Translate this page into:
PRP and its benefit as an adjunctive therapy with subcision and microneedling in atrophic scars: a comparative study
Address for correspondence: Dr. Aditi Vashisht, Department of Dermatology, Subharti Medical College, 35, Bank colony, Garh Road, Meerut 250005, Uttar Pradesh, India. E-mail: draditivahisht@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Context:
Scarring is a biological process of wound repair which leads to a difference in the normal structure and function of the skin and manifests as a depressed or raised area. Treatment of scars is challenging. A number of therapeutic approaches like surgical techniques and non-surgical techniques are performed to improve scarring.
Aims and Objectives:
The aim of this study was to compare the outcome of subcision followed by microneedling versus subcision followed by microneedling and topical platelet-rich plasma (PRP) in atrophic scars.
Materials and Methods:
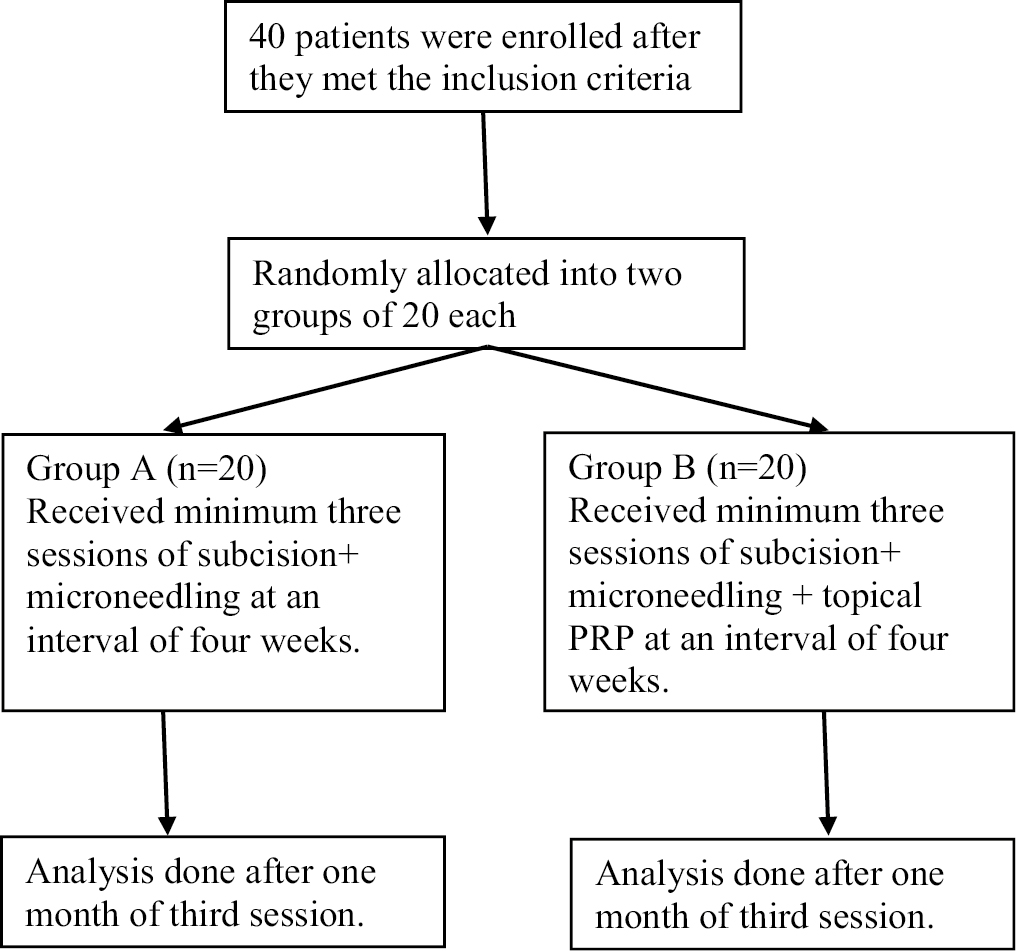
A comparative prospective study was conducted at a tertiary care hospital in North India to compare the efficacy of subcision followed by microneedling versus subcision followed by microneedling and topical PRP. A total of 40 cases were taken and were randomly divided into two groups, A and B of 20 patients in each group. Topical PRP was applied as an additional therapy in Group B in the same sitting. Minimum three sittings were done in each patient at an interval of 4 weeks and results were assessed after 1 month of the third session. The statistical software used is Microsoft Excel and SPSS software program, version 24.0 for analysis of data and Microsoft Word to generate graphs and tables.
Results:
Improvement in scar grading was more in Group B as compared to Group A with statistically significant difference (P = 0.032). There was an improvement in scar grading from grade 4 scar to grade 2 in 15% and 30% patients of Groups A and B, respectively, with improvement in skin texture and pigmentation more in Group B.
Conclusion:
PRP proved to add to the improvement of grade of atrophic scars when combined with subcision and microneedling.
Keywords
acne scars
Atrophic scars
microneedling
platelet-rich plasma
subcision
INTRODUCTION
The word scar originated from Greek word eskhara, which means scab. Scarring manifests as a depressed area and with an alteration of skin texture, color, vascularity, nerve supply and chemical properties.[1]
Treatment of scars is challenging for a physician, hence number of therapeutic approaches like surgical techniques, for example, dermabrasion, microdermabrasion, punch excision, punch grafting, punch elevation, and subcision, as well as nonsurgical techniques, for example, radiofrequency, fillers, peeling, laser, plasma skin regeneration, and intense pulse light have been performed to improve the scarring.[2] Various studies have been conducted to study the efficacy and safety of these procedures.[3,4,5]
One novel technique of treatment of scars is microneedling therapy.[6] It has been used to treat various dermatologic conditions like scars, rhytides and dyschromia.[7] The treatment causes small channels of epidermal and dermal injury through the use of needles that puncture the skin.[8] The damaged collagen is removed and new growth and remodeling subsequently occur.[9] The release of platelet derived growth factors, fibroblasts, and elastic fiber formation contribute to neovascularization and neocollagenesis.[10] Ultimately, this improves the appearance of scars, especially atrophic scars.
