Translate this page into:
Comparative evaluation of therapeutic efficacy and safety of black peel versus 25% trichloroacetic acid peel in mild to moderate acne vulgaris: a split face study
Address for correspondence: Dr. Neerja Puri, Department of Dermatology, GGS Medical College, Faridkot, Punjab, India. E-mail: neerjaashu@rediffmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Introduction:
Peeling has withstood the test of time as a simple, minimally invasive method to renew the skin, despite the introduction of more advanced procedures like lasers.
Materials and Methods:
Thirty patients (or 60 sites) with age ranging from 15 to 45 years with mild-to-moderate acne vulgaris were included in the study. Assessment at baseline was done by the global acne grading system score for including mild and moderate acne patients.
Results:
On grading the improvement according to the 5-point Global Assessment Scale (GAS), it was found that in area A (black peel), 6.7% of patients showed excellent improvement, 86.7% of patients showed good improvement, and 6.7% of patients showed fair improvement. In area B (25%TCA peel), 6.7% of patients showed excellent improvement, 80% of patients showed good improvement, and 13.3% of patients showed fair improvement.
Discussion:
None of the patients showed poor or worse outcomes in any of the areas. The difference between the groups was not significant (P = 0.688).
Conclusion:
There is a paucity of data in the literature regarding the comparison of black peel with other conventional peels in the treatment of acne vulgaris. To the best of our knowledge, this is the first study comparing black peel with TCA peel in the treatment of acne vulgaris.
Keywords
Acne
black
peel
pigmentation
TCA
INTRODUCTION
Acne vulgaris is a chronic, inflammatory illness of the pilosebaceous unit that typically manifests in adolescence as pleomorphic lesions such as comedones, papules, pustules, nodules, and cysts. Acne is a prevalent condition that affects up to 80% of persons between the ages of 11 and 30 and up to 5% of adults beyond the age of 30.[1] The disease occurs in all races worldwide affecting 90% of people at some time in their life.[2] Few racial differences are known. The Japanese population is said to be affected less than Americans and cystic acne is more common in whites.[34] All body regions with high concentrations of pilosebaceous glands are affected, although the face, back, and chest are affected the most. The severity of post-inflammatory hyperpigmentation caused by inflammatory acne lesions depends on how early the acne patients are treated, baseline skin type, history of post-inflammatory hyperpigmentation, sun exposure, adherence to sun protective practices, other medical conditions the patient is suffering from and any concomitant medication intake by the patient. Acne-related severe hyperpigmentation and scarring are associated with significant physical and psychological suffering, especially in teens.
An aberrant desquamation of keratinocytes lining the sebaceous follicle is the earliest step in the development of an acne lesion, and an increase in circulating androgens at the onset of puberty increases the production of sebum in the pilosebaceous unit. These events create a favorable environment for the colonization of commensal bacteria within the pilosebaceous unit. Propionibacterium acnes secretes various inflammatory molecules and chemotactic factors that initiate and perpetuate the local inflammatory response and possibly induce keratinocyte proliferation.[5]
Chemical peeling is a common office procedure that has evolved over time, using the scientific understanding of wound healing after controlled chemical skin injury.[6] It is a type of targeted cutaneous ablation employing chemical agents that permits quick, predictable, and uniform thickness of chemoablation to a chosen skin depth, resulting in an improvement in the skin’s appearance. The application of a chemical solution to the skin makes it to separate, peel off, and regenerate new skin. The new skin is less wrinkled and more supple than the old skin.
Numerous therapy modalities, including topical and systemic anti-bacterial, retinoids, and sebostatics, have been used to treat acne, and now, physicians attempt to apply novel technologies in acne care, such as chemical peeling. Numerous practitioners have used chemical peels for the treatment of acne vulgaris since it is a noninvasive and safe method. It is a suitable choice for patients who cannot tolerate typical oral acne medicines.
Trichloroacetic acid is a conventional peel with 25% TCA acting as a superficial peel. Black peel, a combination of 50% black acetic acid, 0.5% salicylic acid, 6% tetrahydrojasmonic acid, 10% biosulfur, and 0.1% potassium iodide, is a relatively newer superficial to medium depth peel.[7]
MATERIALS AND METHODS
This was a prospective, hospital-based comparative study. Patients of mild to moderate acne vulgaris were enrolled in the outpatient department of dermatology, Venereology, and Leprology at a tertiary care hospital in North India. Written informed consent to participate in the study was obtained from all patients over the age of 18 and guardians of patients under the age of 18.
PATIENT SELECTION
Thirty patients (or 60 sites) with ages ranging from 15 to 45 years with mild to moderate acne vulgaris were included in the study. Assessment at baseline was done by the global acne grading system score for including mild and moderate acne patients.[8]
THE GLOBAL ACNE GRADING SYSTEM
Factor as per location according to the Global Acne Grading System is as follows:
Forehead––2
Right cheek––2
Left cheek––2
Nose––1
Chin––1
Chest and upper back––3
Depending on severity, each type of lesion is assigned a value:
No lesions = 0
Comedones = 1
Papules = 2
Pustules = 3
Nodules = 4
The scores for each area (Local score) are calculated using the formula: Local score = factor × grade (0–4)
The global score is the sum of the local scores, and it was used to grade the acne severity.
1–18 is categorized as mild, 19–30 as moderate, 31–38 as severe, and >39 as extremely severe.
