Translate this page into:
Selective therapy (cryo or scalpel) combined with multimodal therapy for treating keloids
Address for correspondence: Dr. Sushil S. Savant Jr, Department of Dermatology, The Humanitarian Clinic: Skin, Hair and Laser Centre, Ratnagar C.H.S., First floor, Four bunglows signal, Andheri West, Mumbai 400053, Maharashtra, India. E-mail: sushilsavant786@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Keloids are less responsive to any single treatment modality; hence, there is a need for combination therapy that can yield satisfactory outcomes.
Objective:
The present study assessed efficacy and safety of combination therapy—surgical excision or cryotherapy and intralesional corticosteroids along with 5-fluorouracil [IL (S + 5-FU)] injection, followed by silicone gel sheet (SGS) under compression therapy in the treatment of keloids.
Materials and Methods:
This was a retrospective, observational study comprising 21 clinically diagnosed keloid patients. All patients were treated with the stated combination therapy. Data about demographic, lesions, procedural characteristics, and treatment outcomes were reported.
Results:
Of 21, 11 (52.4%) patients were treated with liquid nitrogen (LN2) cryotherapy, and 10 (47.6%) patients were treated with surgical excision. Mean age was 30.8 ± 7.6 (range: 14–44) years with slight male (52.4%) predominance. A mean surface area of keloid lesion was 96.8 ± 170.5 cm3. The most frequently involved site was auricle (8 [38.1%] patients). Patients received the following types of treatments: intralesional LN2 cryotherapy (6 [28.6%]), intralesional excisional surgery (6 [28.6%]), surface LN2 cryotherapy (5 [23.8%]), and extralesional excisional surgery (4 [19.0%]). Complications of recurrence (2 [9.5%]), secondary infections (2 [9.5%]), persistent postinflammatory hypopigmentation (1 [4.8%]), and atrophic scarring with postinflammatory hyperpigmentation (1 [4.8%]) were reported. After a study period of 2.5 years, 100% cure rate was achieved.
Conclusion:
Combination therapy of surgical excision or cryotherapy and IL (S + 5-FU), followed by SGS under compression, was safe and effective in treating keloids.
Keywords
Compression therapy
cryotherapy
intralesional 5-fluorouracil
intralesional corticosteroids
silicone gel sheet
surgical excision
INTRODUCTION
Keloids are exuberant forms of scar formation due to abnormal wound healing in responses to trauma and inflammation, or occasionally occur spontaneously in predisposed individuals, resulting in benign fibrous growth with excessive formation of connective tissue (collagen and glycosaminoglycans). They are raised/flat/pedunculated, firm, painful, pruritic tumors with borders extending beyond original wound and can cause contractile functional problems.[12] Various factors, such as immunological, genetic, fibroblast activity, hypoxia, hormonal, tension, trauma, and inflammation, are thought to be responsible for the development of keloid scars. Various treatment modalities include radiation,[1,2,3,4,5] corticosteroid injection,[1,2,3,4,5] surgical excision,[1,2,3,4,5,6,7] cryotherapy,[1,2,3,4,5,68,9] laser,[2,3,4,58] compression therapy,[2,3,4,5,6] silicone gel sheet (SGS),[2,3,4,5,6] 5-fluorouracil injection,[2,3,4,5,610] and botulinum toxin.[3,4,5] Many of these modalities have been associated with a high recurrence rate. None single effective treatment modality yields satisfactory results; hence, the combination therapies have become popular.[2,3,4,5,611] We have selected surgical excision or cryotherapy in combination with intralesional corticosteroids along with 5-fluorouracil [IL (S + 5-FU)] injection, followed by SGS under compression therapy in the treatment of keloids. With extralesional or intralesional surgical excision, nearly total debulking can be achieved.[1,2,3,4,5,6,7] LN2 cryotherapy (intralesional or surface) achieves debulking through tissue necrosis by cellular destruction and vascular stasis.[13,4,5,6,812] Decreased production and increased breakdown of collagen can be achieved by regulating fibroblasts through other modalities, such as corticosteroids (growth factors),[1,2,3,4,5,610,13] 5-fluorouracil (antimetabolite action),[1,2,3,4,5,610,1113,14] SGS (hydration of keratinocytes),[24,611,13] and compression therapy (decreases blood supply, hypoxia).[2,3,4,5,611,13] This study was carried out to investigate efficacy, safety, recurrence, and aesthetic outcome of combination therapy—surgical excision or cryotherapy and IL (S + 5-FU) injection, followed by SGS under compression therapy in the treatment of keloids. To the best of our knowledge, such an individualized multimodal approach has not been used earlier.
MATERIALS AND METHODS
Study design and participants
This was a retrospective, observational study comprising 21 keloid patients who visited the outpatient department of a tertiary-care institution, Mumbai, India, from June 2018 to June 2019. The patients who were clinically diagnosed with keloid irrespective of age and anatomical site were included. Pregnant or lactating women were excluded. Patients with active local infection were included after controlling infection with broad-spectrum antibiotics. This study was adhered to the tenets outlined in the Declaration of Helsinki, and written informed consent was obtained from each patient.
Data collection
Details about demographic, lesions, procedural characteristics, and treatment outcomes were collected as per the predefined proforma. The recurrence was defined as any elevation with increased firmness, with or without redness. Even if the alteration was minor and the patient was still satisfied with the outcome, these changes were considered as recurrence.
Preoperative workup
The size, shape, number, height, length, width, anatomical location, pigmentation, duration, and current status (growing/static) of keloids were reported. Any previous scars, including Bacillus Calmette-Guérin vaccination, surgery and trauma, were assessed. Custom-made pressure garment was made accordingly.
Procedure
Patients with small nodular or pedunculated keloids were treated with extralesional surgical excision. Patients with auricular keloids were treated with intralesional surgical excision (autoflap-keloid fillet flap). Patients with large bulky lesions (height > 1 cm) or large flat lesions (height > 1 cm) were treated with either modified intralesional (LN2) cryotherapy or modified surface LN2 cryoroller therapy, respectively, and some with both. An appropriate anesthesia (general, regional, local, and tumescent local all have been used) was administered.
