Translate this page into:
A prospective comparative study of efficacy and safety of 15% trichloroacetic acid peel, 35% glycolic acid peel and Q-switched Nd-YAG laser in patients of macular amyloidosis
Address for correspondence: Dr. Kajal Kansara, Department of Skin and V. D., Wing No. 3, 1st Floor, OPD Building, Civil Hospital, Asarwa, Ahmedabad 380016, Gujarat, India. E-mail: kajalkansara5@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
The unappealing appearance of skin in macular amyloidosis (MA) interferes with the patient’s quality of life, and treating the condition has been challenging.
Aims and Objectives:
To compare the efficacy and safety of 15% trichloroacetic acid (TCA) peel, 35% glycolic acid (GA) peel, and Q-switched Nd-YAG Laser in MA.
Materials and Methods:
Open, prospective study was conducted over 2 years, where after fulfilling the criteria, randomization was done into three groups. Group A: 15% TCA peel; Group B: 35% GA peel; Group C: Q-switched Nd-YAG Laser. Procedures were repeated at monthly intervals for six sittings. On each visit, patients were scored on the following parameters: color score, visual analog score (VAS), physician global assessment (PGA) scale, subjective improvement, and adverse effects.
Results:
A total of 75 patients (25 patients in each group) completed the treatment. The mean age of study-population was 35.68 ± 9.8 years, with female to male ratio of 11.5:1. The mean change in color score (1.68) was more by Group A, followed by Group C (1.4), followed by Group B (1.16). Similar results were noted by subjective improvement, VAS, and PGA. Adverse events were more in Group A, followed by Group C, followed by Group B. No patient showed permanent adverse events.
Conclusion:
TCA-peel showed superior results over Nd-YAG laser and glycolic-acid peel. TCA-peel being cost-effective with excellent acceptability should be considered a treatment modality.
Keywords
Glycolic acid peel
macular amyloidosis
Q switched Nd-YAG laser
trichloroacetic acid peel
INTRODUCTION
Amyloidosis is a disease caused by the misfolding of amyloid proteins. Accumulation of these insoluble fibrillar proteins in tissues can disrupt the function of body organs.[1] Primary cutaneous amyloidosis develops when amyloid deposits build up in the skin.[2] Amyloidosis is a disease with a significant psychological impact on patients due to changes in their physical appearance. These psychological symptoms also have negative effects on the quality of life, mental health, and self-esteem of patients.[2]
Macular amyloidosis (MA) is one of the most common types of primary cutaneous amyloidosis, which often manifests as moderate to intense pruritus in areas with hyperpigmentation. It is usually dispersed in a symmetric manner, and the sites most commonly involved include the upper back, limbs, and rarely the chest and buttocks.[3] Several risk factors, including female gender, sun exposure, genetic predisposition, Epstein–Barr virus, race, and friction, have been associated with the etiopathogenesis of MA.[45]
Treatment of amyloidosis is challenging. Many treatment modalities with variable efficacies have been proposed for the treatment of amyloidosis, including dermabrasion,[67] topical and systemic medications,[89] electrodesiccation,[10] phototherapy and cryosurgery,[1112] and laser therapy.[13]
Recently, some studies have proposed effective MA treatments using different types of peel and laser therapy. In several studies, the efficacy and safety of these approaches in the treatment of MA have been reported.[13-15]
AIMS AND OBJECTIVES
-
A.
To compare the efficacy of 15% trichloroacetic acid (TCA) peel, 35% glycolic acid (GA) peel, and Q-switched Nd-YAG Laser in MA.
-
B.
To study the adverse effect of TCA, GA, and Q-switched Nd YAG laser.
MATERIAL AND METHODS
An open-labeled, randomized prospective interventional study was conducted in the Department of Dermatology in a single tertiary care center after patient consent and approved by the Institutional ethics committee (Ethics committee registration no. ECR/72/Inst/GJ/2013/RR-2019; reference no. 78/2021). Inclusion criteria were patients aged ≥18 age of either sex clinically diagnosed as MA. Exclusion criteria were pregnant or breast-feeding females, history of keloids or hypertrophic scars, active dermatitis at the site, hypersensitivity reaction to TCA or GA, patients with unrealistic expectations, patients not willing to give consent or unable to come on regular follow-up. In some patients, a biopsy was taken to confirm the diagnosis.
After taking prior informed, written consent in a language understood by the patient, relevant history (symptoms, duration, age of onset, history of friction, associated conditions, and treatment history, if any) was elicited, and clinical examination was done. Basic demographic data, residence, contact information, and occupation were noted.
All patients were counseled about the modalities of treatment available and thoroughly explained about outcomes and complications of the treatments offered. Clinical photographs were taken before initiating treatment and at every follow-up visit with proper illumination with Canon Ixus 510 hs camera under fixed manual illumination at a fixed site. A thorough general and systemic examination, including recording of temperature, pulse, respiratory rate, and blood pressure, was done. Skin type (according to Fitzpatrick’s classification), color score, and visual analog score (VAS) was assessed on the screening visit.
Patients selected were randomly allocated into three groups: Group A, Group B, and Group C.