Patients were excluded if they had severe acne, if they were taking any oral or topical acne treatment within the last four weeks, if the woman was pregnant or lactating, if the patient had a known hypersensitivity to the formulations used in the trial, if the patient had a history of photosensitivity, hypertrophic scars, keloidal propensity, active or recurrent herpes simplex infection, or any type of active dermatosis; and if the patient had unrealistic expectations. A thorough medical history was obtained to eliminate all exclusion criteria.
MATERIALS AND METHODS
A written informed consent was taken from all patients aged ≥ 18 years and guardians of the patients aged less than 18 years before starting the study. A complete history was obtained, and a general examination was conducted in each case and was recorded on the prescribed proforma. At the first visit, a test peel was done with respective peels on right and left postauricular areas of 1 cm2 after cleaning with acetone and spirit. It was left for 15-20 minutes to find any hypersensitivity to ingredients of peeling agent. The patient was reviewed after one week for any type of erythema, crusting, and scaling in the test peel area. The patients who tolerated both the test peels well were taken up for full face peel.
Priming was done by applying sunscreen and tretinoin 0.025% cream daily for 2 weeks before the peeling procedure. Application of tretinoin 0.025% cream was stopped 3 days before the procedure.
During the peeling session, the skin was cleaned with spirit and then degreased with acetone. Sensitive areas like the inner canthus of the eyes and nasolabial folds and lips were protected by applying petrolatum jelly over there. The commercially available peeling agents i.e., black peel and 25% TCA peel, were then applied with a cotton tip applicator. The right side of the face which was labeled as area A was treated with black peel. The left side of the face which was labelled as area B was treated with 25% trichloroacetic acid. The end point of the peeling was light frosting with both the peels At some sittings frosting was mild and sometimes very mild. Neutralization is not needed with any of these two peels. The face was then washed with water. The patients were sent home advising avoidance of face washing with any soap for the next 24 hours, avoid sun exposure, and apply sunscreen daily in the morning and then repeat every 3 hours thereafter till evening, every day. This procedure was repeated in a similar way every 2nd week for 3 sessions. Follow-up was done at the end of 2nd, 4th, 8th, and 12th weeks.
ASSESSMENT OF EFFICACY
The evaluation was graded by individual lesion count and photographically at baseline and end of the 2nd, 4th, 8th, and 12th weeks. Improvement was graded according to the 5-point Global Assessment Scale (GAS).
GRADES OF IMPROVEMENT BY REDUCTION IN 5 POINT GLOBAL ASSESSMENT SCALE (GAS)-
Excellent––≥75% improvement in GAS
Good––50% to 74% improvement in GAS
Fair––25 % to 49% improvement in GAS
Poor––less than 25% improvement in GAS
Worse––Result worse than pre-treatment finding
STATISTICAL ANALYSIS
All statistical calculations were performed using (Statistical Package for the Social Science) SPSS 21 version for Microsoft Windows (SPSS Inc., Chicago, IL, USA).[9] A Kolmogorov-Smirnov test was used to determine whether the data had a normal distribution. Using the Mann–Whitney U test, quantitative variables between study groups were compared. The chi-square (χ2) test was used to compare categorical data, and the Fisher exact test was used when the expected frequency was less than 5. A probability value (P value) of less than 0.05 was regarded as statistically significant.
RESULTS
The study was carried out in 30 patients (or 60 sites) of mild to moderate acne vulgaris in the Department of Dermatology, Venereology, and Leprology at a tertiary care hospital in North India. According to GAGS, 90% of the patients had mild acne while the remaining had moderate acne. Approximately 66.7% (20) patients were male and 33.3% (10) patients were female. Among the Indian population, approximately 20%–30% of people belong to Fitzpatrick skin phototype III, 30%–40% to skin phototype IV, 10%–20% to skin phototype V, and 5%–10% to skin phototype VI. In our study, 9 patients were of Fitzpatrick skin phototype III and 21 were of skin phototype IV.
EFFICACY
The mean comedone counts at the end of therapy were significantly lower than the baseline values in area A (P =.001) as well as area B (P =.001). The improvement began after two weeks of therapy and continued to be statistically significant throughout treatment [Figure 1]. However, there was no significant difference between the two areas in terms of the change in comedone counts at the end of therapy (P =.656). The mean percentage improvement in comedone counts from baseline in area A was 56.21% (SD = 8.78%) and in area B 57.26% (SD = 10.51%), without a significant difference (P =.675).