Technique
Modified intralesional LN2 cryotherapy
The border of the lesion was pierced with a 1.5-in/3.8-cm-long 18-gauge hypodermic or 3.5-in/8.9-cm long 19-gauge spinal needle at the midpoint (core) of its height. It was maneuvered through across its width to emerge at the opposite side. Both these needles have narrow lumen, thus restricting the periprobe cryoinjury. The guard of the spinal needle was removed. Multiple similar needles were passed 1.5–2 cm apart through entire lesion. The nozzle of either frigitronics gun (CS-76 Cooper Surgical, Trumbull, Connecticut) or handheld cryogun (Derma India Corp., Bangalore, India) was attached through intravenous tubing, respectively, to the hub of the needle, and LN2 was passed through the needle for 20–30 s (freeze cycle) until the ring-shaped freeze zone was visualized at the needle entry and exit sites. Lesion was allowed to thaw completely for 2–3 min (thaw cycle). Two such freeze-thaw cycles were carried out through all the needles, and when dermal edema was observed, all the needles were gently removed. IL (S + 5-FU) was injected, and wound was dressed with antibiotic ointment.
Modified surface LN2 cryoroller therapy
Acetone was applied over the segment of the lesion. A metallic roller of appropriate size among the multiple rollers dipped (5 min) in thermal cup containing LN2 was rapidly rolled 2–3 times with uniform pressure to cover the entire lesion segmentwise. Acetone allows easy slippage, thus avoiding surface cryoinjury. It induced immediate dermal edema; IL (S + 5-FU) was then injected, and wound was dressed with antibiotic ointment.
Extralesional surgical excision
Keloids were completely excised up to the subcutaneous fat along with 3–5 mm of surrounding normal skin. After undermining, IL (S + 5-FU) was injected at the base. The wound was sutured in three layers (subcutaneous and dermal: absorbable vicryl; interrupted epidermal/subcuticular: nonabsorbable prolene) and dressed with antibiotic ointment.
Intralesional surgical excision with autoflap-keloid fillet flap
Intralesional (intramarginal) semicircular “C” shaped incision was taken along the marked border leaving the other side attached. The skin above was dissected from the keloid mass as a flap and reflected back. The exposed keloid mass was debulked either with scalpel or with radiofrequency, and IL (S + 5-FU) was injected at the base. The reflected flap was sutured back to the peripheral margin (interrupted epidermal sutures: nonabsorbable prolene) and dressed with antibiotic ointment.
IL (S + 5-FU) injection
An injection was prepared by mixing ¼ mL, that is, 10 mg of triamcinolone acetonide (TCA) suspension (40 mg/mL), 1 mL of hydrocortisone suspension (25 mg/mL), 1 mL of 5-FU (50 mg/mL), and 1¾ mL of distilled water or 1% lignocaine (total 4 mL). The final concentration was 2.5 mg of TCA, 6.25 mg of hydrocortisone, and 12.5 mg of 5-FU per 1 mL of solution. Using 0.05–0.1 mL at each equidistant point, the entire lesion with its border was injected after cryotherapy (intralesional) or during surgical excision (base). It is important to note that 25 mg of hydrocortisone, 40 mg of TCA, and 50 mg of 5-FU were the maximum amount that could be injected during each session. For large lesions, the prepared solution was further diluted with either distill water or 1% lignocaine as per the requirement to cover the lesion.
Postoperative
Analgesics, antibiotics, and anti-inflammatory drugs were started after the treatment. In patient treated with cryotherapy, dressing was removed after 24 h, and topical ointment was continued until there was epidermal peeling (surface cryotherapy) or until crust fell off 8–10 days (intralesional cryotherapy). In surgically excised patients, dressing was removed at the time of sutures removal (2 weeks). SGS of appropriate size was trimmed as per the size and shape of the lesion and applied over the healed lesion. The patient was instructed to wear the customized pressure dressing/auricular clip over it, daily for 6–8 h until there was a complete flattening.
Schedule
Lesion was reassessed monthly for first 3 months and then 1.5 monthly for the next three times. In patients treated with cryotherapy, multiple similar sessions (3–6) as per the requirement were carried out until the lesion completely regressed and flattened. In patients treated with surgical excision, if required, similar sessions (1–3) were carried out until there was complete resolution. Six IL (S + 5-FU) injections were injected (three at monthly and three at 1.5 monthly intervals) at each follow-up, and they were instructed to continue wearing SGS under compression garments/auricular clip until next treatment session. Maintenance was achieved with further IL (S + 5-FU) injections (0–6) at 2 monthly intervals as per the requirement and continuous use of SGS under compression therapy for 6–12 months until there was a complete resolution and flattening.
Follow-up
Patients were followed up monthly for next 3 months, then every 1.5 month (three times) for next 4.5 months, then every 2 months (six times) for next 1 year, and then 3 monthly totally period of 2.5 years.
Statistical analysis
Quantitative data are presented as mean ± standard deviation, and qualitative data are reported as frequency and percentages. Data were statistically analyzed using the Statistical Package for the Social Sciences software, version 21.0 (IBM Corp., Armonk, New York).
RESULTS
Of total 21 (11 males and 10 females) keloids patients, 11 (52.4%) were treated with LN2 cryotherapy and 10 (47.6%) with surgical excision. The mean age was 30.8 ± 7.6 years with a range of 14−44 years. A mean surface area/volume of keloid lesion was 96.8 ± 170.5 cm3. The most common shape of keloid lesion was bulky (eight patients [38.1%]). Anatomical sites of keloid were as follows: auricle (8 [38.1%]), anterior chest wall (4 [19.0%]), shoulder (2 [9.5%]), bilateral elbow joint (1 [4.8%]), abdomen (1 [4.8%]), nape of neck (1 [4.8%]), left elbow joint (1 [4.8%]), bilateral mandibular margin of face (1 [4.8%]), planter aspect of lower limb (1 [4.8%]), and suprapubic (1 [4.8%]). Patients received the following treatment: intralesional LN2 cryotherapy (6 [28.6%]), intralesional excisional surgery (6 [28.6%]), surface LN2 cryotherapy (5 [23.8%]), and extralesional excisional surgery (4 [19.0%]). Keloids scars were completely healed after receiving the mentioned treatment [Figures 1–5]. Complications of recurrence (2 [9.5%]), secondary infections (2 [9.5%]), persistent postinflammatory hypopigmentation (1 [4.8%]), and atrophic scarring with postinflammatory hyperpigmentation (1 [4.8%)] were noted. After a study period of 2.5 years, 100% cure rate was achieved. A summary of 21 cases with keloid is presented in Table 1.