Platelet-rich plasma (PRP) has been used as a treatment modality in various conditions (orthopedic, musculoskeletal and maxillofacial disorders), but recently it has gained popularity in dermatology too.[11] PRP is plasma that is enriched with a high concentration of platelets and various growth factors like platelet derived growth factor, transforming growth factor, vascular endothelial growth factor, and insulin like growth factor. These growth factors stimulate tissue remodeling by upregulation of collagen synthesis and enhanced tissue healing.[12]
Microneedling is an efficient treatment option for atrophic scars; but the addition of PRP with it is recently being studied. PRP leads to upregulation of growth factors that further augments tissue remodeling hence causes synergistic effect with microneedling and subcision in the treatment of scars.[13]
MATERIALS AND METHODS
A comparative prospective study was conducted after a prior approval taken from the ethical committee of the university. The objective of the study was to compare the efficacy of subcision followed by microneedling in Group A versus subcision followed by microneedling and topical PRP in Group B patients attending dermatology outpatient department at a tertiary care hospital in north India for one and half year between January 2021 and July 2022. Considering the fact that very less number of patients agree for the procedure to be compared in our study, it was decided to include every patient presenting with atrophic scars during the above mentioned duration in the study after they have given the informed written consent for participation. The participants were then randomly divided into two groups using a chit system which eliminated the patient selection bias. A total of 40 cases were taken and randomly divided into two Groups A and B comprising of 20 patients in each group. The study was an unblinded study. Both the groups received a minimum of three sessions. In Group A, subcision was followed by microneedling in the same sitting followed by second and third session of this combination at an interval of 4 weeks. Group B patients underwent subcission and microneedling followed by topical PRP in the same sitting.
Microneedling was done using an electric microneedling pen device with a disposable 12 pin cartridge with the adjustable depth of penetration ranging from 0.5 to 3 mm. Same device was used in every patient in all the sessions. PRP was made using a conventional double spin method using sodium citrate vials for the first soft spin (1500 rpm/15 min) followed by hard spin (3000 rpm/10 min) in sterile vial without any anticoagulant.
Inclusion criteria comprised of patients with atrophic scars only (present anywhere on the body) with grade 2 to grade 4 acne scars, classified on the basis of Goodman’s Qualitative classification and age between 20 and 50 years because scarring is mostly found around the age of 20 and early treatment results in better results. Exclusion criteria included patients with inflammatory acne, any active infection like herpes simplex infection or folliculitis on face, patients on systemic retinoids, any present or past history of keloid, pregnant or lactating females, any history of facial surgery or procedure for scars in past 3 months, present or past history of any bleeding or platelet disorder and patients having unrealistic expectations were excluded from the study. Viral markers were done before the first session in Group B.
Patients who completed the required sessions for the study were only analyzed for the results.
Assessment of the results was achieved objectively and the patients were digitally photographed using the same camera, lighting settings and patient positioning before and 1 month after the completion of three sessions at an interval of 4 weeks. The severity of acne scarring and other atrophic scars was graded according to Goodman’s qualitative global scar grading system [Figure 1][14] before and after treatment.
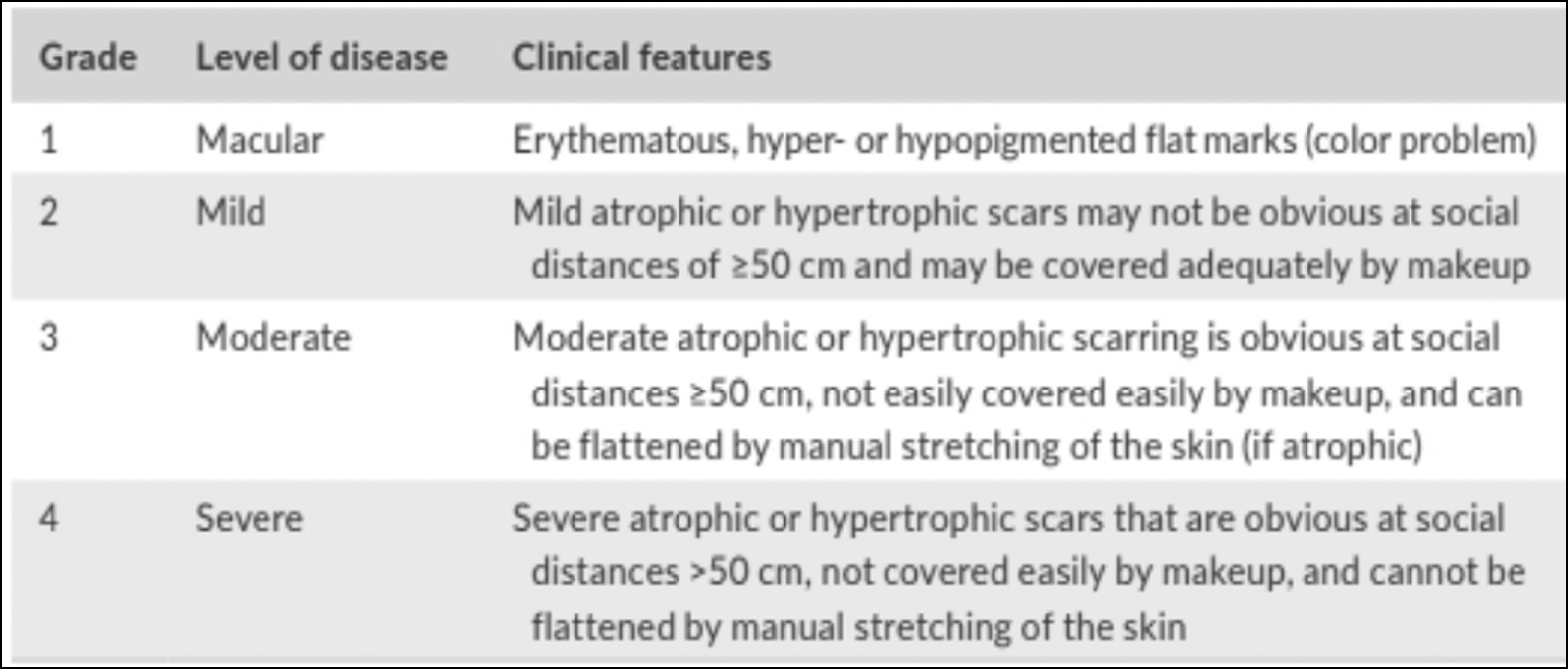
- Acne scarring severity grading per Goodman and Baron
Subjective method: Recording the degree of patient’s satisfaction after three sittings. Patient’s satisfaction score of zero is no improvement and four is excellent improvement.
