophthalmos on the left upper eyelid, leading to eye dryness and foreign body sensation. Three years earlier, he had been subm itted to radical excision of a basal cell carcinoma of the lateral canthus of the left eye by Mohs surgery. During surgery, a full-thickness skin graft from the preauricular region was used to cover the defect, and a lateral canthoplasty was performed. However, a cicatricial lagophthalmos ensued nonetheless, leading to a corneal ulcer 7 months later.
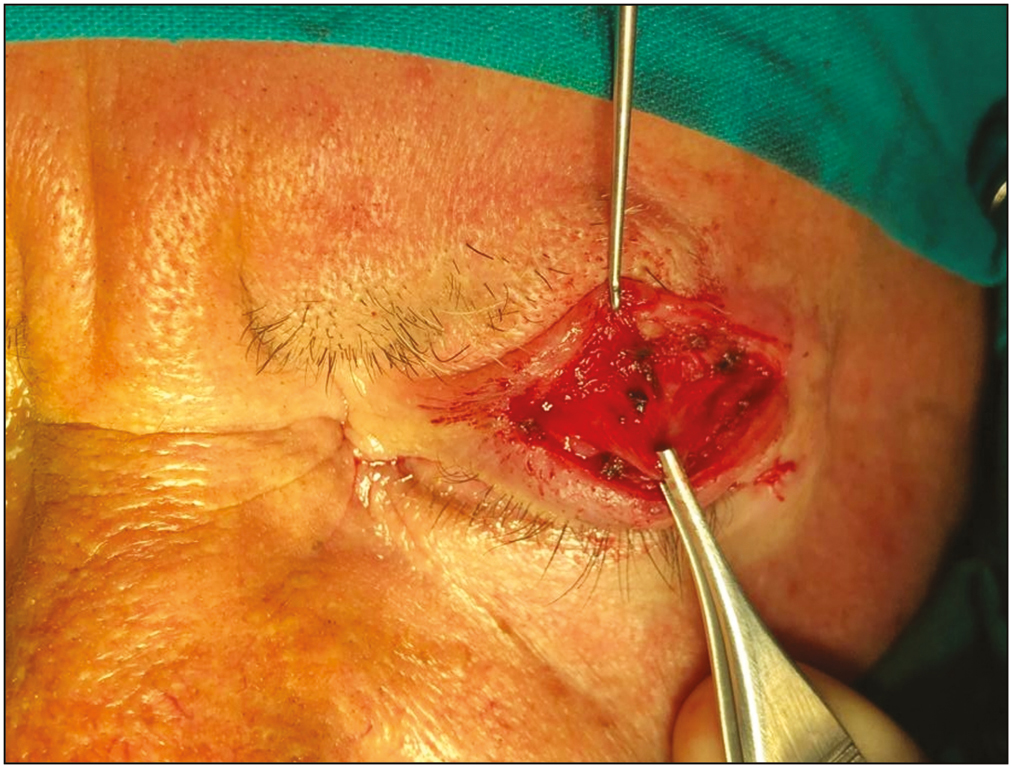
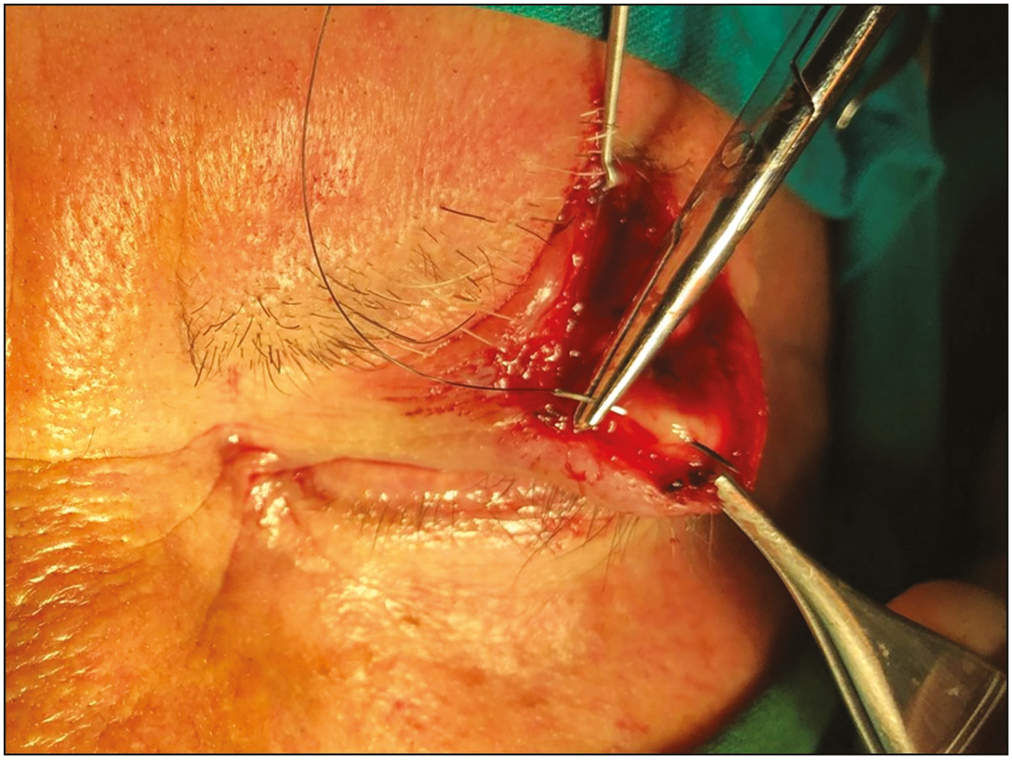
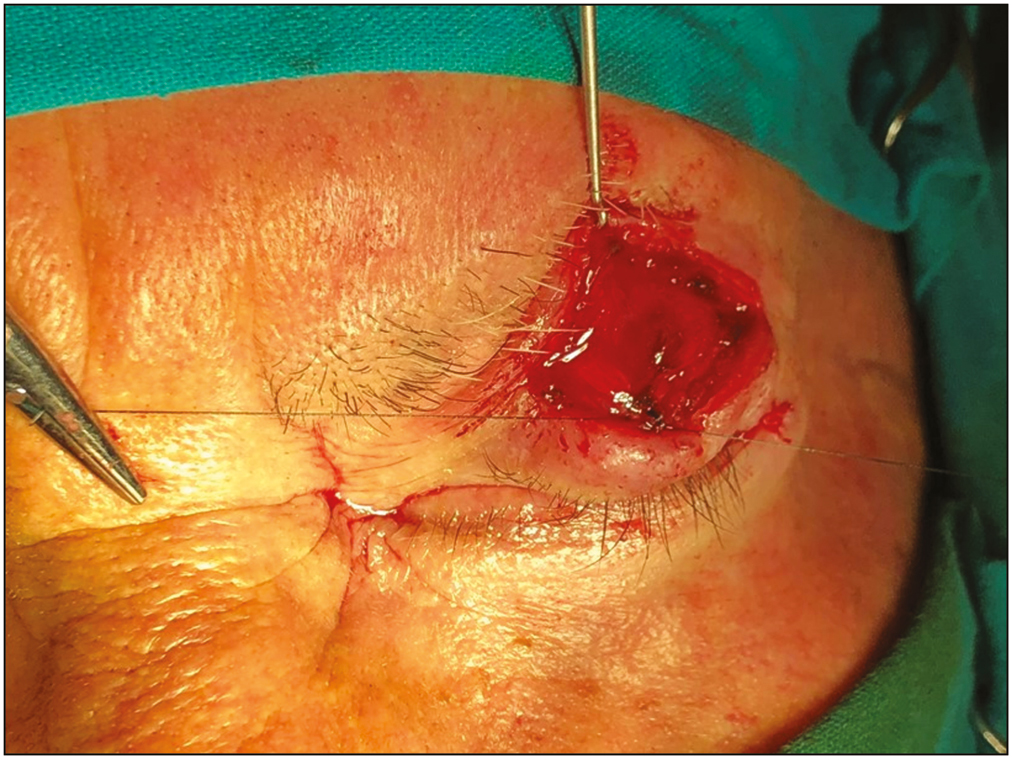
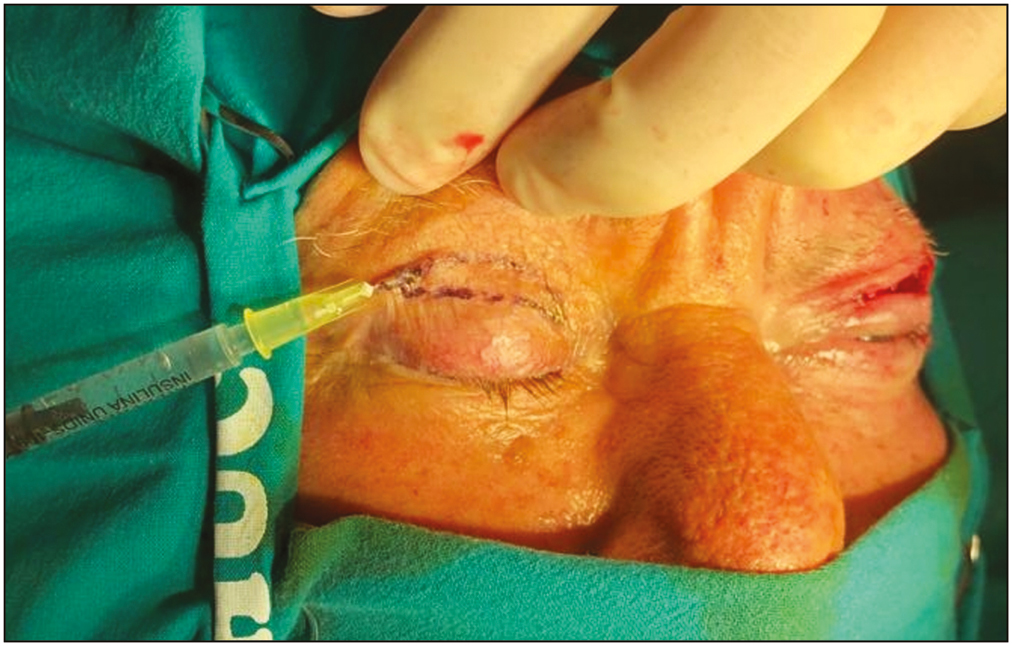
On examination, scarring and retraction could be observed in the central and lateral segments of the left upper eyelid [Figure 1]. An incision was made through the superior eyelid crease. Scar tissue was released [Figure 2] and a lateral tarsorrhaphy was performed. The aponeurosis of the levator palpebrae superioris was identified [Figure 3], repositioned, and