Group A patients were treated with TCA (15%). Prepeel priming was done with GA cream 12% and physical sunscreen for 2 weeks. Test patch with 50% TCA behind the ear was done in every patient 2 weeks prior to peeling. The involved area was degreased with 70% alcohol, and TCA 15% was applied by cotton bud. After a contact period of 3–5 min, neutralization was done with normal saline. If the patient developed frosting early, it was neutralized immediately, even before 3 min.
Group B patients were treated with GA (35%). Prepeel priming was done with GA cream 12% and physical sunscreen for 2 weeks. The involved area was degreased with 70% alcohol, and GA 35% was applied by cotton bud. After a contact period of 3–5 min, neutralization was done with sodium bicarbonate. If the patient developed erythema, it was neutralized immediately, even before 3 min.
Group C patients were treated with Q-switched Nd-YAG laser 1064 nm over the involved area. Eyes were covered with an eye shield, and the involved area was shaved if required. The energy used for the 1064 nm mode of the Nd-YAG laser was 5 J/cm2, with a spot size of 4 mm and a frequency of 10 Hz.
All the patients were advised strict photoprotection for 2 weeks.
Procedures were repeated at monthly intervals for a total of six sittings.
On each visit, patients were scored on the following parameters:
Color score
VAS
Physician global assessment scale (PGA)
Subjective improvement
Adverse effects
Color score (darkness score) developed by Sharquie et al.[1617] was assessed. Score 0 indicates color similar to surrounding, score 1 indicates light brown, score 2 indicates brown, score 3 indicates dark brown, and score 4 indicates black.
Color photography was performed at every visit. The photographs were assessed at the end of the study in computer view, and VAS from 0 to 10 (0—similar to surrounding normal skin to 10—black) was determined for each patient.
At the end of 6 months, improvement was termed excellent if the score was reduced by 7, 8, or 9 from the pretreatment value, good if the score reduces by 4, 5, or 6 from the pretreatment value, and poor if the score reduces by 1, 2, or 3 from pretreatment value.
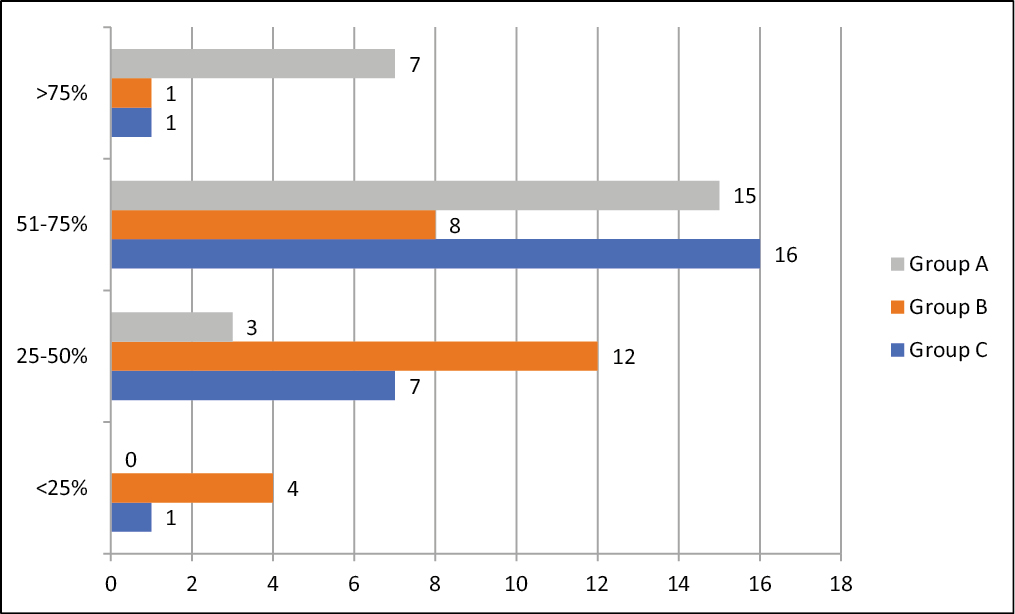
The percentage of improvement in pigmentation was recorded by PGA Scale at the end of treatment in four grades: ≥75%, 50%–75%, 25%–50%, and <25%.
Subjective assessment was done by asking the patient to grade the response (Grade 0 being not satisfied, Grade 1 as moderately satisfied, Grade 2 as greatly but not fully satisfied, and Grade 3 as fully satisfied).
Descriptive and statistical analysis was done using Microsoft Excel 2013. Statistical tests like paired t-tests and analysis of variance (ANOVA) tests were applied to calculate statistically significant differences among Groups A, B, and C and within each group. P value of <0.05 was considered to be statistically significant.
After 6 months, all the patients were observed for 3 months period for the recurrence of the lesion.
RESULTS
A total of 80 patients (Group A—26, Group B—27, Group C—27) were enrolled in the study, of which 75 patients (25 patients in each group) completed the treatment and rest five patients were lost to follow-up due to the COVID-19 pandemic.