Statistical analysis
Results on continuous measurement are presented as Mean and SD and results on categorical measurements are presented in number and percentage (%). The significance of study parameters are calculated by Student’s t test for continuous data. Statistical software: The statistical software used is Microsoft Excel and SPSS software version 24 for analysis of data and Microsoft Word to generate graphs, and tables. Difference between the two groups is analyzed using chi square test and P < 0.05 is considered as statistically significant result.
RESULTS
Females were comparatively more as compared to males in both the groups, 15 and 13 in Groups A and B, respectively. Maximum subjects were from the age group of 21–30 years. Maximum subjects in this study were suffering from scar since 1–5 years among both the groups. Fitzpatrick skin type III, IV and V was reported in 4(20%), 11(55%), 5(25%) and 5(25%), 10(50%), 5(25%) of the subjects in Groups A and B, respectively. Most common etiology among the study subjects was acne atrophic scar 15 patients (75%) in both the groups [Figure 2].
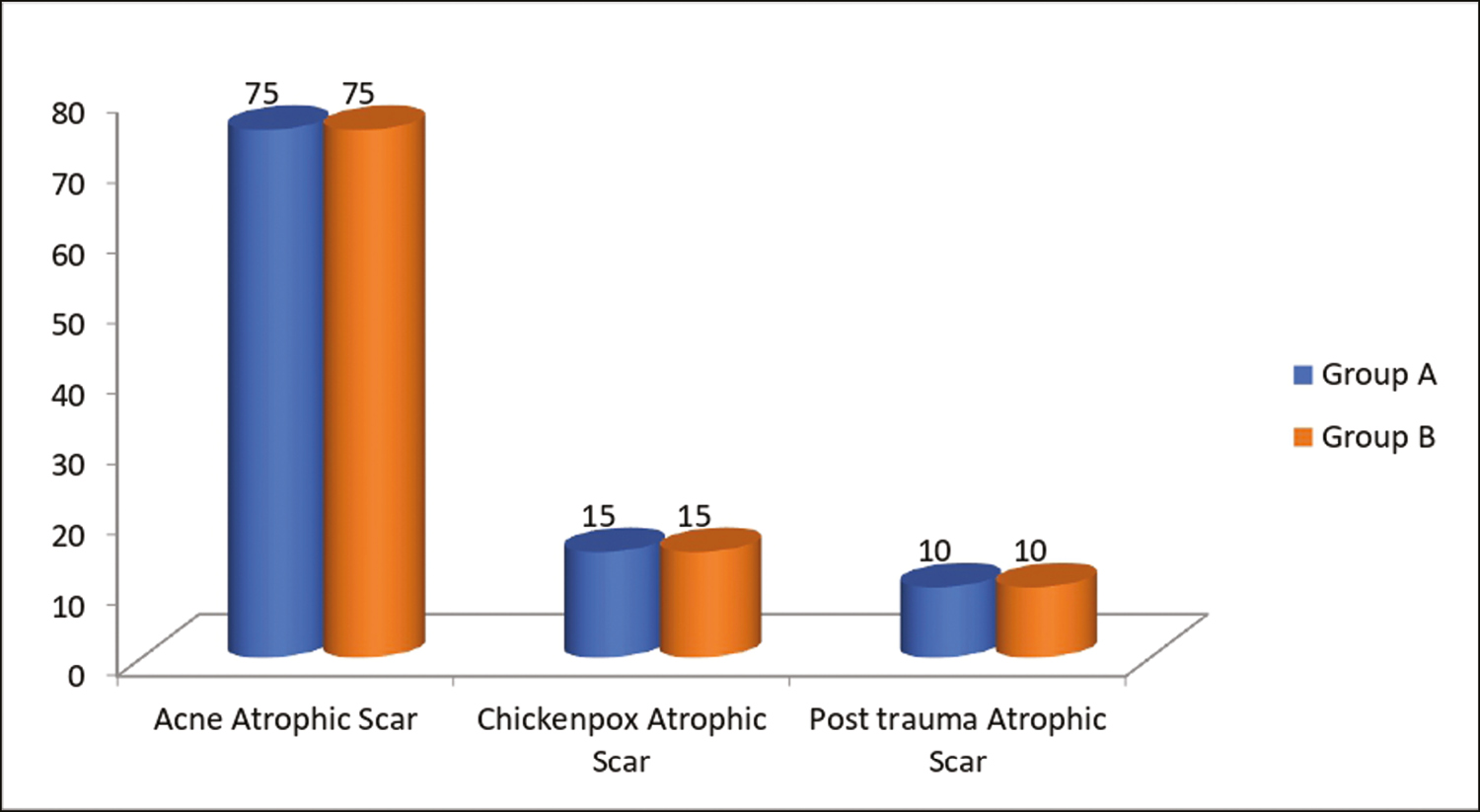
- Types of atrophic acne scars among the study groups
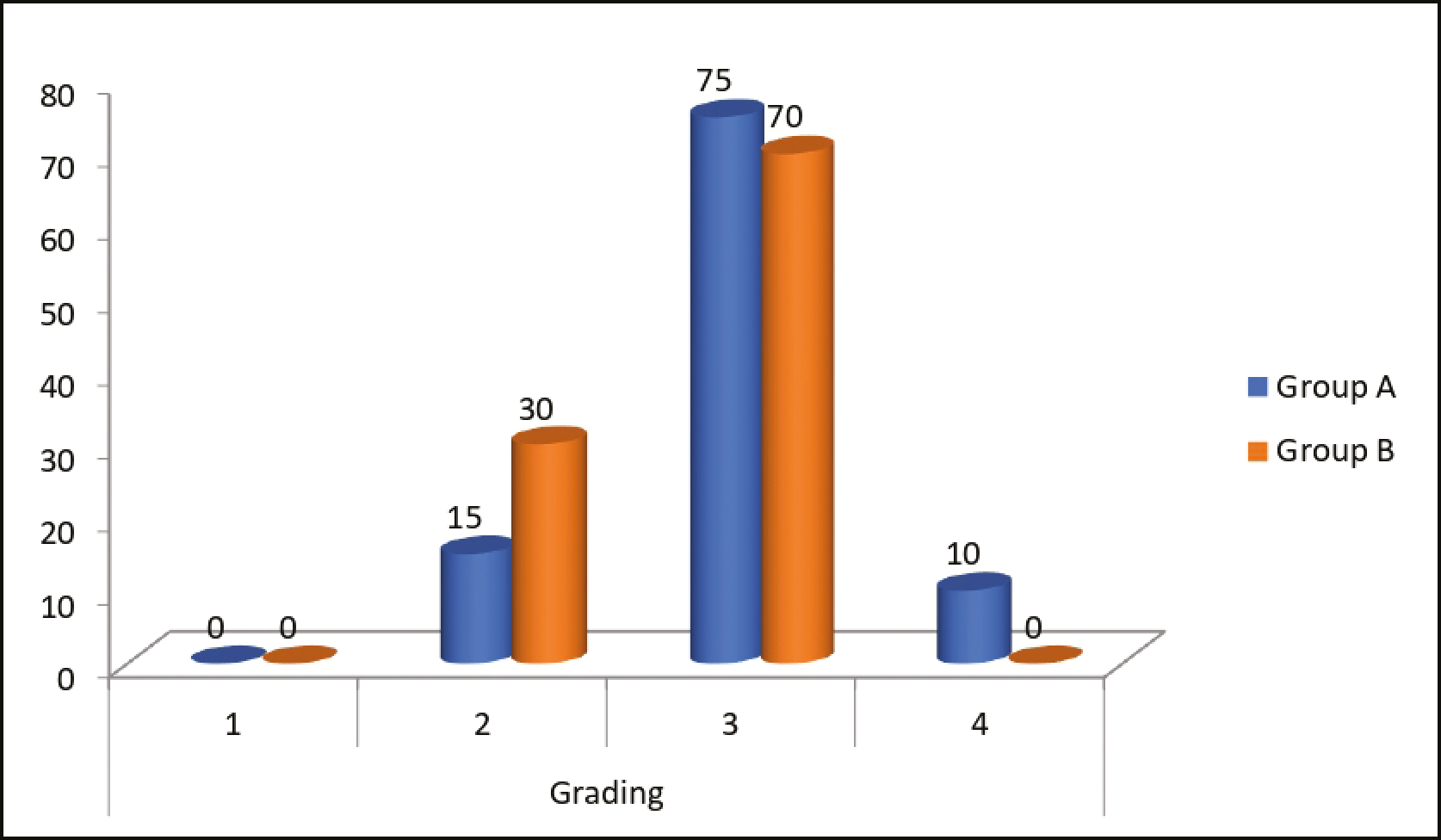
Box scar, rolling and ice pick type was revealed in 5(33.33%), 9(60%), 1(6.67%) and 6(40%), 8(53.33%), 1(6.67%) of the subjects in Groups A and B, respectively. Before intervention, scar grade 4 was