sutured to the anterior surface of the superior tarsal plate [Figures 4 and 5]. A skin graft was harvested from the right upper eyelid [Figure 6]. The secondary defect was easily closed primarily. The graft was then adapted and sutured to the defect on the left upper eyelid. Immediately after surgery, full eyelid closure was possible. An excellent functional and cosmetic outcome was noticeable after 1 week [Figure 7] and also after 6 months [Figures 8A and B], with complete resolution of subjective symptoms.
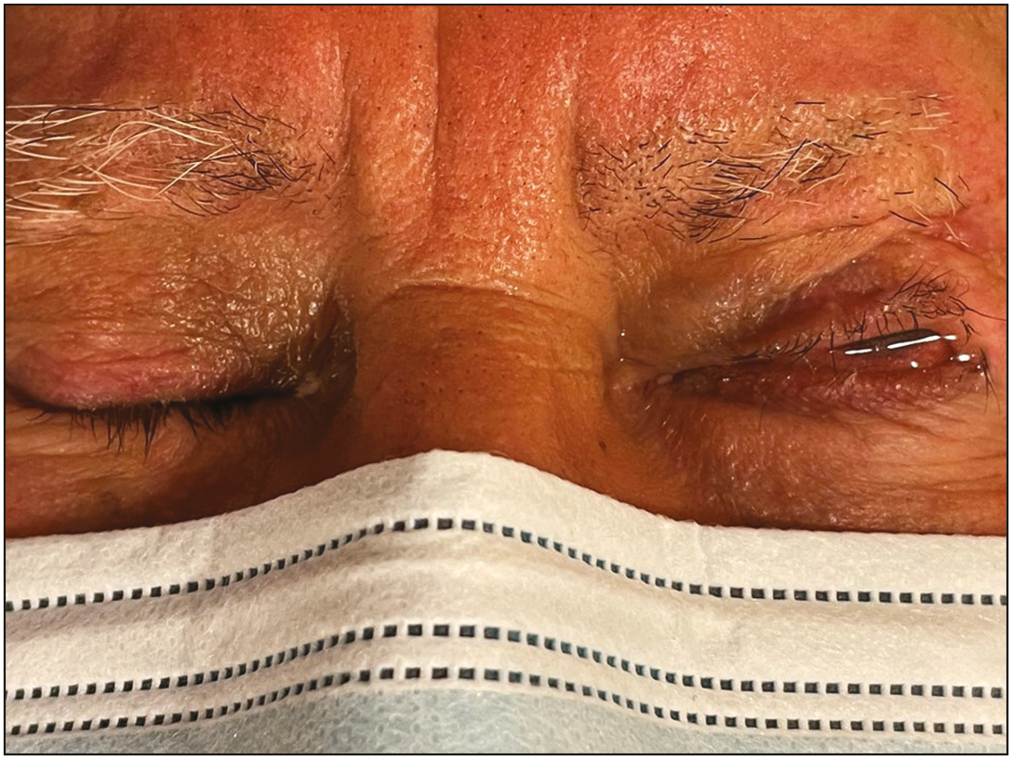
- Cicatricial lagophthalmos on the left upper eyelid

- Incision through the superior eyelid crease. Scar tissue was released
- Aponeurosis of the levator palpebrae superioris was identified
- Aponeurosis of the levator palpebrae superioris was repositioned and sutured to the anterior surface of the superior tarsal plate
- Aponeurosis of the levator palpebrae superioris in its new position
- A skin graft was harvested from the right upper eyelid