The present study was carried out in the Department of a Tertiary Care Hospital; 80 patients were allotted to the three study groups, Group A (TCA), Group B (GA), and Group C (Q-switched Nd-YAG laser). In total, 26 patients were treated with TCA peel, 27 patients with GA peel, and 27 patients with Q-switched Nd-YAG laser.
In total, 75 patients (25 patients in each group) completed the treatment. Thus, statistical analysis for efficacy and safety of treatment modality was done on existing patients (n = 75).
The mean age of the study population was 35.68 ± 9.8 years. The majority of the patients 38.67% (29), were in the age group 30–39 years. The youngest patient was 20 years old, while the oldest patient was 62 years old. 8% (6) were male, and 92% (69) were female, with female to male ratio of 11.5:1. Majority of the patients, 81.33% (61), had Fitzpatrick skin type IV. No patients had skin type I, II, or VI. The mean age of onset was 32.81 ± 9.05 years, with a range of 18–58 years. The mean duration of the disease was 2.86 ± 1.6 years. The maximum duration was 7 years. Overall, 59% (44) patients had pruritus over the site of involvement. There was a history of friction in 63% (47) patients. Six patients were known cases of diabetes mellitus, four patients were hypertensive, and three patients were having hypothyroidism. Family history of similar lesions was present in 22.67% (17) patients.
At the time of presentation, most patients had color score-II (41.33%) or III (40%). Color score IV was seen in 18.67% patients. No patient had a color score-I.
Table 1 shows pre and postprocedure color scores in all groups.
| Color score | Group A precolor score | Group A postcolor score |
|---|---|---|
| A | ||
| I | 0 (0%) | 23 (92%) |
| II | 10 (40%) | 1 (4%) |
| III | 10 (40%) | 1 (4%) |
| IV | 5 (20%) | 0 (0%) |
| Color score | Group B precolor score | Group B postcolor score |
| B | ||
| I | 0 (0%) | 12 (48%) |
| II | 10 (40%) | 10 (40%) |
| III | 10 (40%) | 3 (12%) |
| IV | 5 (20%) | 0 (0%) |
| Color score | Group C precolor score | Group C postcolor score |
| C | ||
| I | 0 (0%) | 23 (92%) |
| II | 11 (44%) | 1 (4%) |
| III | 10 (40%) | 1 (4%) |
| IV | 4 (16%) | 0 (0%) |
After 6 months, the majority of patients had changed their color score grade by one in all three groups, followed by two grades in all groups. A maximum reduction in color score by three grades was seen in Group A. There was no change in color score in 4 (16%) patients in Group B.
Table 2 shows a change in the color score at the end of the treatment.
| Change in score by | Group A | Group B | Group C |
|---|---|---|---|
| 3 | 4 (16%) | 0 (0%) | 1 (4%) |
| 2 | 9 (36%) | 7 (28%) | 7 (28%) |
| 1 | 12 (48%) | 14 (56%) | 17 (68%) |
| 0 | 0 (0%) | 4 (16%) | 0 (0%) |
Table 3 shows the mean change in pretreatment and posttreatment color score.
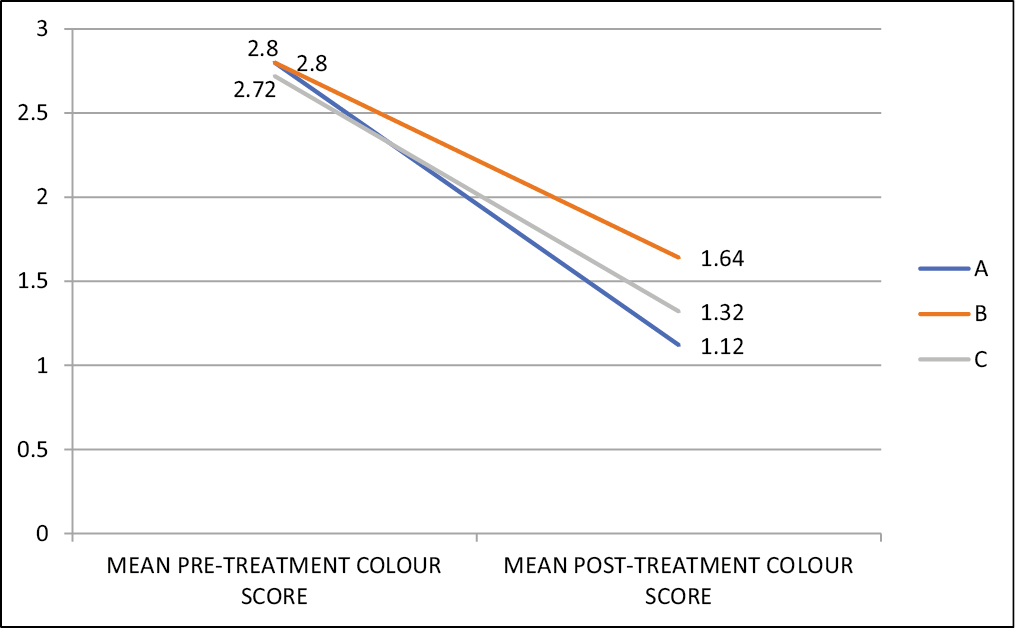 |
Table 3 shows the mean change in color score of Group A (1.68) was more, followed by Group C (1.4), followed by Group B (1.16). These changes were statistically significant. By paired t test, in each group, on comparing the mean color score of pre and postprocedure, the P value is <0.00001, which is highly significant (Df = 24).