found most commonly in Group A 15(75%) as well as Group B 14(70%). Scar grading was comparable among Groups A and B as P = 0.78 before the intervention [Figure 3].
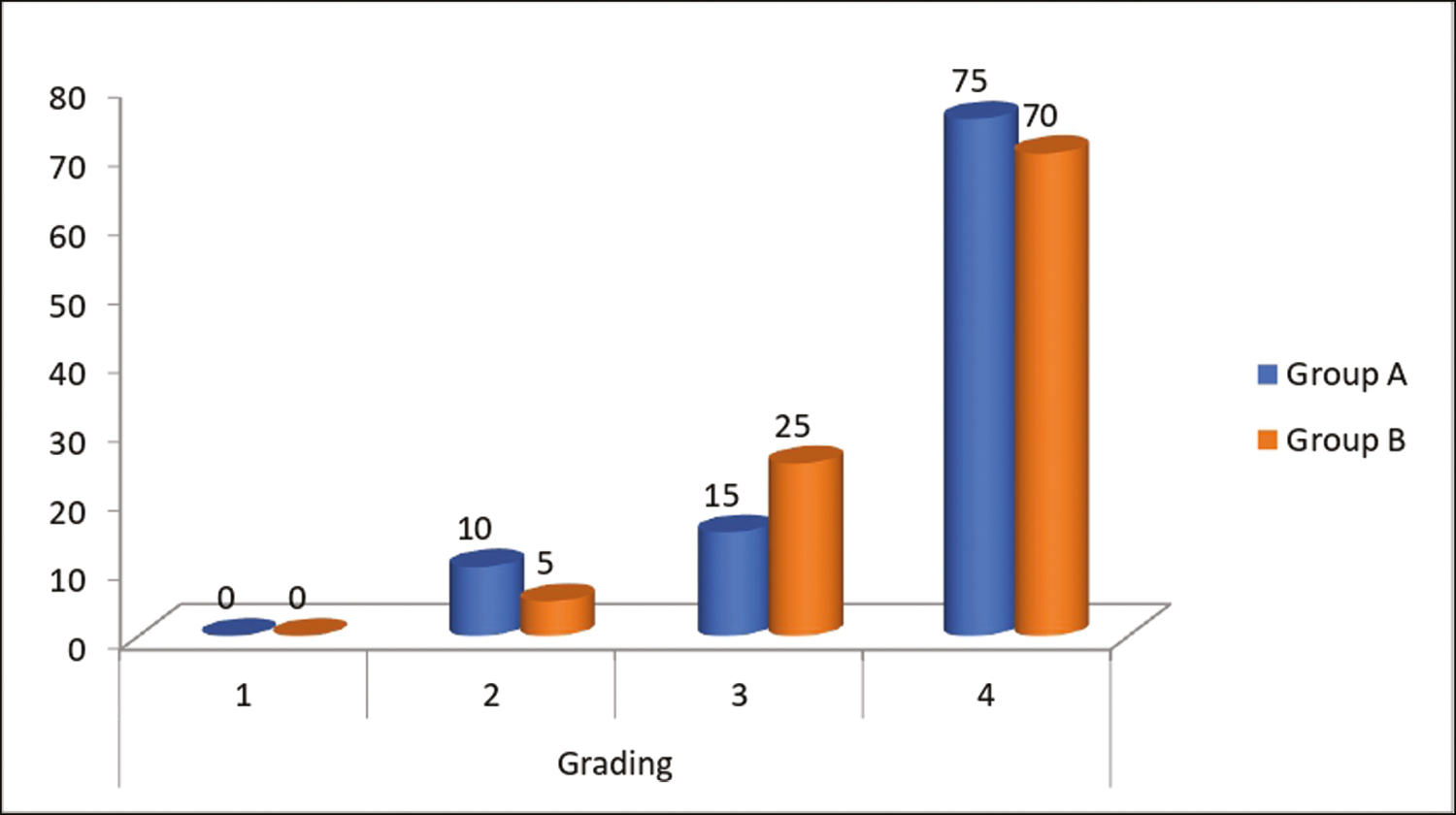
- Comparison of scar grading (Goodman and Baron Qualitative Grading system) before intervention among the study groups
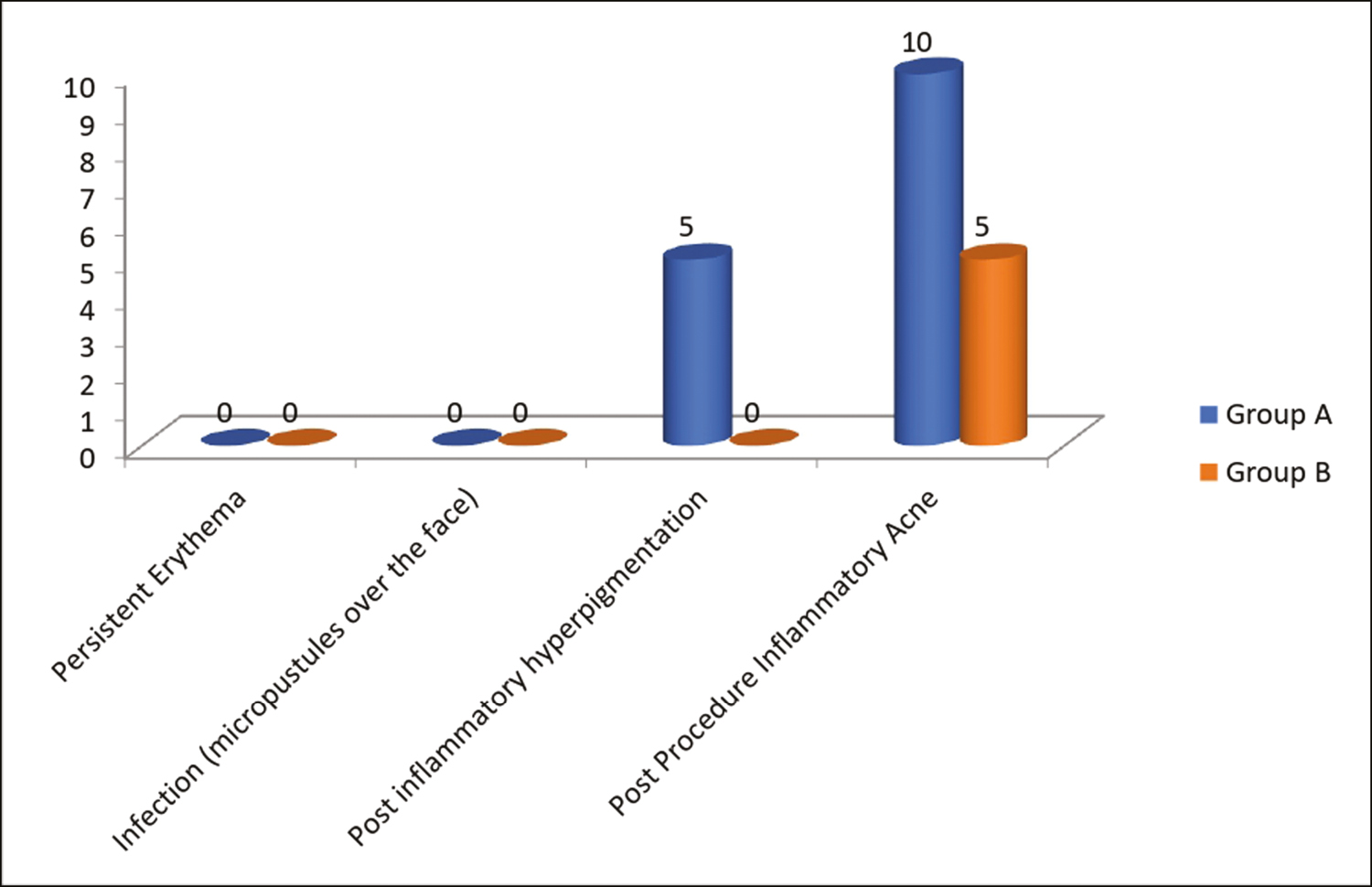
After intervention, scar grading improvement was found to be better in Group B as compared to Group A with statistical significant difference as P = 0.032 [Figure 4]. 2(10%) patients had a scar grade 4 in Group A and none had grade 4 scarring in Group B after the intervention with improvement of 86.6% and 100% in grade 4 scar in Groups A and B, respectively.