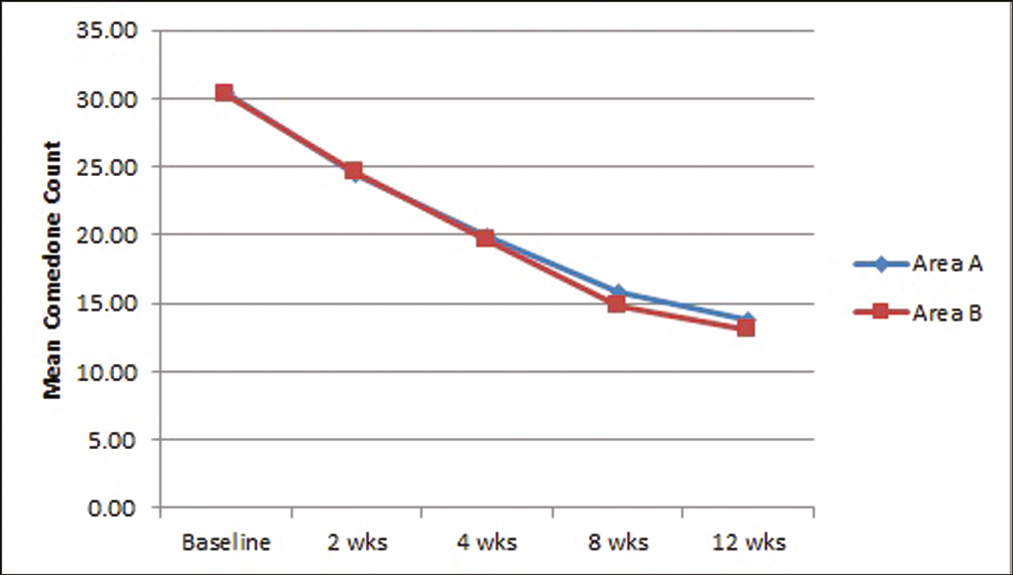
- Showing mean comedone count
There was a significant improvement in mean papule count from the baseline values in area A (P =.001) as well as area B (P =.001). at the end of 12 weeks of therapy. The improvement started at 2 weeks and remained significant throughout the therapy [Figure 2]. At the end of therapy, however, there was no statistically significant difference between the areas (P =.201). The percentage improvement in mean papule count in area A was 60.59% (SD = 8.78%) and in area B 58.04% (SD = 7.99%), without a significant difference (P =.245) after 12 weeks of therapy.
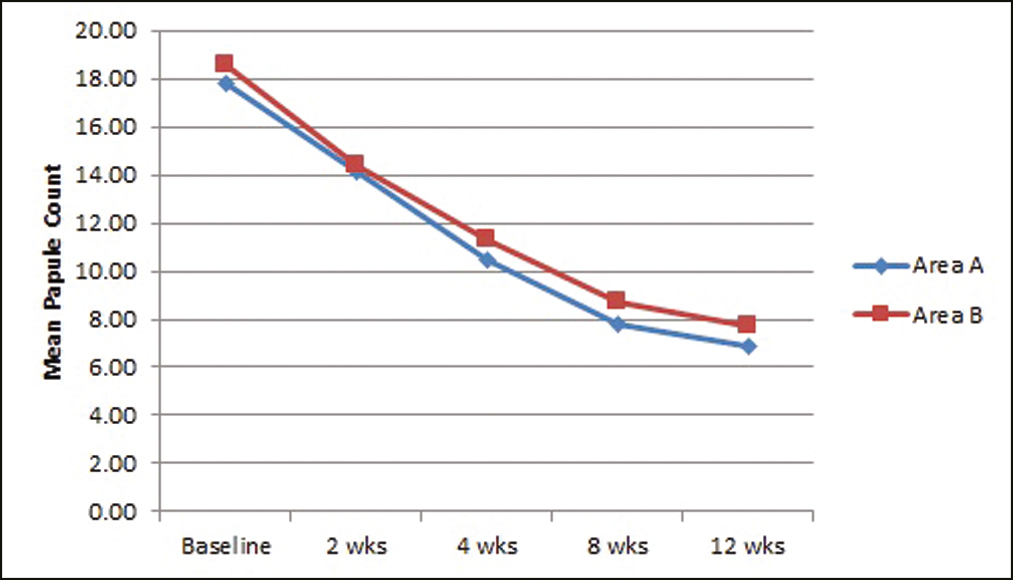
- Showing mean papule count
There was a significant improvement in mean pustule count from the baseline values in area A (P =.027) as well as area B (P =.033) at the end of 12 weeks of treatment. The improvement began at two weeks and persisted throughout the therapy [Figure 3]. At the end of therapy, the difference between the areas in terms of pustule count was not statistically significant (P =.806). The percentage improvement in mean pustule count in areas A and B was 59.72% (SD = 8.67%) and 55.71% (SD = 5.15%), respectively, but the difference was not significant (P =.529).
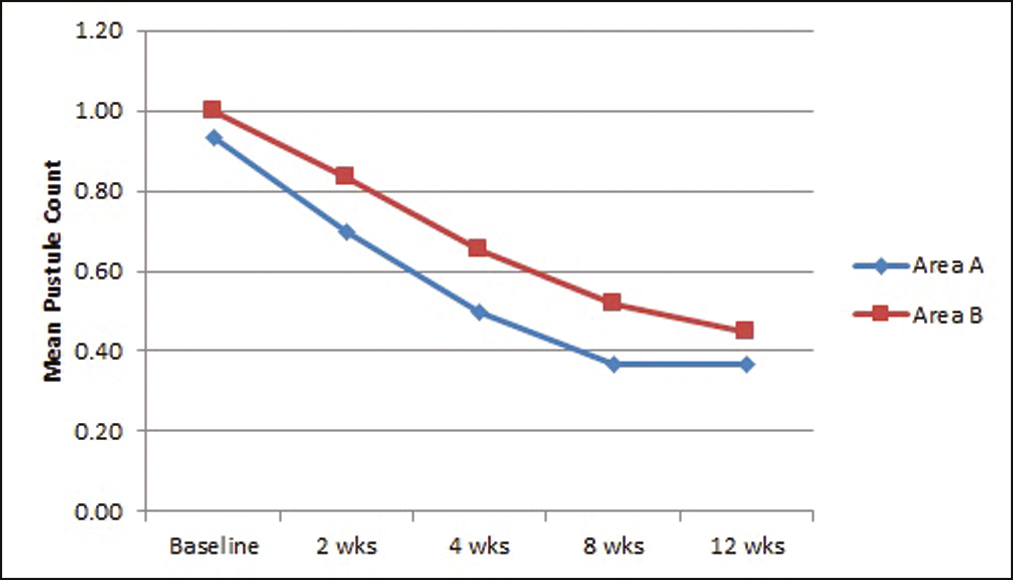
- Showing mean pustule count
There was a significant mean reduction in the total number of lesions in both areas from baseline to the completion of therapy in area A (P =.001) as well as area B (P =.001). However, the difference between the areas was not significant at the end of therapy (P =.922). The overall mean percentage improvement in total lesion count in areas A and B was 57.74% (SD = 7.54%) and 57.59% (SD = 8.12%), respectively, but the difference was not significant (P =.940) [Figure 4].