On comparing the improvement of a color score of all three groups by one-way ANOVA test, the P-value equals 0.0148958, and the test statistic F equals 4.462313, which is not in the 95% critical value accepted range. P-value is highly significant.
Of all the modalities, Group A showed superior results, followed by Group C, followed by Group B.
Table 4 shows the mean change in pretreatment and posttreatment VAS.
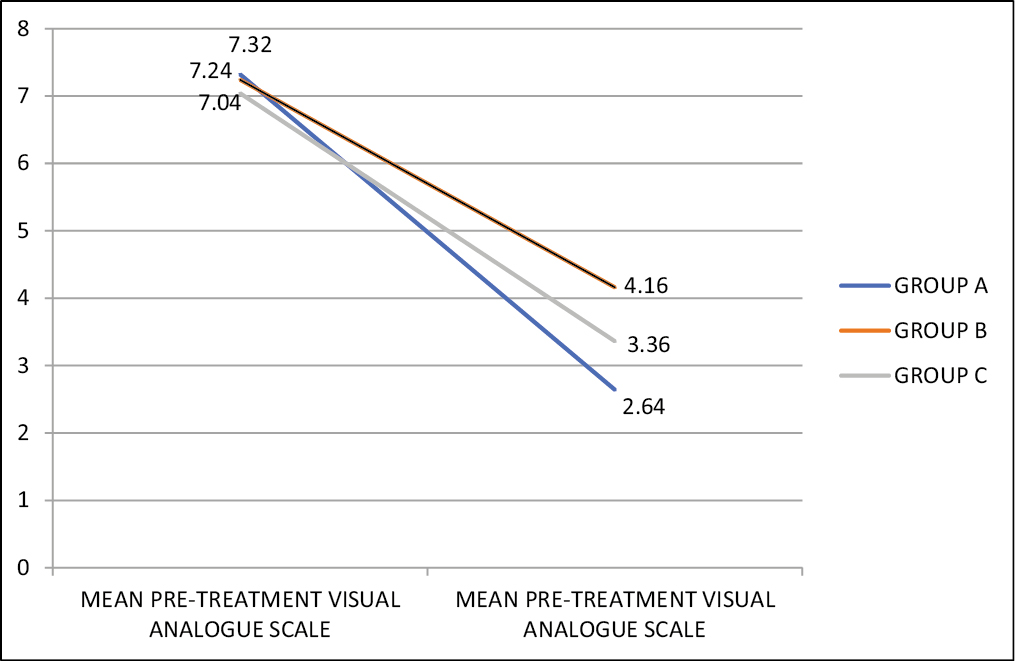 |
On VAS, the mean change in VAS of Group A (4.68) was more, followed by Group C (3.68), followed by Group B (3.08) and the results were statistically significant. By paired t test, in each group, on comparing mean VAS of pre and postprocedure, the P-value is <0.00001, which is highly significant (Df = 24).
On comparing the improvement of VAS in all three groups with each other by one-way ANOVA test, the P-value equals 0.000038554, the test statistic F equals 11.74322397, is not in the 95% critical value accepted range. P-value is highly significant.
Figure 1 shows excellent improvement in Group A; Figure 2 shows good improvement in Group B; Figure 3 shows poor improvement in Group B.

- Group A—Trichloroacetic acid peel showing excellent improvement (A and B: baseline VAS 8, after 6 months VAS 1; C and D: baseline VAS 9, after 6 months VAS 2)
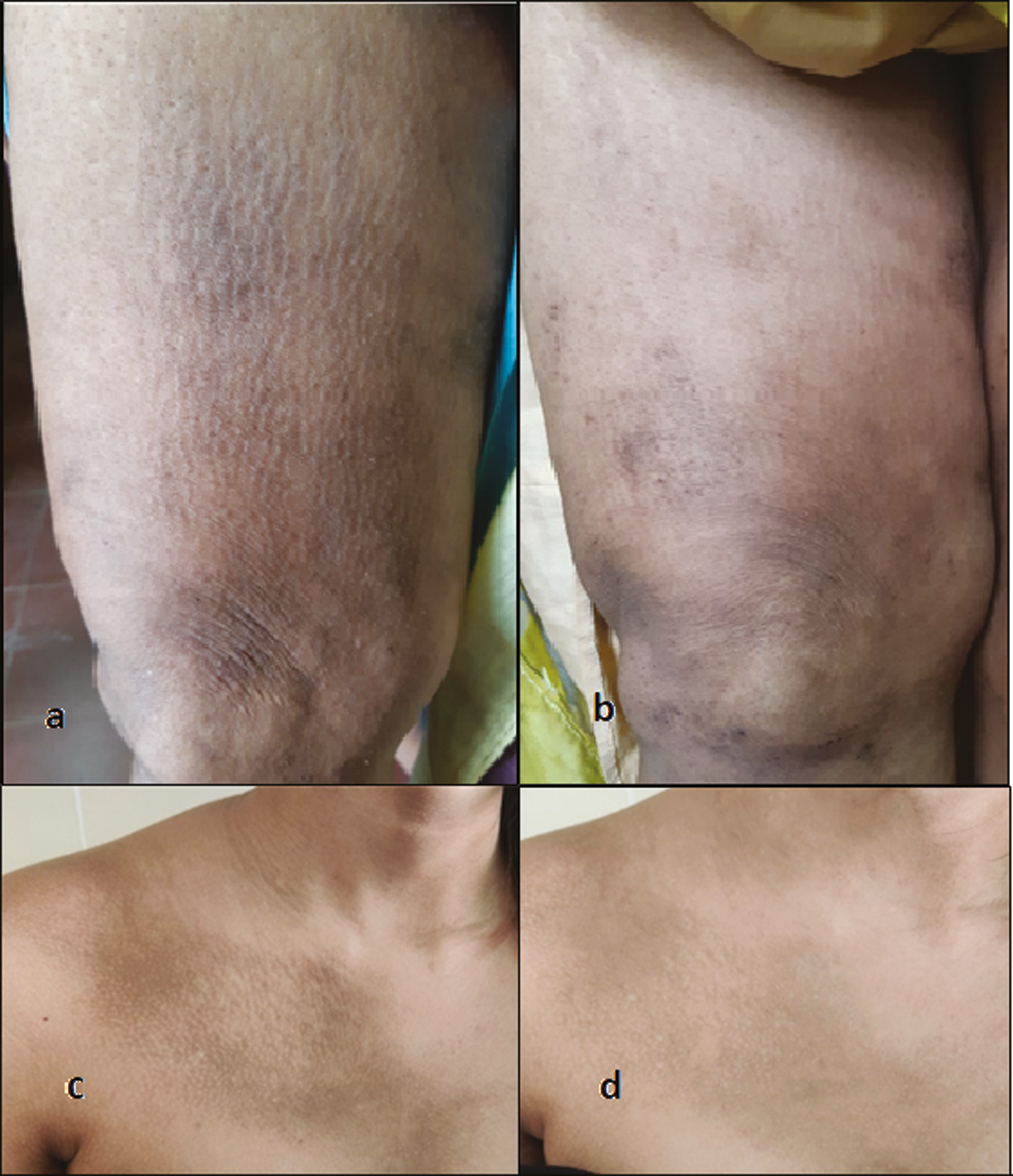
- Group C—Q-switched Nd-YAG laser showing good improvement (A and B: baseline VAS 8, after 6 months VAS 3; C and D: baseline VAS 7, after 6 months VAS 3)

- Group B—Glycolic acid peel showing poor improvement (A and B: baseline VAS 10, after 6 months VAS 8; C and D: baseline VAS 8, after 6 months VAS 7)
PGA scale in terms of the percentage of improvement in pigmentation at the end of treatment showed an improvement by >75% in 28% and 4% each in Groups A, B, and C, respectively. About 51%–75% improvement was observed in 60%, 32%, and 64% in Group A, B, and C, respectively. At the same time, 25%–50% improvement was seen in 12%, 48%, and 28% in Groups A, B, and C, respectively. Improvement of <25% was seen in 16% and 4% patients in Group B and C, respectively. No patients in Group A showed <25% improvement [Table 5].
