Translate this page into:
Elliptical excision and primary closure of nasal defect to achieve best esthetic outcome: A case series of 50 patients
*Corresponding author: Yogesh M. Bhingradia, Department of Dermatology, Venereology and Leprosy, Shivani Skin Care and Cosmetic Clinic, Surat, Gujarat, India. yogeshbhingradia@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhingradia YM, Yadav C, Salunke TS. Elliptical excision and primary closure of nasal defect to achieve best esthetic outcome: A case series of 50 patients. J Cutan Aesthet Surg. 2024;17:234-8. doi: 10.25259/jcas_120_23
Abstract
Objectives:
To evaluate the cosmetic result of nasal of an elliptical excision and primary closure on small nasal defect by using Scar assessment using the Stony Brook Scar Evaluation Scale (SBSES) score.
Material and Methods:
This retrospective interventional study was conducted in a private clinic over a 2-year duration. Patients aged 18–60 years with nasal defects <1.5 cm were enrolled after obtaining informed consent. Exclusion criteria included immunocompromised status, keloidal tendency, local site infection, bleeding disorder, age <18 years, and lack of consent. Scar assessment using the SBSES was performed at the end of 6 months. Statistical analysis included summary statistics, analysis of variance tests, and a significance level of P < 0.05.
Results:
The study included 50 patients, with 54% males and 46% females. The most common age group was 21–40 years, and melanocytic nevi was the most common cause for excision. Lesions were excised mainly from the lateral wall and dorsum of the nose. The mean SBSES score was 3.79 ± 0.467. The best cosmetic outcome was observed in lesions involving the dorsum followed by the root of the nose. No significant difference was found among the SBSES scores for various subunits.
Conclusion:
Elliptical excision with primary closure is a simple and effective technique for small nasal defects, providing good cosmetic results. The location of the nasal defect influences the cosmetic outcome, with better results observed in areas with thinner skin and increased skin laxity.
Keywords
Nasal defect
Elliptical excision
SBSES score
INTRODUCTION
The nose plays a significant role in facial esthetics and overall appearance. It greatly influences the facial balance and the overall attractiveness of a person. In the past decade, there has been an increasing demand for corrections of nasal imperfections and to improve the visual appeal.1 Nose is also an equally challenging site owing to its complex contour, uneven skin thickness, lack of skin elasticity, and various topographic subunits.2
For moderate to large nasal defects, various surgical methods such as flaps and grafts are generally used.3 For small nasal defects (1.5 cm), fusiform elliptical excision is an excellent tool for obtaining optimal esthetic outcomes.4 It minimizes tissue removal, skin movement, and incision length.
There are many scales or scoring systems to quantify the appearance of scars. There are mainly five subjective scar assessment scales: Vancouver scar scale, Manchester scar scale, patient and observer scar assessment scale, visual analog scale, and Stony Brook Scar Evaluation Scale (SBSES). SBSES is a 6-item ordinal wound evaluation scale initially developed to measure short-term cosmetic outcomes, now being used for long-term assessment as well.5
This study aims to observe the final cosmetic result of elliptical excision of the nasal defect using the SBSES scale.
Aims and objectives
This study aimed to use SBSES to evaluate the cosmetic results of an elliptical excision and primary closure on small nasal defects.
MATERIAL AND METHODS
It was a retrospective interventional study conducted in a private clinic over 2 years. Patient between 18 and 60 years of age, irrespective of gender having lesions on the nose <1.5 cm were enrolled in the study after their informed consent.
Immunocompromised patients, patients with keloidal tendency, local site infection, bleeding disorder, age <18 years and patients who did not give consent were excluded from the study.
A detailed history was recorded and clinical photographs were taken for each patient. Patients were subjected to baseline investigations and were then opted for surgery.
Procedure
The patient was enrolled after fulfilling the inclusion criteria and by obtaining their informed consent.
The lesion site and size were noted and a clinical photograph taken.
The surgical site was cleaned after maintaining aseptic precaution.
The classic ellipse is traced with the help of a skin marker. The width-length ratio is 1:3–1:4 and the elliptical angle is 30. Case-specific refinement was done to increase the cosmetic outcome.
With the help of surgical blade no. 15, the skin was excised in a single stroke to avoid overlapping. The wound closure was done by subcuticular buried 6–0 polyamide black suture followed by a superficial vertical mattress using 6–0 polyamide black.