| Sr. no. | Sex | Age | Size (cm × cm × cm) | Area (cm3) | Shape | Location | Treatment modalities | Treatment (cryotherapy/ surgical excision | Liquid nitrogen (surface cryoroller/ intralesional) | Recurrence |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 38 | 22 × 9 × 4 | 792 | Bulky | Bilateral elbow joint | Multiple | Cryotherapy | Intralesional | Yes |
| 2 | M | 14 | 9 × 13 × 1 | 117 | Flat | Abdomen | Multiple | Cryotherapy | Surface cryoroller | No |
| 3 | F | 41 | 6 × 5 × 0.8 | 24 | Bulky | Anterior chest wall | Multiple | Cryotherapy | Surface cryoroller | No |
| 4 | F | 27 | 4.5 × 6 × 2.5 | 67.5 | Bulky | Shoulder | Multiple | Cryotherapy | Intralesional | No |
| 5 | M | 29 | 5 × 6 × 3 | 90 | Bulky | Nape of neck | Multiple | Cryotherapy | Intralesional | No |
| 6 | M | 34 | 12 × 9 × 1 | 108 | Bulky | Left elbow joint | Multiple | Cryotherapy | Surface cryoroller | No |
| 7 | F | 25 | 2 × 2.5 × 1 | 5 | Nodular | Auricle | Multiple | Cryotherapy | Surface cryoroller | No |
| 8 | M | 29 | 12 × 5× 4 | 240 | Bulky | Bilateral mandibular margin of face | Multiple | Cryotherapy | Intralesional | No |
| 9 | M | 34 | 7 × 8 × 1 | 56 | Flat | Anterior chest wall | Multiple | Cryotherapy | Surface cryoroller | No |
| 10 | F | 39 | 5 × 7 × 3.5 | 122.5 | Bulky | Shoulder | Multiple | Cryotherapy | Intralesional | No |
| 11 | M | 34 | 12 × 9 × 0.9 | 97.2 | Flat | Anterior chest wall | Multiple | Cryotherapy | Surface cryoroller | No |