 |
To summarize the results observed from the color score, VAS, and PGA, TCA peel showed superior results, followed by Nd-YAG laser, followed by GA peel.
In terms of Subjective improvement, 36% patients in Group A were fully satisfied; 56% in Group A, 48% in Group B, and 72% in Group C were greatly but not fully satisfied; 8% in Group A, 36% in Group B and 24% in Group C were moderately satisfied; 16% in Group B and 4% in Group C were not satisfied [Table 6].
| Subjective grade | Group A | Group B | Group C |
|---|---|---|---|
| 3 (Fully satisfied) | 9 (36%) | 0 (0%) | 0 (0%) |
| 2 (Greatly but not fully satisfied) | 14 (56%) | 12 (48%) | 18 (72%) |
| 1 (Moderately satisfied) | 2 (8%) | 9 (36%) | 6 (24%) |
| 0 (Not satisfied) | 0 (0%) | 4 (16%) | 1 (4%) |
Table 7 shows adverse events. Figure 4 shows adverse events in Group A; Figure 5 shows adverse events in Group A. In Group A, erythema, burning, and frosting were seen immediately in seven and nine patients, respectively; in Group B, five patients showed erythema; in Group C, eight patients showed erythema, and 14 patients showed frosting.
| Group | Early | Late | ||||
|---|---|---|---|---|---|---|
| Immediate | Delayed | Hyperpigmentation | Hypopigmentation | |||
| Erythema, burning | Frosting | Crusting | Desquamation | |||
| A | 7 (28%) | 9 (36%) | 2 (8%) | 8 (32%) | 1 (4%) | 1 (4%) |
| B | 5 (20%) | – | – | – | – | – |
| C | 8 (32%) | 14 (56%) | 1 (4%) | 1 (4%) | 1 (4%) | – |

- Adverse events in Group A: (A) immediate frosting after TCA peel, (B) post-TCA peel desquamation, (C) postinflammatory hyperpigmentation after TCA peel, (D) postinflammatory hypopigmentation after TCA peel

- Adverse events in Group C: (A) erythema, crusting, and excoriations after Q-switched Nd-YAG laser, (B) postinflammatory hyperpigmentation after Q-switched Nd-YAG laser
Two patients in Group A and one patient in Group C showed crusting. Eight patients in Group A and one patient in Group C showed desquamation.