- Comparison of scar grading (Goodman and Baron Qualitative Grading system) after intervention among the study groups
According to patient satisfaction score; good and very good improvement was found in 6(30%), 1(5%), and 9(45%), 7(35%) of the subjects in Groups A and B, respectively, with statistically significant difference P = 0.002.
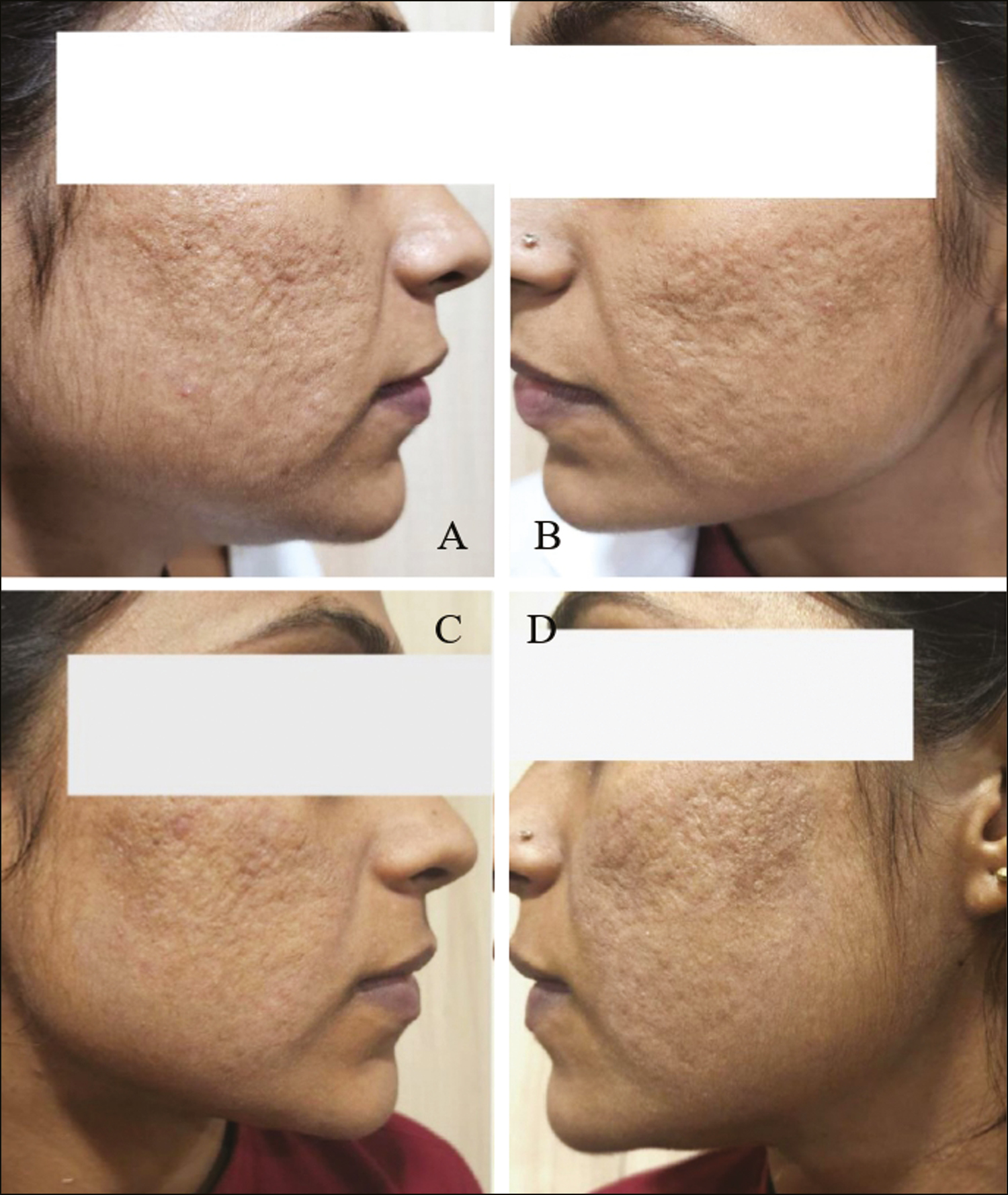
Secondary complications were significantly less in the study groups. Post procedure inflammatory acne was found among 2(10%) and 1(5%) of the subjects in Groups A and B, respectively, and post inflammatory hyper-pigmentation was seen in only one patient in Group A due to inadequate sun protection post procedure [Figure 5].
- Comparison of secondary complications among the study groups
All the patients showed significant improvement in the atrophic scars at the end of study period [Figures 6,7,8,9,10].