| 12 | F | 36 | 1.2 × 1.3 × 0.8 | 1.2 | Nodular | Auricle | Single | Surgical excision | Intralesional | No |
| 13 | M | 44 | 9.4 × 4.7 × 2.7 | 119.3 | Bulky | Plantar aspect of lower limb | Multiple | Surgical excision | Extralesional | Yes |
| 14 | F | 21 | 0.6 × 0.5 × 0.9 | 2.7 | Nodular | Auricle | Single | Surgical excision | Extralesional | No |
| 15 | F | 19 | 0.8 × 0.6 × 0.7 | 0.3 | Nodular | Auricle | Single | Surgical excision | Intralesional | No |
| 16 | M | 32 | 7.1 × 6.9 × 1.8 | 88.2 | Flat | Anterior chest wall | Multiple | Surgical excision | Intralesional | No |
| 17 | F | 35 | 1.3 × 1.9 × 1.4 | 3.5 | Nodular | Auricle | Single | Surgical excision | Intralesional | No |
| 18 | M | 28 | 5 × 3 × 4 | 60 | Nodular | Auricle | Multiple | Surgical excision | Intralesional | No |
| 19 | M | 37 | 4.9 × 3.2 × 2.2 | 34.5 | Pedunculated | Suprapubic area | Single | Surgical excision | Extralesional | No |
| 20 | F | 23 | 1.4 × 1.2 × 1.8 | 3.0 | Nodular | Auricle | Single | Surgical excision | Intralesional | No |
| 21 | F | 27 | 0.7 × 0.4 × 0.8 | 0.2 | Pedunculated | Auricle | Single | Surgical excision | Extralesional | No |
F = female, M = male
Transient postoperative pigmentary (de/hypo/hyper) change, which gradually subsided and disappeared over next 6–9 months, was seen in all 11 patients
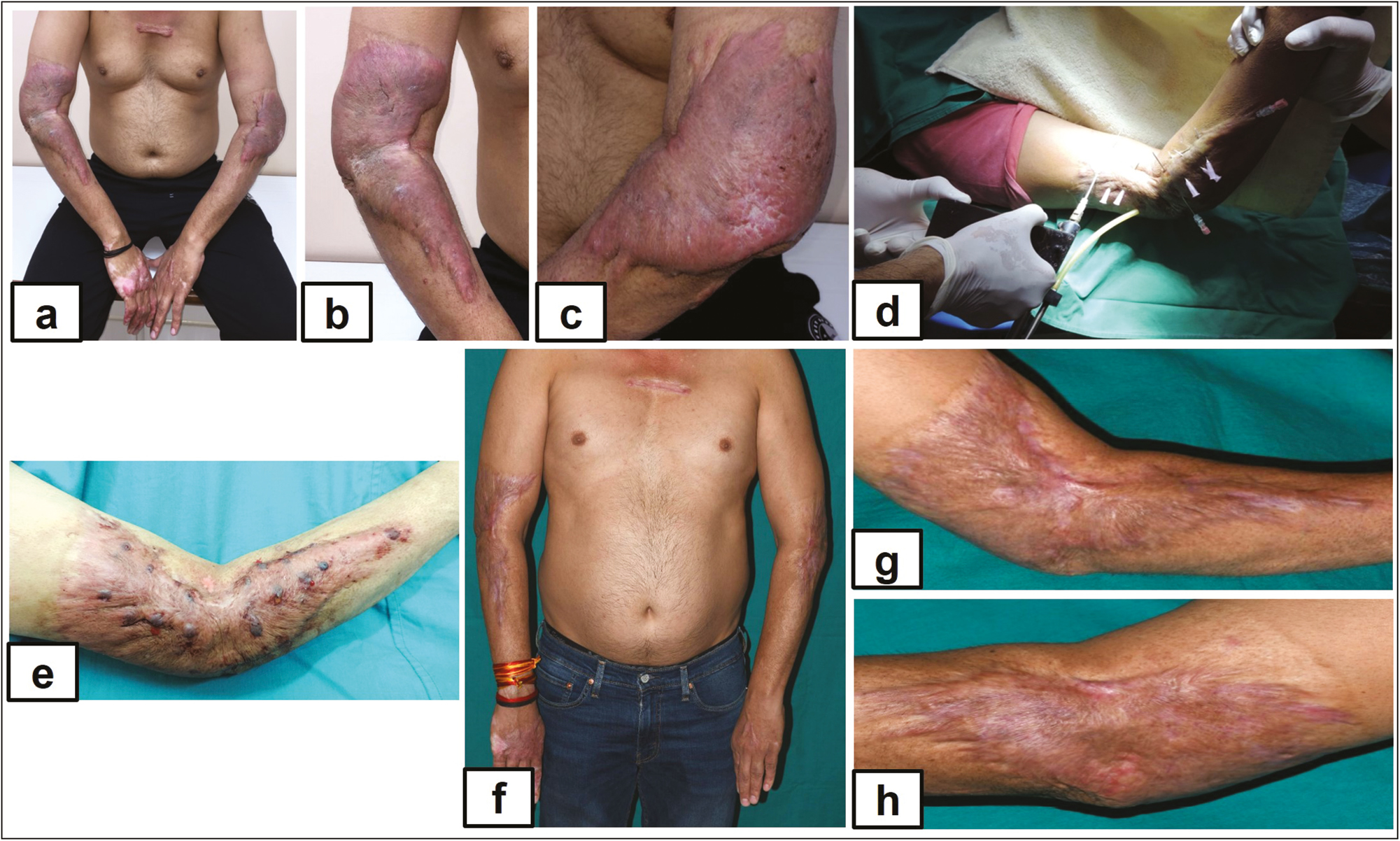