Follow-up
Suture removal was done on the seventh day after surgery. The patient was followed up monthly and at the end of 6 months, scar assessment was done by the SBSES. A standardized photograph of the evaluated scar was taken with a digital camera at the highest image resolution and held at 3 feet from the subject. It was then sent to another physician for independent assessment. The SBSES score ranges from 0 (worst scar) to 5 (best scar). The evaluation scale is detailed in Table 1. The total score of each patient is tabulated on Microsoft Excel and mean ± standard deviation (SD) is calculated.
Statistical analysis
Summary statistics were applied for basic demographic data and clinical characteristics of the patient. Analysis of variance test was used to compare the mean of SBSES between various groups. P = 0.05 was accepted as statistically significant.
In SBSES, the range varies from 0 (worst) to 5 (best) [Table 1].
| Scar category | Points |
|---|---|
| Width | |
| >2 mm | 0 |
| <2 mm | 1 |
| Height | |
| Elevated/depressed concerning the surrounding skin. | 0 |
| Flat | 1 |
| Color | |
| Darker than the surrounding skin. | 0 |
| Same color or lighter than the surrounding skin. | 1 |
| Suture marks | |
| Present | 0 |
| Absent | 1 |
| Overall appearance | |
| Poor | 0 |
| Good | 1 |
RESULTS
Of the 50 patients studied, 27 (54%) were male and 23 (46%) were female. The most common age group was 21–40 years (46%) followed by 41–60 years (28%). The most common cause for the excision was melanocytic nevi (n = 23, 46%), followed by post-traumatic scar (n = 15, 30%). Table 2 provides patients clinical data. Lesions were excised mainly from the lateral wall (n = 15, 30%) followed by the dorsum of the nose (n = 14, 28%) [Table 3 and Figure 1a-c].
| Number | Percentage | |
|---|---|---|
| Sex | ||
| Male | 27 | 54 |
| Female | 23 | 46 |
| Age | ||
| <20 | 3 | 6 |
| 21–40 | 23 | 46 |
| 41–60 | 14 | 28 |
| Lesion on nose | 23 | 46 |
| Melanocytic nevi | 15 | 30 |
| Post-traumatic scar | 4 | 8 |
| Melanoma | 6 | 12 |
| Congenital melanocytic nevi | 1 | 2 |
| Fibrous papule | 1 | 2 |
| Site | Number | Percentage |
|---|---|---|
| Dorsum | 14 | 28 |
| Lateral wall | 15 | 30 |
| Root | 9 | 18 |
| Alae | 4 | 8 |
| Tip | 4 | 8 |
| Dorsum+lateral wall | 4 | 8 |

- (a) A hyperpigmented atrophic scar measuring 1.5 cm × 0.3 cm present on the lateral nasal wall. (b) The scar was then excised using elliptical excision. (c) After 6 months of the surgery, a linear light scar can be noticed with a stony brook scar evaluation scale of 5.
Post-procedure outcome was evaluated using SBSES at the end of 3 months, as shown in Table 4. The average mean of the score was calculated to be 3.79 with an SD of 4.67. The best cosmetic scar was seen in the lesion which involves the dorsum (4.28) [Figure 2a and b] followed by the root of the nose (4.1) [Figure 3a-d]. The lesion present on the alae (3) [Figure 4a and b] and the tip of the nose (3.5) [Figure 5a and b] had a less favorable outcome. This difference can be explained by the slight redundancy of the cutaneous tissue in the upper 2/3 of the nose.6,7 No significant difference was found among the SBES of various subunits [Table 5].