- (A and B) Pretreatment photographs of the patient with acne scars. (C and D) Posttreatment photographs 1 month after three sessions of subcision followed by microneedling

- (A and B) Pretreatment photographs of atrophic acne scars. (C and D) Posttreatment photograph after three sessions of subcision and microneedling
- (A and B) Pretreatment photographs of the patient with acne scars. (C and D) Posttreatment photographs 1 month after three sessions of subcision followed by microneedling and topical PRP
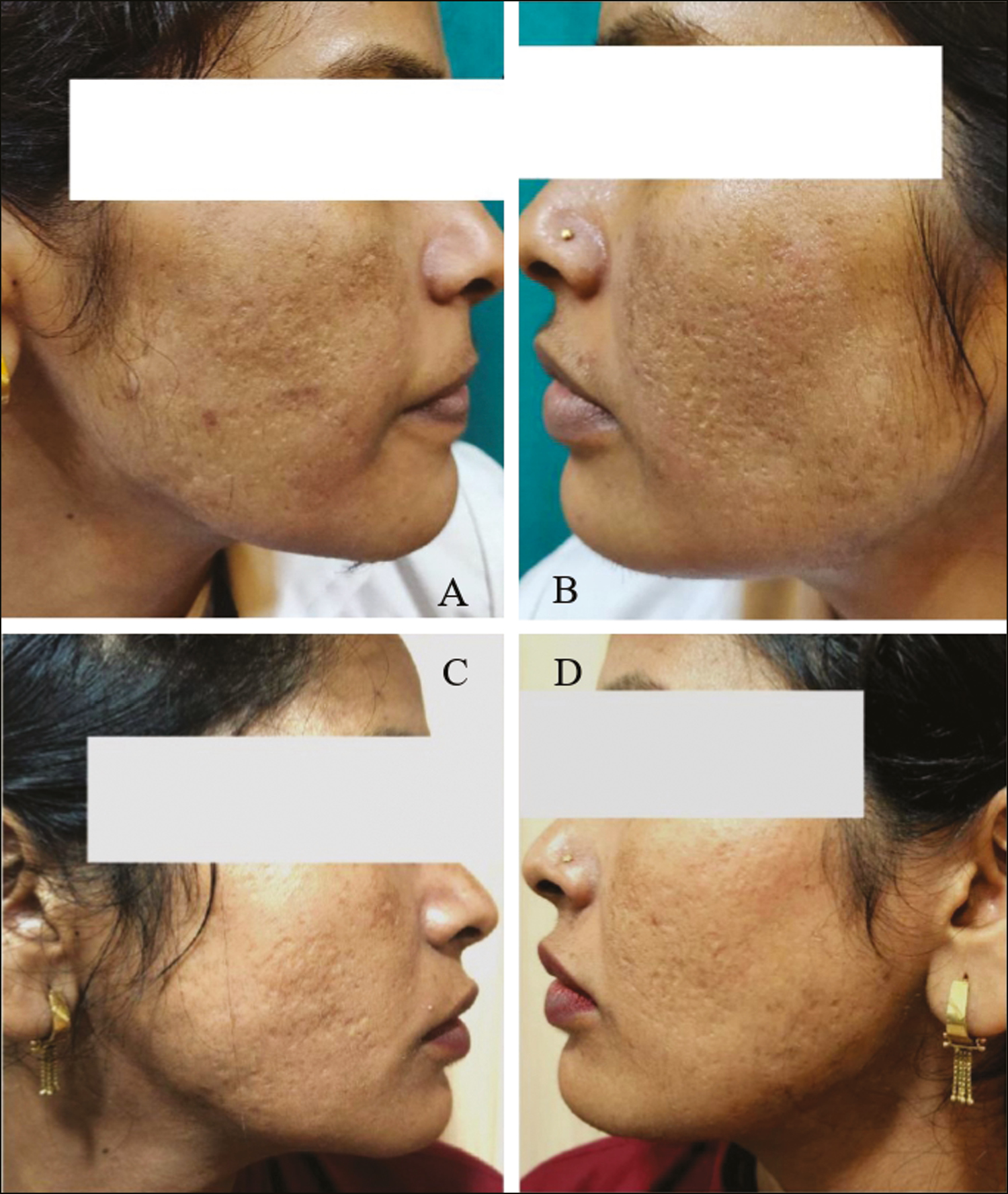
- (A and B) Pretreatment photographs of the patient with acne scars. (C and D) Posttreatment photographs 1 month after three sessions of subcision followed by microneedling and topical PRP

- (A and B) Pretreatment photographs of the patient with acne scars. (C and D) Posttreatment photographs 1 month after three sessions of subcision followed by microneedling and topical PRP shows reduction in scar grading along with significant reduction in pigmentation
DISCUSSION
The process of wound healing is a complicated process whereby the skin repairs itself after injury. The wound healing stages are in the order of: (1) inflammation, (2) granulation tissue formation, and (3) matrix remodeling.[15] The pathogenesis of acne is largely attributed to multiple factors[16] and mostly heals with a sequel of scarring.[17] Hypertrophic and keloidal scars are the result of increased tissue production at the time of healing, and atrophic scars result due to the loss or damage of the tissue.[18] Atrophic acne scars are more common than keloids and hypertrophic scars with a ratio 3:1.[419]
The present prospective interventional study was conducted to compare the efficacy of subcision followed by microneedling in Group A versus subcision followed by microneedling and topical PRP in Group B (containing 20 patients in each group).
Females were comparatively more as compared to males in both the groups. Gender distribution was comparable among the study groups in this study. Studies done by Saurabh Sharma et al.[20] and Meghna Gupta et al.[21] too showed female dominance.
Most common etiology among the study subjects was acne atrophic scar in both the groups. Box scar, rolling and ice pick type was revealed in 33.33%, 60%, 6.67% and 40%, 53.33%, 6.67% of the subjects in Groups A and B, respectively, whereas some estimations report that within atrophic scars, the ice pick type represents 60%–70%, boxcar 20%–30%, and rolling scars 15%–25%.[918]
In the present study; before intervention, scar grade 4 was found most commonly in Group A (75%) as well as Group B (70%). Scar grading was comparable among Groups A and B as P = 0.78 before the intervention. After intervention, scar grading improvement was found to be better in Group B as compared to Group A with statistically significant difference (P = 0.032).
Similarly, Saurabh Sharma et al.[20] in their study reported that the scar grading improved markedly with the combination therapy of microneedling with PRP with the decrease in the scar grade of Goodman and Baron’s scar scoring system. A split face study was conducted by Fabbrocini et al.[22] on acne scars to look for safety and efficacy of micro-needling alone and in combination with PRP. They reported that the mean acne severity score on the side treated by microneedling alone was decreased from 7.5 to 4.9 however the decrease in the score was 7.5 to 4 on the side treated with PRP in addition to micro-needling. Hence better results were obtained on treating the scars with micro-needling followed by PRP.