- (A) Multiple bulky keloids on bilateral elbow joint, (B) multiple bulky keloids on bulky keloids right forearm, (C) multiple bulky keloids on left forearm, (D) multiple bulky keloids treated with intralesional cryotherapy, (E) immediate postoperative, (F) complete flattening after six sessions, (G) complete flattening after six sessions, and (H) complete flattening after six sessions
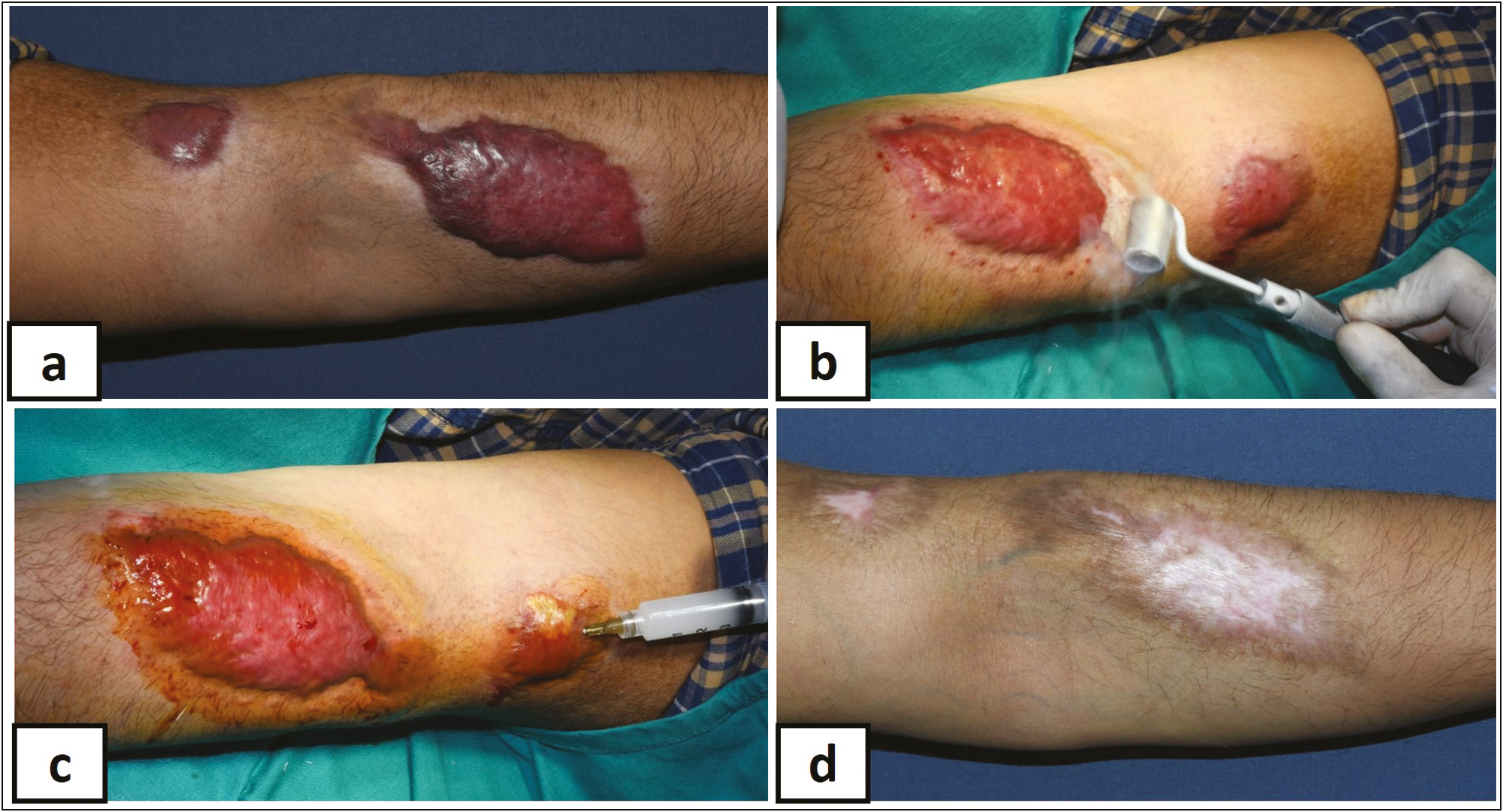
- (A) Flat keloid left forearm, (B) surface ln2 cryo roller, (C) intralesional injection (S + 5-FU), and (D) after four sessions
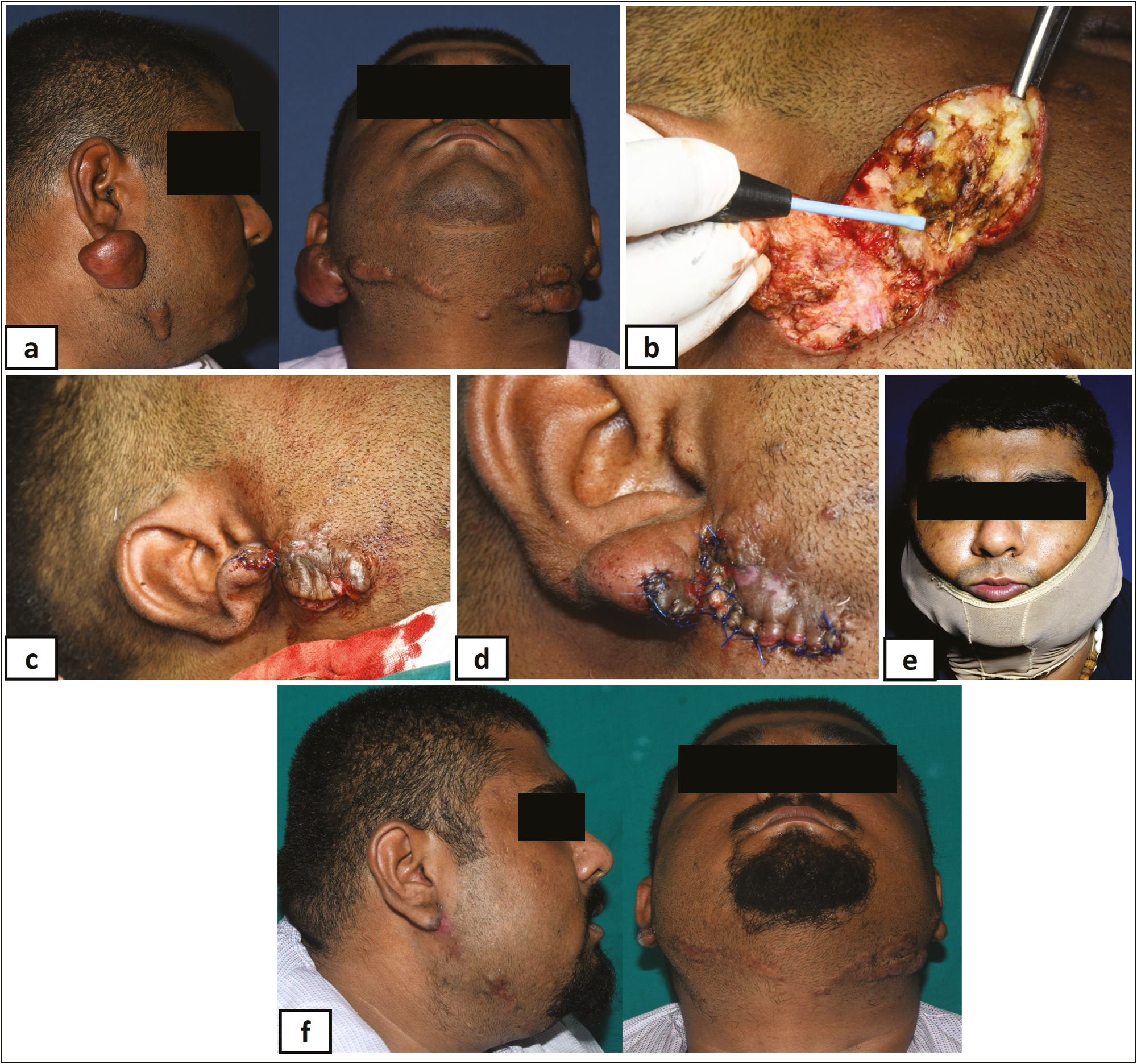
- (A) Bulky keloid on face, (B) debulking with radiofrequency, (C) after complete debulking—suturing, (D) after complete suturing, (E) compression with SGS, and (F) after complete healing
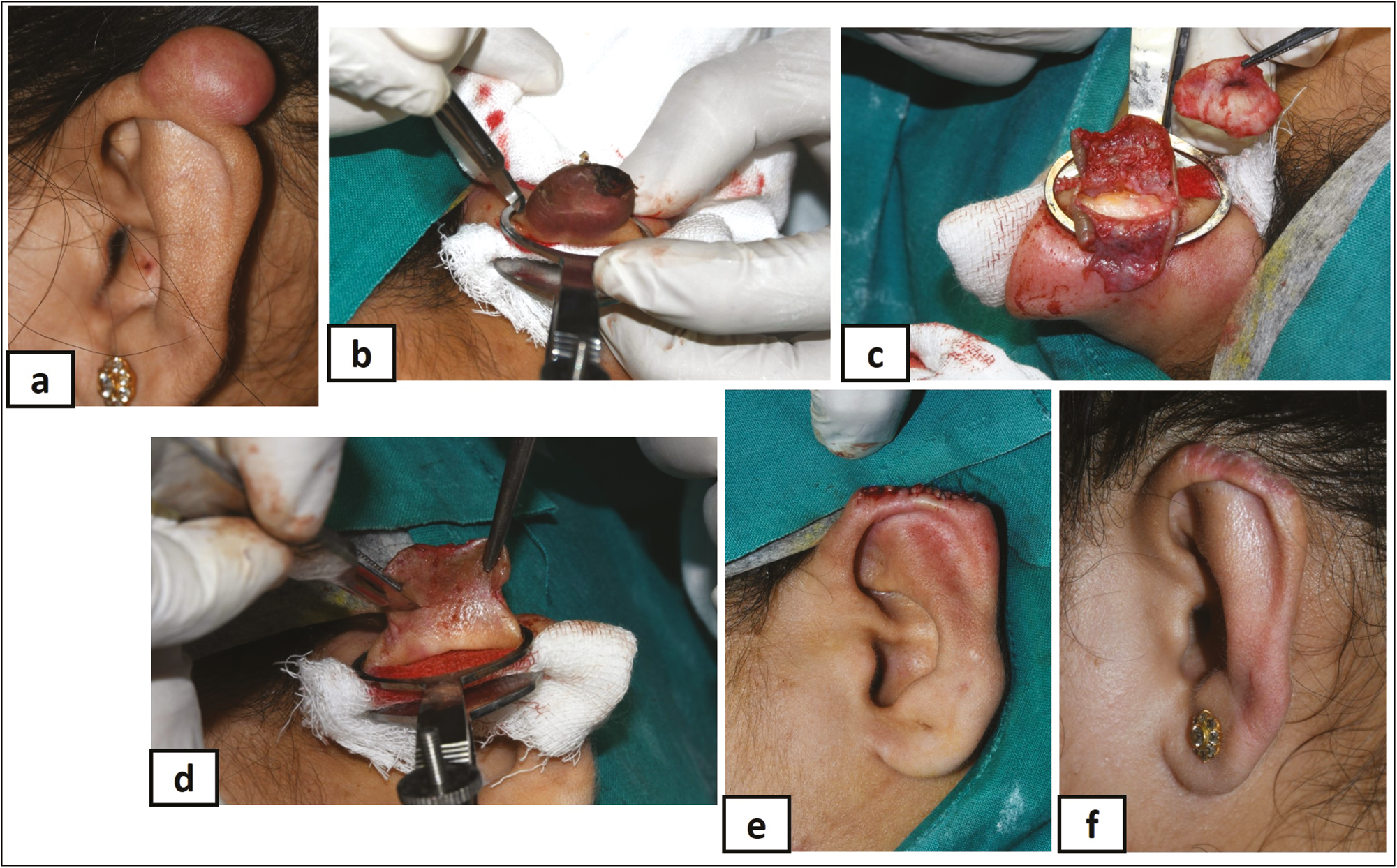
- (A) Nodular keloid over left auricle rim, (B) surgical excision, (C) complete debulking, (D) suturing the auto flap, (E) sutured flap immediate postoperative, and (F) complete healing
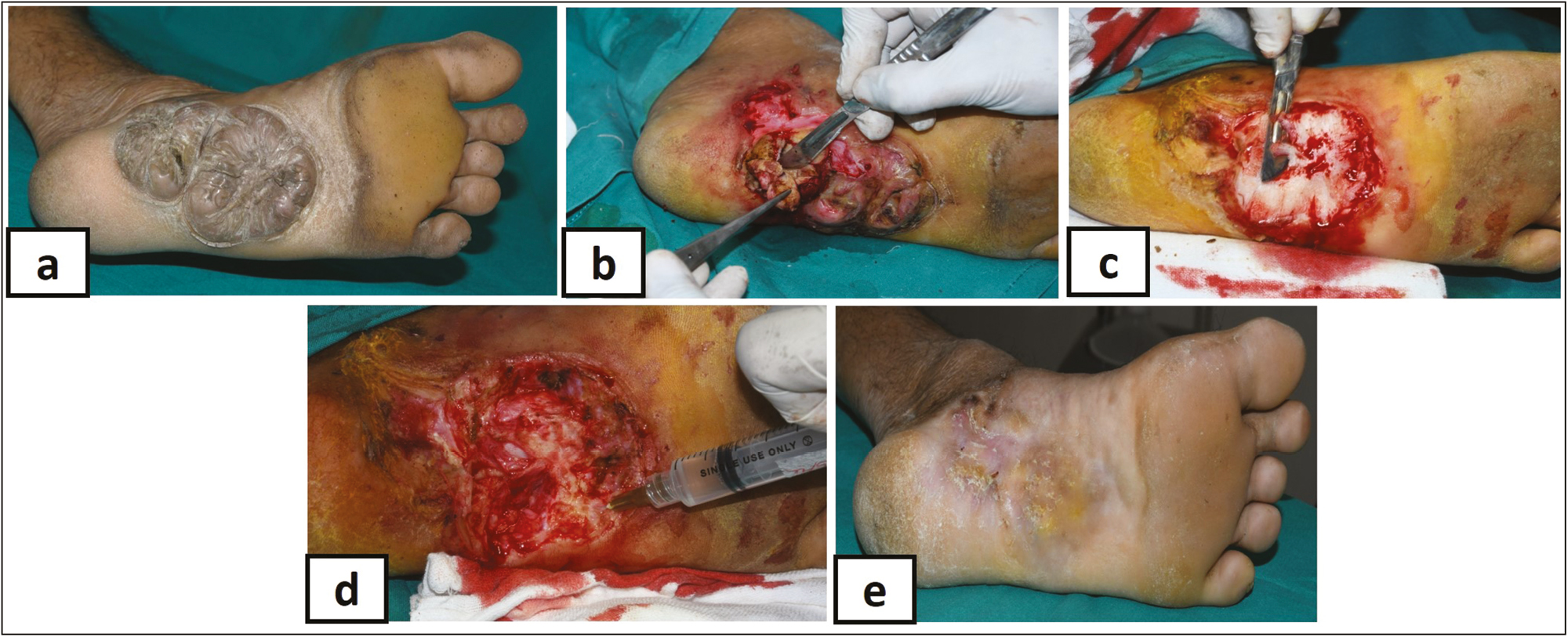
- (A) Bulky keloid on plantar aspect of foot, (B) debulking with scalpel, (C) complete debulking with scalpel, (D) intralesional (S + 5-FU), and (E) complete healing
DISCUSSION
Keloids pose a challenge as they have high recurrence rate and do not respond completely to any single treatment modality. Hence, surgical key for successful outcome is the sequential combination of multiple modalities after maximum debulking either by cryotherapy or surgical excision.[2,3,4,5,6,7,8,911,12,13] However, after extralesional surgical excision, most of the studies have reported a high recurrence rate of 80%–100%.