In Group A, one patient (4%) had hyperpigmentation, and one patient (4%) had hypopigmentation. In Group C, one (4%) patient had hyperpigmentation. These side effects were treated during the treatment period. Group B patients had no long-term side effects. Patients were followed up for three months posttreatment. No patient had a recurrence of the lesion within 3 months period of observation after treatment.
Based on the results of this study, all three modalities are effective. But TCA peel offers the most efficacious and cost-effective option for patients with MA, especially those who do not respond to topical treatments. With proper pre-procedure counseling and postprocedure care, we were able to prevent or minimize the adverse effects effectively.
DISCUSSION
The unappealing appearance of the skin in MA not only interferes with the patient’s quality of life but also decreases the self-confidence of people, especially when it occurs in young adults.
Topical corticosteroids have been tried for a long period of time, but they have provided very little success. Hence, there is a need for alternate therapeutic options which can provide a long-term sustainable effect with minimal adverse outcomes.
GA peels which provide an aesthetic and therapeutic benefit to the skin with quick recovery time, are now practiced in various pigmentation. GA peels have anti-inflammatory, keratolytic, and antioxidant effects. It targets the corneosome by enhancing breakdown and decreasing cohesiveness, causing desquamation.[1819]
TCA induces coagulation necrosis of the keratinocytes. This inflammatory reaction has stimulatory effects on fibroblasts with new collagen production and restoration of keratinocyte polarity. Their exfoliating effects and the increased epidermal turnover explain their efficacy on MA.[20]
Continuing advances in technology have expanded the dermatologist’s armamentarium to the use of lasers which remove the pigment selectively.
Q-switched Nd YAG lasers deliver high energies and act selectively on the chromophore-sparing surrounding tissues and therefore considered the most effective and safe treatment for benign hyperpigmentations. It induces transepidermal elimination of amyloid deposits and melanin and initiating a controlled inflammatory process and release of certain cytokine production, resulting in decreased itch sensation.[21]
The present study was hence conducted to compare the efficacy and safety of TCA, GA peel, and Q-switched Nd-YAG laser.
A total of 80 patients were enrolled in the study, of which 75 patients (25 patients in each group) completed the treatment. Thus, statistical analysis for efficacy and safety of treatment modality was done on existing patients (n = 75).
In our study, 8% were male, and 92% were female, with female to male ratio of 11.5:1. In study by Ozkaya-Bayazit et al.[17] 15.4% were male, and 84.6% were female, with female to male ratio of 5.4:1, and in Krishna et al.[22] 28.95% were male, and 71.05% were female, with female to male ratio of 2.45:1.
The reason for the predominance in young patients and females in our study could be suggested by the fact that they tend to be more aware as far as cosmesis is concerned and may present to the clinic early.
The majority of the patients, 81.33% (61), had Fitzpatrick skin type IV. No patients had skin type-I, II, or VI in our study. These results were comparable to the study done by Radmanesh et al.,[23] which reported that 70.6% had skin type IV, while higher prevalence in patients with skin type III in Jowkar et al.[21]
In our study, mean age of onset was 32.81 ± 9.05 years. The mean duration of the disease was 2.86 ± 1.6 years. The mean duration of disease was 9.9 and 7.5 years in Ozkaya-Bayazit et al.[17] and Terao et al.,[24] respectively.
59% patients had pruritus over the site of involvement. In a study done by Radmanesh et al.[23] 64.7% patients had pruritus, while it was present in 86% patients in another study done by Jowkar et al.[21] The degree of pruritus ranged from mild to severe. Along with cosmetic disfigurement, severe pruritus can also significantly impair the quality of life of these patients.
There was a history of friction in 63% patients in our study, while Krishna et al.[22] showed 37.5% patients had a history of friction. A study by Jowkar et al.[21] showed a history of friction in 54% patients.
Family history of similar lesions was present in 22.67% (17) patients, which corroborates with the findings of other research workers, i.e., 28% in Jowkar et al.[21] and 20.8% in Krishna et al.[22] Radmanesh et al.[23] showed 52.9% patients having positive family history. High familial occurrence of this condition can be partially explained by inherited mutations in some genes.
In a study by Sacchidanand et al.,[25] 40 patients with MA were divided into two equal groups; one group was treated with 15%-TCA peel and another group with 50%-GA peel. Four peels were done once every 15 days.