According to patient satisfaction score; good and very good improvement was found in 30%, 5% and 45%, 35% of the subjects in Groups A and B, respectively. Hence, improvement was found more in Group B as compared to Group A. Gulanikar et al.[23] in their study too showed that on asking the patients to score their satisfaction level from zero to four, 16 patients (53.3%) gave score as three (very good) followed by 14 patients (46.7%) patients who gave score as two (good). However, they revealed findings related to PRP only.
The side effects noted in the study were similar to side effects reported in other studies. In a study Ibrahim et al. reported that edema and erythema that occurred post procedure lasted for less duration of time when treated with combined therapy by microneedling and PRP.[12] Gulanikar AD et al.[23] in their study revealed that PRP is a completely safe procedure. They only noted minor and transient side effects that lasted for a day in majority of the patients. Only one patient developed hyperpigmentation after the fourth sitting which resolved with the treatment.
Rightnow, there are very few researches done to compare the outcome of combination therapy including subcision, microneedling and topical PRP therapy because PRP is a recently studied therapy for the management of acne scars. On the basis of our results micro-needling when combined with PRP application was more efficacious than microneedling alone. However, more elaborative studies are required for establishing the role of PRP as a combination therapy for treating atrophic scars.
Limitations
The findings of this analysis are most generalizable to darker skin types particularly fitzpatrick skin type IV and there is lack of clinical trials comparing other combinations of non-invasive therapies and PRP for the treatment of atrophic scars.
CONCLUSION
Our study’s uniqueness lies in demonstrating the superior efficacy of the combined approach of microneedling and PRP in treating atrophic scars, along with the addition of subcision.
Although similar studies have been conducted in the past, our research specifically showcases statistically significant difference (P = 0.032) between the combined approach and single methods. Moreover, our study brings to light the remarkable outcomes observed in patients with grade 4 scars, with 86.6% and 100% improvement in Groups A and B, respectively. Additionally, the enhanced improvements in skin texture and pigmentation observed in Group B add further weight to the benefits of this combination therapy.
Moreover, this combination therapy does not demand any pricy equipment and can be safely performed in all skin types as post-inflammatory hyper-pigmentation is rarely seen after this combination treatment. Therefore, it is suggested that for better results PRP should be considered as an adjuvant treatment option along with microneedling and subcision in the management of atrophic scars.
However, there is need to strengthen the evidence with larger studies. To the best of our knowledge, there have been no prior studies that have investigated the combination of Subcision, microneedling, and PRP for the treatment of atrophic scars. This unique aspect adds significant value to our study, as it explores an innovative approach that has not been published till date.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Wound healing. In: Burns T, Breathnach S, Cox N, Griffiths C, eds. Rook’s Textbook of Dermatology (7th ed). Oxford: Blackwell Science Ltd; 2004. p. :11.1-11.25.
- [Google Scholar]
- Microneedling therapy in atrophic facial scars: an objective assessment. J Cutaneous Aesthet Surg. 2009;2:26-30.
- [Google Scholar]
- Autologous platelet rich plasma: topical versus intradermal after fractional ablative carbon dioxide laser treatment of atrophic acne scars. Dermatol Surg. 2014;40:152-61.
- [Google Scholar]
- The efficacy of autologous platelet-rich plasma combined with erbium fractional laser therapy for facial acne scars or acne. Mol Med Rep. 2013;8:233-7.
- [Google Scholar]
- Microneedling Therapy for Atrophic Acne Scars: An Objective Evaluation. J Clin Aesthet Dermatol. 2015;8:36-42.
- [Google Scholar]
- Skin needling as a treatment for acne scarring: An up-to-date review of the literature. Int J Womens Dermatol. 2015;1:77-81.
- [Google Scholar]
- Microneedling therapy with and without platelet-rich plasma. Cutis. 2017;99:239-42.
- [Google Scholar]
- Applications and efficacy of platelet-rich plasma in dermatology: A clinical review. J Cosmet Dermatol. 2018;17:660-5.
- [Google Scholar]
- Skin microneedling plus platelet-rich plasma versus skin microneedling alone in the treatment of atrophic post acne scars: a split face comparative study. J Dermatolog Treat. 2018;29:281-6.
- [Google Scholar]
- Microneedling and PRP for acne scars: A new tool in our arsenal. J Cosmet Dermatol. 2020;19:112-4.
- [Google Scholar]
- Postacne scarring: a qualitative global scarring grading system. Dermatol Surg. 2006;32:1458-66.
- [Google Scholar]
- Physiology and healing dynamics of chronic cutaneous wounds. Am J Surg. 1998;176:26S-38S.
- [Google Scholar]
- New developments in our understanding of acne pathogenesis and treatment. Exp Dermatol. 2009;18:821-32.
- [Google Scholar]
- Disorder of sebaceous glands. In: Burns T, Breathnach S, Cox N, Griffiths C, eds. Rook’s Textbook of Dermatology (8th ed.). Oxford: Blackwell; 2010. p. :42.
- [Google Scholar]
- Acne scarring: a classification system and review of treatment options. J Am Acad Dermatol. 2001;45:109-17.
- [Google Scholar]
- Acne scars: pathogenesis, classification and treatment. Dermatol Res Pract. 2010;2010:8-12.
- [Google Scholar]
- A split face comparative study to evaluate the efficacy of skin microneedling and platelet rich plasma (PRP) combination versus skin microneedling alone for treatment of post acne scars. J Pak Assoc Dermatol. 2020;30:449-55.
- [Google Scholar]
- A Comparative Study of Microneedling Alone Versus Along with Platelet-Rich Plasma in Acne Scars. J Cutaneous Aesthet Surg. 2021;14:64-71.
- [Google Scholar]
- Combined use of skin needling and platelet-rich plasma in acne scarring treatment. Cosmet Dermatol. 2011;24:177-83.
- [Google Scholar]