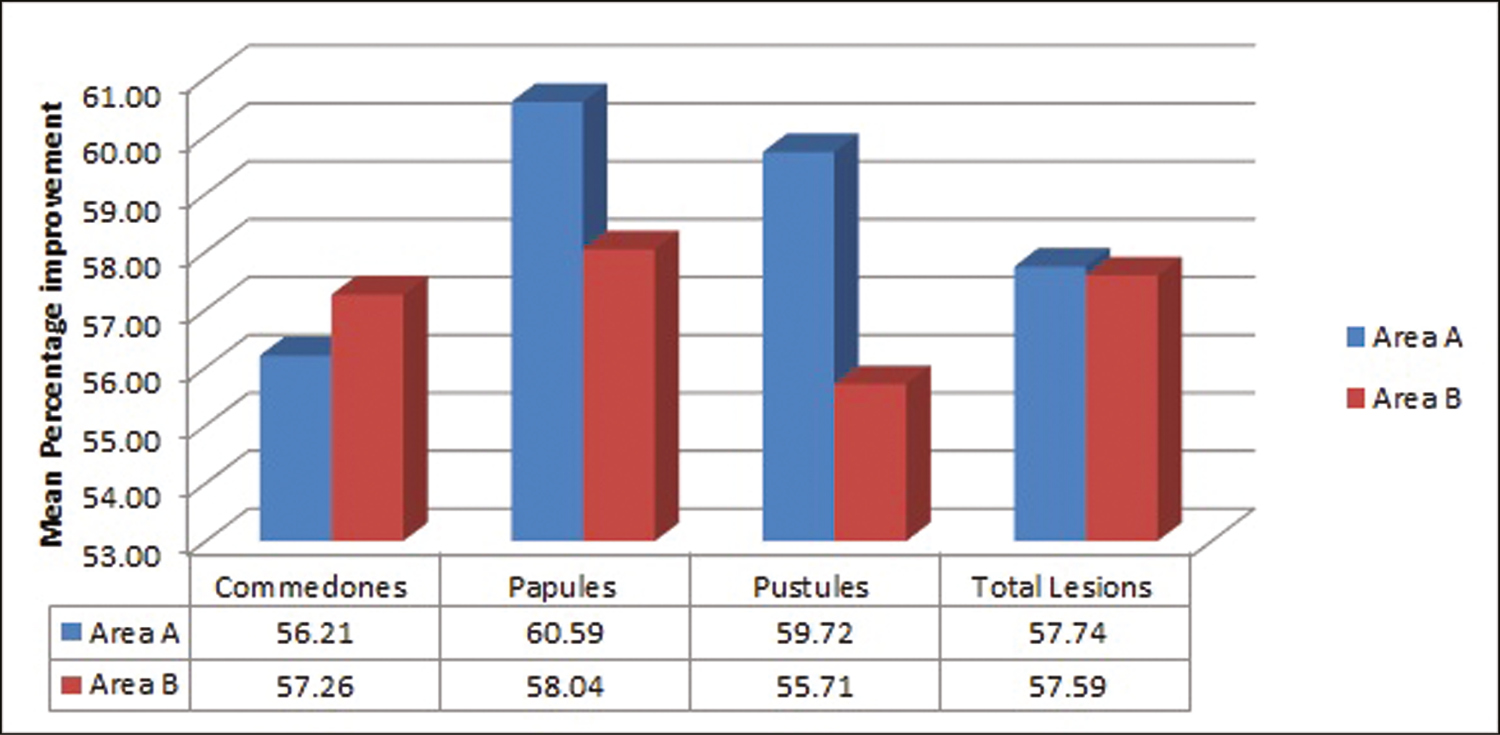
- Showing mean percentage improvement in total lesion count in both the groups
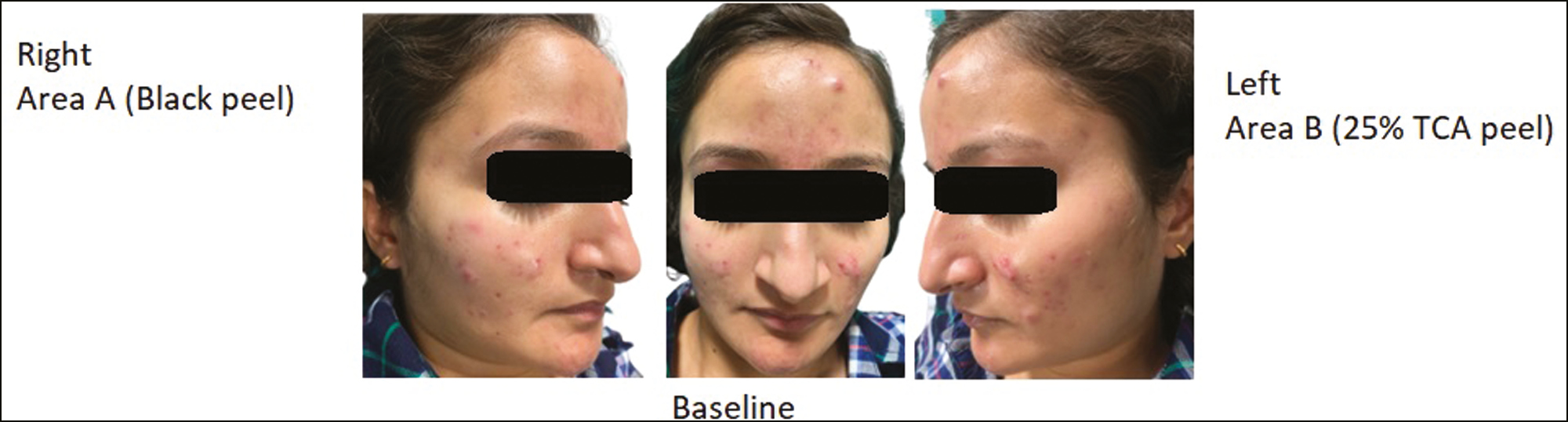
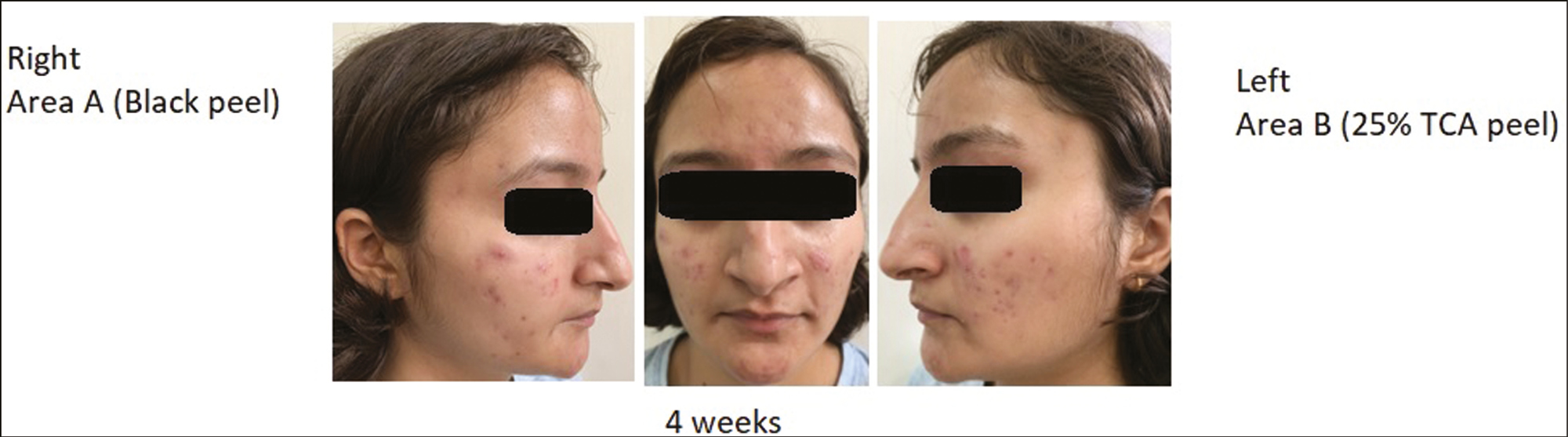
On grading the improvement according to the 5 Point Global Assessment Scale (GAS), it was found that in area A (Black peel), 6.7% of patients showed excellent improvement, 86.7% of patients showed good improvement and 6.7% of patients showed fair improvement. In area B (25%TCA peel), 6.7% of patients showed excellent improvement, 80% of patients showed good improvement and 13.3% of patients showed fair improvement. None of the patients showed poor or worse outcomes in any of the areas. The difference between the groups was not significant (P = 0.688) [Figure 5]. Clinical photographs of two patients at baseline, 4 weeks, and 12 weeks are shown in Figures 6,7,8,9,10,11.