Table 8 shows a comparison between our study and the study done by Sacchidanand et al.[25]
| Our study, 2019–2021 | Sacchidanand et al. 25 | |
|---|---|---|
| No. of patients | 25 in each group | 20 in each group |
| Mean age | 35.7 years | 30.7 years |
| Mean disease duration | 2.8 years | 3 years |
| Family history | 22.67% | 22.5% |
| TCA peel group | ||
| • Mean precolor score | 2.8 | 3.5 |
| • Mean postcolor score | 1.12 | 1.45 |
| • Mean change in color score | 1.6 | 2.05 |
| Glycolic acid peel group | ||
| • Mean precolor score | 2.8 | 3.4 |
| • Mean postcolor score | 1.64 | 1.75 |
| • Mean change in color score | 1.16 | 1.65 |
| Subjective improvement in the TCA peel group | ||
| • Fully satisfied | 36% | 30% |
| • Greatly but not fully satisfied | 56% | 45% |
| • Moderately satisfied | 8% | 25% |
| • Not satisfied | 0% | 0% |
| Subjective improvement in glycolic acid peel group | ||
| • Fully satisfied | 0% | 5% |
| • Greatly but not fully satisfied | 48% | 65% |
| • Moderately satisfied | 36% | 30% |
| • Not satisfied | 16% | 0% |
| TCA peel group | ||
| • Burning | 28% | 35% |
| • Desquamation | 32% | 45% |
| • Postinflammatory hyperpigmentation | 4% | 5% |
| • Postinflammatory hypopigmentation | 4% | 5% |
| Glycolic acid peel group | ||
| • Burning | 32% | 40% |
| • Desquamation | 0% | 0% |
| • Post inflammatory hyperpigmentation | 0% | 5% |
| • Post inflammatory hypopigmentation | 0% | 0% |
Our study showed significant improvement in color score and VAS in all three groups.
The mean pretreatment color score in Group A was 2.8, which was reduced to 1.12 at the end of the treatment. The mean pretreatment color score in Group B was 2.8, which was reduced to 1.64 at the end of treatment. The mean pretreatment color score in Group C was 2.72, which was reduced to 1.32 at the end of treatment.
The mean pretreatment VAS in Group A was 7.32, which was reduced to 2.64 at the end of treatment. The mean pretreatment VAS in Group B was 7.24, which was reduced to 4.16 at the end of treatment. The mean pretreatment VAS in Group C was 7.04, which was reduced to 3.36 at the end of treatment.
On the PGA scale, a percentage of improvement in pigmentation by >75% in 28% in Group A and 4% each in Group B and C. 51%–75% improvement was observed in 60%, 32%, and 64% in Group A, B, and C respectively. At the same time, 25%–50% improvement was seen in 12%, 48%, and 28% in Group A, B, and C, respectively. An improvement of <25% was seen in 16% and 4% patients in Groups B and C, respectively. No patients in Group A showed <25% improvement.
To summarize the results observed from the color score, VAS, and PGA, TCA peel showed superior results, followed by Nd-YAG laser, followed by GA peel.
In a study done by Nandini and Kumar,[26] the first session of TCA peel was done with 10% of TCA peel, followed by 20 % in further sessions with monthly intervals. Overall, 50% patients showed more than 51% improvement after three sessions. 28% patients showed more than 70% improvement after five sessions. Our study showed 25%–50% improvement in 12% patients, 51%–75% improvement in 60% patients, and >75% improvement in 28% patients after six sessions done at monthly intervals.
In a study done by Nilforoushzadeh et al.,[12] patients were treated with Q-swithced Nd-YAG laser 1064 nm. About 5% patients had poor satisfaction, 25% with moderate satisfaction, and 70% with excellent satisfaction after four sessions done at monthly intervals. These study results were comparable to our study. But, this study showed such results after four laser sessions.
Ostovari et al.[15] compared the efficacy of 532 and 1064-nm wavelength of Q-switched Nd-YAG on 20 patients with MA in a single therapeutic session. They found a treatment result of 90% improvement for those sides treated with 532nm and 60% improvement for those sides treated with 1064 nm.
In our study, in Group A, erythema and frosting were seen immediately in 28% and 36% patients, respectively; in Group B, 20% patients showed erythema; in Group C, 32% patients showed erythema and 56% patients showed frosting. About 8% patients in Group A and 4% patients in Group C showed crusting. 32% patients in Group A and 4% patients in Group C showed desquamation. In Group A, 4% patients had hyperpigmentation, and 4% patients had hypopigmentation. In Group C, 4% patients had hyperpigmentation. These side effects were treated during the treatment period. Group B patients had no long-term side effects.
In a study done by Nandini and Kumar,[26] 92% patients had burning sensation during TCA peel. After 4–5 days, skin peeling started and lasted for 15–20 days. Postinflammatory hyperpigmentation was seen in 16% patients, and postinflammatory hypopigmentation was seen in 4% patients.
A study by Sacchidanand et al.[25] showed burning immediately after peel in 35% and 40% patients treated with TCA peel and GA peel, respectively. Desquamation was seen in 45% in the TCA peel group only. About 5% patients had postinflammatory hyperpigmentation in both groups, while hypopigmentation was seen only in the TCA peel group (5%).