[13] Lee et al.[7] devised intralesional autoflap surgery and reported no recurrence in 20 of 24 patients (90%). Various advantages have been proposed for reducing recurrence in support of intralesional as against extralesional surgical excision are: (a) it avoids injury to neighboring skin[15] and the deep dermal layers with subcutaneous fat,[16] (b) reduces the most proliferative central fibroblastic group,[17] (c) facilitates injecting intralesional corticosteroid,[15] and (d) provides protective action by retaining the keloidal rim.[18] By contrast, many studies are not in support of this as some amount of keloidal tissue (rim) is left behind, which can proliferate, so also keloid can arise from the extralesional peripheral areas and, thus, has reported high recurrence rate (45%).[1920] Hence, various adjuvant therapies have been suggested along with surgical excision. Auricular compression devices and intralesional TCA have been combined with surgical excision to successfully treat auricular keloids with reduced recurrence rate and improved scar quality.[21] There are other studies that have combined intralesional excision with multiple sessions of intralesional TCA (10–40 mg per session) and a recurrence rate of 0%–25% over a follow-up of 9–36 months.[1113,18,19,20] In this study, after surgical excision, IL (S + 5-FU) was given intra- and postoperatively, followed by the use of SGS under compression to achieve complete regression in 9 of 10 patients (90%).