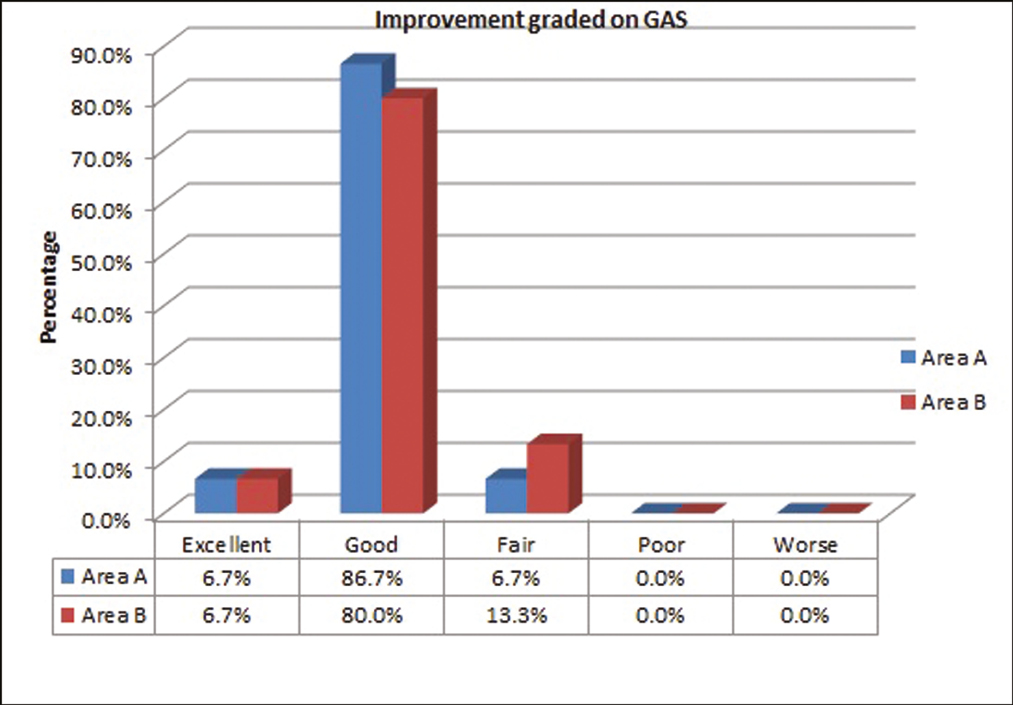
- Showing improvement graded on GAS SCORE

- Baseline picture of 22-year-old patient in both the groups
ADVERSE EFFECTS
No major adverse effects were noted in either of the areas. In the minor side effects, the burning and stinging sensation was observed in 10% of patients in area A and 20% of patients in area B. Post-peel erythema was seen in 6.7% of patients in area A and 16.7% of patients in area B. Approximately 6.7% patients showed post peel visible desquamation and 3.3% patients showed post peel dryness in area B, while none of these was seen in area A [Figure 12].

- Picture of 22-year-old patient in both the groups at 4 weeks

- Picture of 22-year-old patient in both the groups at 12 weeks
- Baseline picture of 20-year-old patient in both the groups
- Picture of 20-year-old patient in both the groups at 4 weeks

- Picture of 20-year-old patient in both the groups at 12 weeks
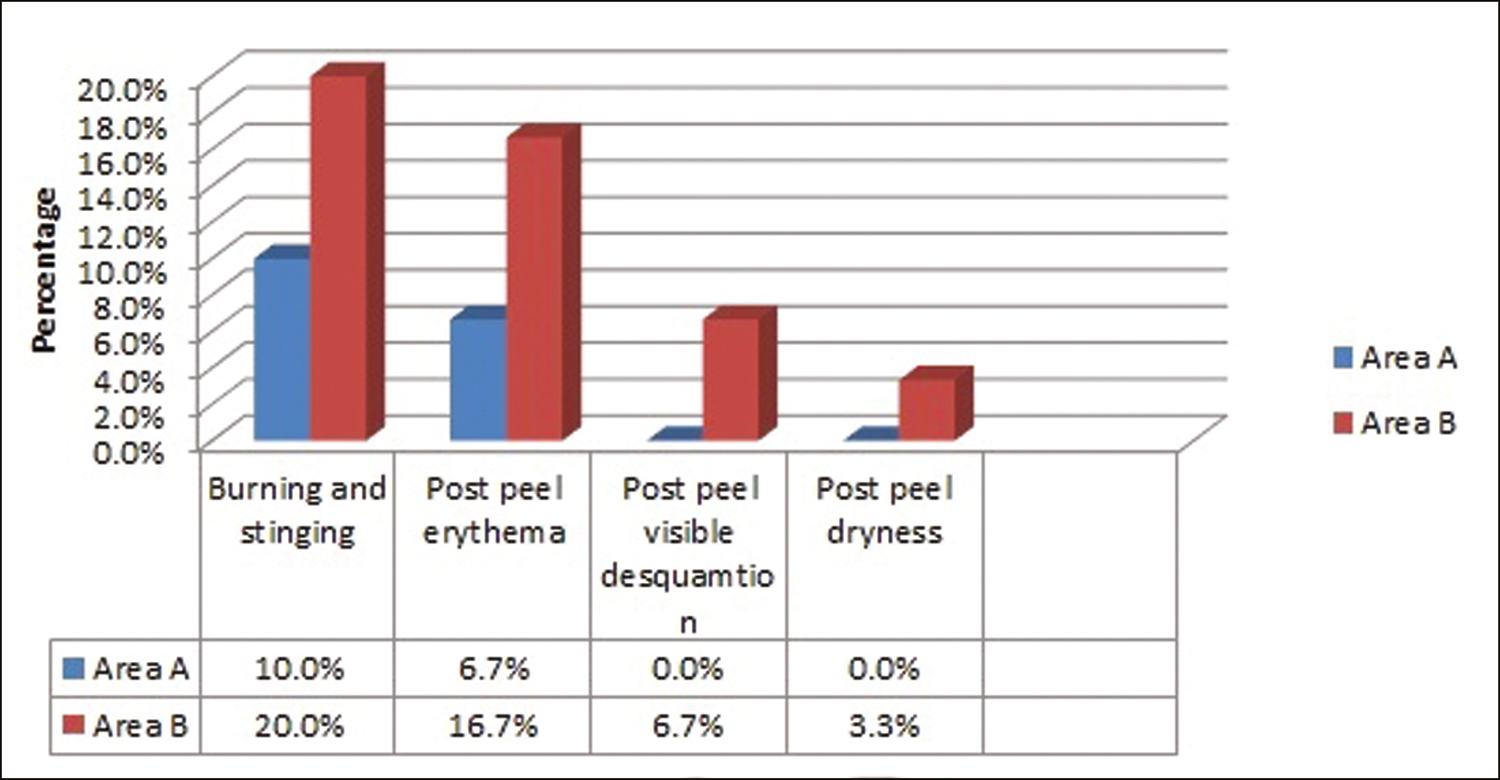
- Showing complications in both the groups
DISCUSSION
Chemical peeling is a safe, effective, and cost-efficient method for treating a variety of skin problems and improving the appearance of the skin.