To summarize the discussion, all three modalities are effective, but the efficacy of the TCA peel was better as compared to the Q-switched Nd-YAG laser, which was later followed by the GA peel. TCA peel offers the most efficacious and cost-effective option for patients with MA, especially those who do not respond to topical treatments. With proper pre-procedure counseling and postprocedure care, we were able to prevent or minimize the adverse effects effectively. No patient had permanent adverse effects in our study. No patient had a recurrence of the lesion within 3 months period of observation after treatment.
Limitation of study
Small group study. Long-term follow-up is required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Amyloidosis: Pathogenesis and new therapeutic options. J Clin Oncol. 2011;29:1924-33.
- [Google Scholar]
- Dermabrasion for lichen amyloidosus: Report of a long-term study. Arch Dermatol. 1982;118:302-4.
- [Google Scholar]
- Therapeutic regional dermabrasion in papular lichen amyloidosis of shins. Indian J Dermatol Venereol Leprol. 1995;61:196-201.
- [Google Scholar]
- Calcipotriol ointment vs. betamethasone 17-valerate ointment in the treatment of lichen amyloidosis. Int J Dermatol. 1999;38:539-41.
- [Google Scholar]
- Comparative study of phototherapy (UVB) vs. photochemotherapy (PUVA) vs. topical steroids in the treatment of primary cutaneous lichen amyloidosis. Photodermatol Photoimmunol Photomed. 2001;17:42-3.
- [Google Scholar]
- Lichen amyloidosis of the auricular concha: Successful treatment with electrodesiccation. J Dermatol. 2009;36:116-7.
- [Google Scholar]
- Liquid nitrogen cryotherapy for conjunctival amyloidosis. Arch Ophthalmol. 2009;127:645-8.
- [Google Scholar]
- Treatment of primary cutaneous amyloidosis with laser: A review of the literature. Lasers Med Sci. 2016;31:1027-35.
- [Google Scholar]
- Histopathology of primary cutaneous amyloidoses and systemic amyloidosis. Clin Dermatol. 1990;8:30-5.
- [Google Scholar]
- A comparative study of the efficacy of fractional neodymium-doped yttrium aluminum garnet (Nd: YAG) laser therapy alone and in combination with erbium: YAG laser therapy: Tracing and objective measurement of melanin index in macular amyloidosis. Lasers Med Sci. 2020;35:1171-7.
- [Google Scholar]
- Friction melanosis, friction amyloidosis, macular amyloidosis, towel melanosis: Many names for the same clinical entity. Eur J Dermatol. 2001;11:545-8.
- [Google Scholar]
- Efficacy of different modes of fractional CO2 laser in the treatment of primary cutaneous amyloidosis: A randomized clinical trial. Lasers Surg Med. 2015;47:388-95.
- [Google Scholar]
- 532-nm and 1064-nm Q-switched Nd: YAG laser therapy for reduction of pigmentation in macular amyloidosis patches. J Eur Acad Dermatol Venereol. 2008;22:442-6.
- [Google Scholar]
- Lactic acid as a new therapeutic peeling agent in melasma. Dermatol Surg. 2005;31:149-54.
- [Google Scholar]
- Local DMSO treatment of macular and popular amyloidosis. Der Hautarzt; Zeitschrift fur Dermatologie, Venerologie, und verwandte Gebiete. 1997;48:31-7.
- [Google Scholar]
- A practical approach to chemical peels: a review of fundamentals and step-by-step algorithmic protocol for treatment. J Clin Aesthetic Dermatol. 2018;11:21-8.
- [Google Scholar]
- Mode of action of glycolic acid on human stratum corneum: Ultrastructural and functional evaluation of the epidermal barrier. Arch Dermatol Res. 1997;289:404-9.
- [Google Scholar]
- A randomized, split-face clinical trial of low-fluence Q-switched neodymium-doped yttrium aluminum garnet (1,064 nm) laser versus low-fluence Q-switched alexandrite laser (755 nm) for the treatment of facial melasma. Lasers Surg Med. 2014;46:531-7.
- [Google Scholar]
- Clinicopathological evaluation of patients with rippled pattern pigmentation of the skin: A single-center study. Dermatol Ther. 2020;33:e13278.
- [Google Scholar]
- Study on epidemiology of cutaneous amyloidosis in northern India and effectiveness of dimethylsulphoxide in cutaneous amyloidosis. Indian Dermatol Online J. 2012;3:182-6.
- [Google Scholar]
- Comparing the efficacy of pulsed dye laser, QSwitched Nd-YAG, CO2, and combined CO2 and Q-Switched Nd-YAG lasers for the treatment of cutaneous macular amyloidosis. J Dermatol Treat. 2021;32:258-60.
- [Google Scholar]
- Clinical effect of tocoretinate on lichen and macular amyloidosis. J Dermatol. 2011;38:179-84.
- [Google Scholar]
- Efficacy of 15% trichloroacetic acid and 50% glycolic acid peel in the treatment of frictional melanosis: A comparative study. J Cutan Aesthet Surg. 2015;8:37-41.
- [Google Scholar]
- TCA peel in the treatment of macular amyloidosis. J Evol Med Dental Sci. 2014;3:11090-6.
- [Google Scholar]