Standard LN2 cryotherapy either intralesional or surface (spray/probe) achieves rapid debulking of large bulky/flat keloids.[1,2,3,4,5,68,911,12] However, following both these techniques, there are tissue necrosis, ulceration with surface destruction, delayed wound healing, pigmentary changes (hypo/hyper/depigmentation), atrophy, scarring, and recurrence.[1,2,3,4,5,68,911,1222] As against standard intralesional cryotherapy,[89,22] where the LN2 is used to freeze the lesion completely from inside (core) out to destroy it along with surface skin, in this study, two freeze-thaw cycles were carried out to achieve debulking with minimal damage to the overlying surface skin at the entry and exit points of the needle only. Similarly, as against standard surface cryotherapy,[1,2,3,4,5,611,12] where the LN2 is used to freeze the lesion from outside either by spray or probe to destroy it along with surface skin, in this study, metallic rollers were used to cause shallow cryoinjury to achieve debulking without damaging the surface skin. The results of the most of the intralesional cryotherapy studies reported mean volume reduction ranging from 51.4% to 63% (range: 16%–100%).[89] Stromps et al.[23] reported volume reduction of 89% for facial and 47% for presternal scars. Gupta and Kumar[22] reported more than 75% scar volume reduction in 7 of 12 patients. van Leeuwen et al.[8] in addition reported 58.5% mean scar surface area reduction. Most of this reduction occurred after single treatment in 3–4 months. Most studies evaluated the results after single cryo session, whereas some used up to 10 sessions.[89] In this study, more than 75–100 scar volume reduction was achieved in 11 patients with one or both methods of cryotherapy in 4–6 sessions. Cryotherapy, when used alone, has shown variable recurrence rate; hence, it has been combined with TCA with or without 5-fluorouracil, SGS, compression therapy, etc. to successfully reduce the recurrence rate by many authors.[1,2,3,4,5,610,1113,14,15,1820,2123,24] Boutli-Kasapidou et al.[25] reported complete recovery in 87% using cryosurgery and intralesional corticosteroids. Weshahy and Abdel Hay[26] used the combination of intralesional cryotherapy and intralesional corticosteroid injections in 22 of 25 cases with 93% mean volume reduction after 4 months (P < 0.001). Stromp et al.[23] as mentioned earlier used SGS as an adjuvant to intralesional cryotherapy and achieved good results in 21 of 32 (89%) cases. In this study, after cryotherapy, ILS + 5-FU injection was given intra- and postoperatively followed by SGS under compression to achieve complete regression in 10 of 11 patients (90.9%).
Response of keloids to corticosteroid injection alone is reported to be variable with 70%–90% regression rate and with 33%–50% recurrence rate after 1 and 5 years.[14] The combination of TCA with 5-FU has been reported to be more effective with less side effects and better patient satisfaction.[2,3,4,5,6] Darougheh et al.[10] in a double-blind study of 40 patients reported more than 50% improvement in 55% of cases treated with TCA and 5-FU as against only 20% of cases treated with TCA alone. Khan et al.[27] compared the use of intralesional TCA alone and its combination with 5-fluorouracil and found that the combination was superior to TCA alone in achieving faster response with fewer side effects. The intralesional 5-fluorouracil (50 mg/mL 2–3 times a week) shrinks keloid safely while avoiding the side effects of repeated corticosteroid injections such as tissue atrophy and telangiectasia.[28] Corticosteroids and fluorouracil when combined, complement each other by diminishing the adverse effect of each other such as menstrual irregularity (corticosteroids), ulceration (5-fluorouracil) as fewer treatment sessions are required to achieve favorable outcome, thus increasing the patient compliance.[2728] In this study, the combination of intralesional injection of short-acting (hydrocortisone) and long-acting (TCA) corticosteroids along with injection 5-fluorouracil was used intra- and postoperatively, which gave immediate symptomatic (pain and itching) relief with volume/surface reduction that was sustained over next 4–6 weeks. In this study, no adverse effects of corticosteroids or 5-fluorouracil were observed in any of the patients, fewer numbers of sessions were required to achieve volume reduction with flattening, and there was good patient compliance with recurrence in only 2 of 21 cases (9.1%).