TCA peel is a conventional peel. Its mechanism of action in the treatment of acne vulgaris is based on its ability to reduce corneocyte cohesion and keratinocyte plugging, thereby contributing to comedolytic action. In addition, TCA causes precipitation of proteins and coagulative necrosis of epidermal cells, resulting in the removal of damaged skin and its replacement with healthy tissue.
Al Hussein Stela Mariana et al. conducted a study in 2014 comparing the efficacy of 20% trichloroacetic acid peel versus 15% topical azelaic acid gel in the treatment of acne vulgaris. Fifty-one patients aged 16 to 40 with mild to moderate acne were randomly assigned to one of two groups. Twenty-seven patients (group A) were administered 15% azelaic acid gel twice daily for eight weeks, while 24 patients (group B) underwent four sessions of 20% TCA peels at 14-day intervals. The effectiveness was determined by counting acne lesions at baseline and after eight weeks. The number of acne lesions decreased by a mean of 32.36% in group A and 69.36% in group B. The mean number of acne lesions after treatment was significantly different (P < 0.00001) between 20% TCA peels and 15% azelaic acid gel; 20% TCA peels demonstrated superior results. In addition, 96% of patients who underwent TCA peels were very satisfied with the results.[10]
Dyal et al. conducted a study on 50 patients with mild or moderate acne vulgaris at the Pt B D Sharma University of Health Sciences in Rohtak, Haryana, in 2020. Patients were randomly divided into two groups of 25. One group received 25% trichloroacetic acid peel, while the other received 30% salicylic acid peel. The procedure was repeated every two weeks for twelve weeks. Both peels resulted in a significant decrease in individual lesion counts and MAS relative to baseline values, with no significant differences between treatment groups. Therefore, the peels were equally effective against acne vulgaris.[11]
Between January 2012 and March 2013, Sharquie et al. conducted an interventional study on 18 patients with active acne vulgaris at the Baghdad Teaching Hospital. One session of chemical peeling with 35% Trichloroacetic acid was administered to patients with active acne vulgaris and three sessions to those with associated scarring. After starting treatment, patients were followed every 2 weeks for 12 weeks, and then every four weeks for 12 weeks after treatment was discontinued. Lesions of active acne vulgaris showed a highly statistically significant reduction after 2 weeks of therapy (P < 0.0001), whereas acne scar scoring showed a reduction ranging from 26% to 50% in 2 patients, 50% to 75% in 2 patients, and greater than 75% in 8 patients (P = 0.000002). After twelve weeks of follow-up, no active lesion recurrence was noted.[12]
Black peel is a newer combination peel consisting of 50% black acetic acid, 0.5% salicylic acid, 6% tetrahydrojasmonic acid, 10% biosulfur, and 0.1% potassium iodide. Traditional methods of producing black acetic acid, often known as fermented vinegar, may be found in both Japan and Korea. It contains a greater quantity of amino acids as well as organic acids.[1314] Black acetic acid has a variety of beneficial properties, including those of an anti-tumor agent, an anti-oxidant, and an antihypertensive.[15-17] When administered topically as a skin dressing, acetic acid demonstrates activity against various bacterial strains like Escherichia coli, Proteus mirabilis, Streptococcus and Enterococcus, and fungal strains like Candida albicans, Aspergillus niger, Aspergillus fumigatus and Cryptococcus neoformins.[18]
Jasmonic acid has effects like exfoliation of the epidermis, elimination of discolouration, and control of sebaceous gland activity. Salicylic acid decreases corneocyte cohesion leading to skin shedding and improvement in comedones. Salicylic acid also inhibits the arachidonic acid pathway leading to a decrease in inflammatory lesions. Potassium iodide (KI) acts as an anti-infective, anti-bacterial, and anti-fungal agent. Because of these properties, it was once used as a topical treatment for a variety of skin disorders. Biosulfur is useful in acne due to its keratolytic and antibacterial properties.[19]
In 2012, a preliminary study employing black peel for acne patients was undertaken by Kim et al. on 13 patients with acne in Korea. 3 sessions of black peel were performed for a total of 6 weeks. Excellent response to treatment with complete clearance of acne was observed in 69% of patients, good response with almost clear skin having rare non-inflammatory papules was observed in 23% of patients while poor response was observed in 7% (1 out of 13). The average pretreatment ISGA scale score of 3.08 improved to 0.38 after treatment (P < 0.0001).[20]
Raj Kumar et al. conducted a prospective observational study on 20 patients with facial nodulocystic acne who were poorly compliant to treatment with isotretinoin, at Baba Raghav Das Medical College, Gorakhpur, Uttar Pradesh. 3 sessions of black peel were performed at 2 weeks of interval. There was a significant decline in the number of nodulocystic lesions. Approximately 55% of patients exhibited an excellent response, 45% had a good response, and none of the patients had a non-responsive response. The post-treatment ISGA score was 0.45, compared to 3.70 before treatment (P = 0.0001).[21]
There is a paucity of data in the literature regarding the comparison of black peel with other conventional peels in the treatment of acne vulgaris. To the best of our knowledge, this is the first study comparing black peel with TCA peel in the treatment of acne vulgaris.