- One week after surgery, an excellent functional and cosmetic outcome was noticeable
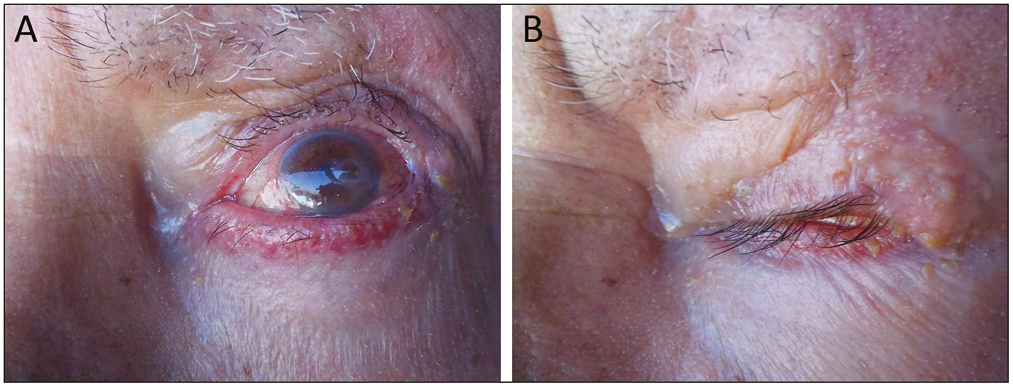
- (A) Six months after surgery, an excellent functional and cosmetic outcome was noticeable (eyes open). (B) Six months after surgery, an excellent functional and cosmetic outcome was noticeable (eyes closed)
The management of cicatricial lagophthalmos involves both medical and surgical approaches. The aim of medical treatment is to improve tear film stability. Artificial tears without preservatives should be administered frequently. Ointments, moist chambers, physiotherapy, and overnight taping of the eyelid can also be beneficial.[3]
In severe or permanent cases, surgical treatment is typically required.[4] The objective is to prevent exposure keratitis and reestablish eyelid function. The preferred procedure will depend on the location, severity, and etiology of lagophthalmos, as well as patient factors (including age, comorbidities, and expectations) and surgeon experience. Critical steps include (1) complete excision or release of the contracted scar tissue, (2) a method to prevent readhesions, and (3) reconstruction of the skin defect.[1]
Several reconstruction techniques have been reported, including local flaps and skin grafts. The upper eyelid should be soft and flexible to allow natural and effortless blinking. If a severe contracture is present, local flaps can leave large unsightly scars and may not achieve adequate scar release.[2] The technique described achieved favorable functional and cosmetic outcomes in this patient.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Not applicable.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Early cicatricial lagophthalmos release with pentagonal wedge resection of the scar, fat redistribution, and full-thickness skin grafting. Arch Craniofac Surg. 2020;21:49-52.
- [Google Scholar]
- Lagophthalmos or hare eye: An etymologic eye opener. Aesthetic Plast Surg. 2008;32:573-4.
- [Google Scholar]