Most of the standard (intralesional/superficial), cryotherapy studies reported mild-to-moderate postoperative pain with local edema and superficial necrosis in the first few weeks followed by postoperative pigmentation (de/hypo/hyper) in majority of the cases; which improves over a period in most of them.[1,2,3,4,5,68,912,1322] Two meta-analysis studies on intralesional cryotherapy reported that hypopigmentation persisted permanently in 30%–35% of patients.[89] One study reported wound infection in 7.5% of cases, which improved after conservative treatment.[8] In this study, minimal postoperative pain and edema occurred in all the patients who were successfully treated with anti-inflammatory and analgesic drugs. Secondary infection was reported in two patients, which was successfully controlled with additional course of antibiotics. There were transient postoperative pigmentary (de/hypo/hyper) changes, which gradually subsided and disappeared over the next 6–9 months in all 10 of 11 patients (90.9%) treated with cryotherapy. However, postinflammatory hypopigmentation persisted in one patient even after a follow-up of 2.5 years. The recurrence rate in most of the studies ranged from 0% to 24% with a mean of 7.6%% ± 10.1%.[8] One study reported recurrence at the periphery (0.5–1 cm3) in 12% of cases, which flattened after repeated intralesional steroid injections.[21] In this study, recurrence was noted in 2 of 21 patients (9.1%) in spite of combination treatment. One patient with large multifocal keloid on the plantar aspect (extralesional surgical excision) had recurrence 2 months after undergoing three sessions of extralesional excision at monthly interval and another with large bulky circumferential keloid near the elbow (intralesional and surface cryotherapy) had recurrence 1.5 months after six sessions of intralesional surface cryotherapy. This could have been due to incomplete removal or destruction of the active part of the keloidal lesion; both these patients were further subjected to similar sessions of treatment as mentioned above, and SGS under compression was continued for prolonged time even after flattening of the keloid (4–6 months) to achieve complete clearance without any further recurrence on follow-up of 2½ years. Patients with multifocal keloids healed with atrophic scarring and postinflammatory hyperpigmentation due to multiple sessions of extralesional surgical excision. Thus, this study brings out the importance of individualized multimodal approach for successfully treating keloids. However, the study is limited by a single-center study design with a relatively small sample size.
All in all, this study concludes that a long-term multimodal approach comprising of IL (S + 5-FU) injection followed by SGS under compression after the initial debulking by either surgical excision or LN2 cryotherapy as per the individual lesions was found to be highly effective and safe in treating small nodular/pedunculated to large bulky/flat keloids of variable size, number, or anatomical location. There was also a reduction in volume and recurrence rate with less complications and complete regression with flattening effect. The modified cryotherapy adopted in this study minimized surface damage, thus achieving favorable aesthetic and functional outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
REFERENCES
- Keloids and hypertrophic scars: Review and treatment strategies. Semin Cutan Med Surg. 1999;18:159-71.
- [Google Scholar]
- Hypertrophic scars and keloids: Etiology and management. Am J Clin Dermatol. 2003;4:235-43.
- [Google Scholar]
- Textbook of dermatosurgery and cosmetology. Indian J Dermatol Venereol Leprol. 2005;71:307.
- [Google Scholar]
- Hypertrophic scars and keloids: A review and current treatment modalities. Biomed Dermatol. 2020;4:11.
- [Google Scholar]
- Up-to-date approach to manage keloids and hypertrophic scars: A useful guide. Burns. 2014;40:1255-66.
- [Google Scholar]
- A new surgical treatment of keloid: Keloid core excision. Ann Plast Surg. 2001;46:135-40.
- [Google Scholar]
- Intralesional cryotherapy for the treatment of keloid scars: Evaluating effectiveness. Plast Reconstr Surg Glob Open. 2015;3:e437.
- [Google Scholar]
- Intralesional cryotherapy for hypertrophic scars and keloids: A review. Scars Burn Heal. 2017;3:2059513117702162.
- [Google Scholar]
- Intralesional triamcinolone alone or in combination with 5‐fluorouracil for the treatment of keloid and hypertrophic scars. Clin Exp Dermatol. 2009;34:219-23.
- [Google Scholar]
- A review of current keloid management: Mainstay monotherapies and emerging approaches. Dermatol Ther. 2020;10:931-48.
- [Google Scholar]
- Use of cryotherapy in the treatment of keloids. J Dermatol Surg Oncol. 1993;19:529-34.
- [Google Scholar]
- The most current algorithms for the treatment and prevention of hypertrophic scars and keloids. Plast Reconstr Surg. 2010;125:557-68.
- [Google Scholar]
- Triamcinolone acetonide intralesional injection for the treatment of keloid scars: Patient selection and perspectives. Clin Cosmet Investig Dermatol. 2018;387:96.
- [Google Scholar]
- Head and neck keloid: Treatment by core excision and delayed intralesional injection of steroid. J Oral Maxillofac Surg. 2007;65:1292-6.
- [Google Scholar]
- Control of wound healing and scar formation in surgical patients. Arch Surg. 1981;116:1325-9.
- [Google Scholar]
- Abnormal balance between proliferation and apoptotic cell death in fibroblasts derived from keloid lesions. Plast Reconstr Surg. 2001;107:87-96.
- [Google Scholar]
- The influence of surgical excision margins on keloid prognosis. Ann Plast Surg. 2010;64:55-8.
- [Google Scholar]
- Intralesional excision as a surgical strategy to manage keloid scars: What’s the evidence? Scars Burn Heal. 2019;5:2059513119867297.
- [Google Scholar]
- Assesment of the treatment of earlobe keloids with triamcinolone injections, surgical resection, and local pressure. Rev Col Bras Cir. 2015;42:09-13.
- [Google Scholar]
- Intralesional cryosurgery using lumbar puncture and/or hypodermic needles for large, bulky, recalcitrant keloids. Int J Dermatol. 2001;40:349-53.
- [Google Scholar]
- Intralesional cryosurgery combined with topical silicone gel sheeting for the treatment of refractory keloids. Dermatol Surg. 2014;40:996-1003.
- [Google Scholar]
- International Advisory Panel on Scar Management Updated international clinical recommendations on scar management: Part 2–Algorithms for scar prevention and treatment. Dermatol Surg. 2014;40:825-31.
- [Google Scholar]
- Hypertrophic and keloidal scars: An approach to polytherapy. Int J Dermatol. 2005;44:324-7.
- [Google Scholar]
- Intralesional cryosurgery and intralesional steroid injection: A good combination therapy for treatment of keloids and hypertrophic scars. Dermatol Ther. 2012;25:273-6.
- [Google Scholar]
- Intralesional triamcinolone alone and in combination with 5-fluorouracil for the treatment of keloid and hypertrophic scars. J Pak Med Assoc. 2014;64:1003-7.
- [Google Scholar]
- Treatment of inflamed hypertrophic scars using intralesional 5-FU. Dermatol Surg. 1999;25:224-32.
- [Google Scholar]