In our study, both black peel and 25% TCA peel led to a significant decrease in individual lesion counts and showed improvement graded on GAS, without significant differences between the peels. Thus, the two peels were equally effective in reducing acne vulgaris. There was a non-significant trend favoring black peel for treating inflammatory lesions and favoring TCA peel for treating non-inflammatory lesions. No major adverse effects were seen in our study, but more patients treated with 25% TCA peel experienced burning, stinging, post-peel erythema, post-peel visible desquamation, and post-peel dryness. Post-inflammatory hyperpigmentation after peeling was not observed with any of the peels.
A limitation of our study is that the acne grading system used for assessing the improvement is not an established grading system. Individual lesion count and total lesion count were done at every visit.
CONCLUSION
Our study demonstrated that both peels led to significant improvement in mild to moderate acne vulgaris and the efficacy of black peel is comparable to that of 25% TCA peel. No serious adverse effects were noted in the study. Black peel is gentler on the skin compared to 25% TCA peel as it showed lesser burning, stinging, post-peel erythema, post-peel visible desquamation, and post-peel dryness but 25% TCA peel can be used as a cost-effective alternate.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The pathological and ecological significance of micro-organisms colonizing acne vulgaris comedones. J Med Microbiol. 1985;20:11-6.
- [Google Scholar]
- Greater tendency to acne in white Americans than in Japanese population. J Clin Endocrinol Metab. 1964;24:267-72.
- [Google Scholar]
- Prevalence of nodulocystic acne in white and Negro males. Arch Dermatol. 1970;102:631-4.
- [Google Scholar]
- A comparative histologic study of the effects of the three peeling agents and dermabrasion on normal and sun damaged skin. Aesth Plast Surg. 1982;6:123-35.
- [Google Scholar]
- Chemical Peeling as an Innovative Treatment Alternative to Oral Antifungals for Onychomycosis in Special Circumstances. Skin Appendage Disord. 2019;5:181-5.
- [Google Scholar]
- A comparison of current acne grading systems and proposal of a novel system. Int J Dermatol. 1997;36:416-8.
- [Google Scholar]
- Trends in the usage of statistical software and their associated study designs in health sciences research: A bibliometric analysis. Cureus. 2021;13:e12639.
- [Google Scholar]
- Eficacy of trichloroacetic acid peel versus 15% topical azelaic acid gel in the treatment of acne vulgaris-a comparative study. Acta Medica Marisiensis. 2015;61:25-30.
- [Google Scholar]
- Efficacy and safety of 25% trichloroacetic acid peel versus 30% salicylic acid peel in mild-to-moderate acne vulgaris: A comparative study. Dermatology Practical & Conceptual. 2021;11:2021063.
- [Google Scholar]
- Treatment of active acne vulgaris by chemical peeling using TCA 35%. JCDSA. 2013;03:32-5.
- [Google Scholar]
- Glycolic acid peels versus amino fruit acid peels for acne. J Cosmet Laser Ther. 2010;12:242-5.
- [Google Scholar]
- Standard guidelines of care for chemical peels. Indian J Dermatol Venereol Leprol. 2008;74:5-12.
- [Google Scholar]
- Extract of vinegar “Kurosu” from unpolished rice inhibits the proliferation of human cancer cells. J Exp Clin Cancer Res. 2004;23:69-75.
- [Google Scholar]
- Extract of Kurosu, vinegar from unpolished rice, inhibits azoxymethane-induced colon carcinogenesis in male F344 rats. Nutr Cancer. 2004;49:170-3.
- [Google Scholar]
- Antioxidant activity of the new black vinegar “IZUMI”. J Nutr Health Aging. 2010;14:845-9.
- [Google Scholar]
- Acetic acid dressings: Finding the Holy Grail for infected wound management. Indian J Plast Surg. 2017;50:273-80.
- [Google Scholar]
- New chemical peel using black acetic acid (black peel) J Cosmet Laser Ther. 2013;15:21-4.
- [Google Scholar]
- A prospective observational study on efficacy of black acetic acid combination peel in patients of facial nodulocystic acne. Int J Res Dermatol. 2019;5:673-7.
- [Google Scholar]