| Score | Number | Percentage |
|---|---|---|
| 5 | 20 | 40 |
| 4 | 17 | 34 |
| 3 | 8 | 16 |
| 2 | 2 | 4 |
| 1 | 3 | 6 |
| 0 | 0 | 0 |
| Site | 5 | 4 | 3 | 2 | 1 | 0 | Total | Average |
|---|---|---|---|---|---|---|---|---|
| Dorsum | 7 | 4 | 3 | 0 | 0 | 0 | 60 | 4.28 |
| Lateral wall | 6 | 5 | 2 | 2 | 0 | 0 | 38 | 3.86 |
| Root | 5 | 2 | 1 | 0 | 1 | 0 | 29 | 4.1 |
| Alae | 0 | 2 | 1 | 0 | 1 | 0 | 11 | 3 |
| Tip | 1 | 2 | 0 | 0 | 1 | 0 | 12 | 3.5 |
| Dorsum+lateral wall | 1 | 2 | 1 | 0 | 0 | 12 | 4 |
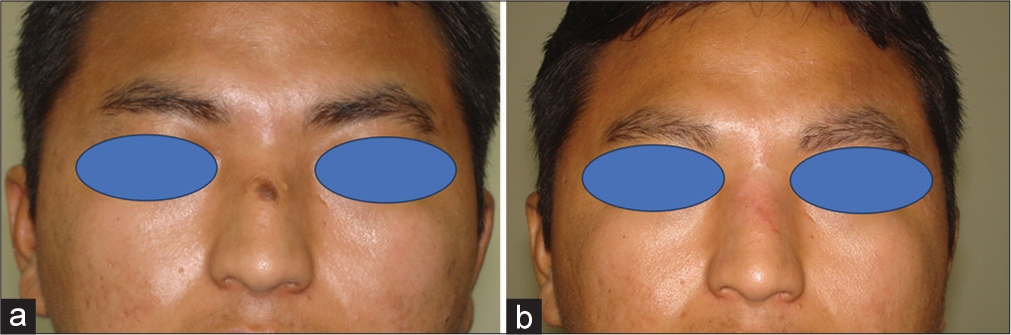
- (a) A singular melanocytic nevus measuring 0.5 cm × 0.5 cm present on the dorsum of the nose. (b) After 6 months, the patient has a thin linear erythematous scar, with a stony brook scar evaluation scale of 4.
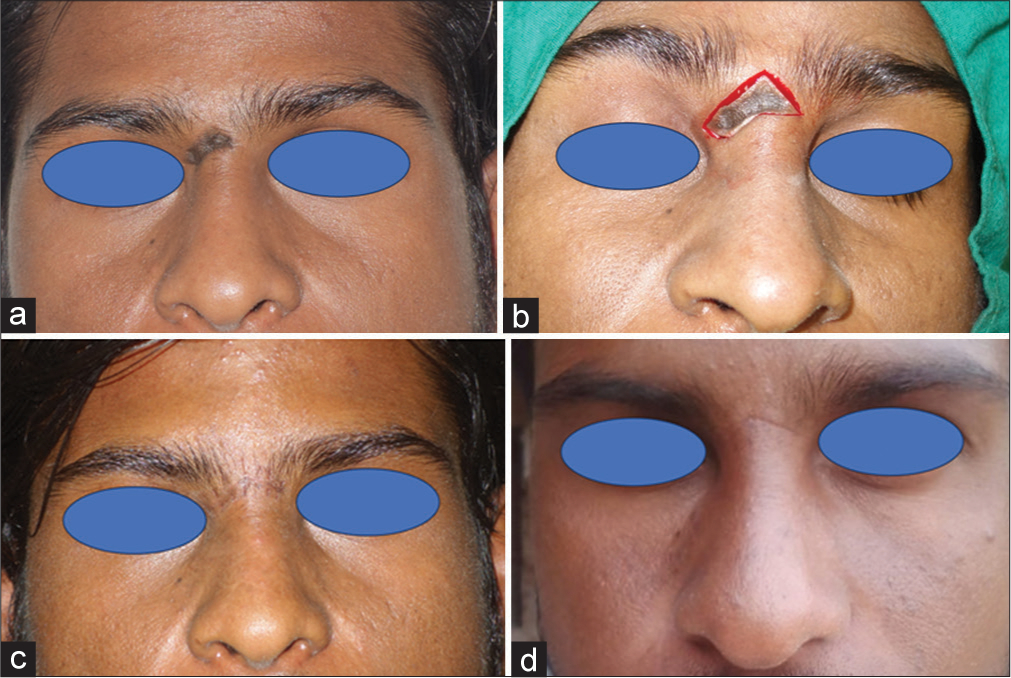
- (a) A single melanocytic nevus measuring 1.5 cm × 0.4 cm on the root of the nose. (b) The lesion was excised with modifications of classical elliptical excision. (c) One month post-surgery, a linear thin scar can be seen with suture marks. (d) After 6 months of surgery, a linear scar with no suture marks and normal skin, a stony brook scar evaluation scale of 5.
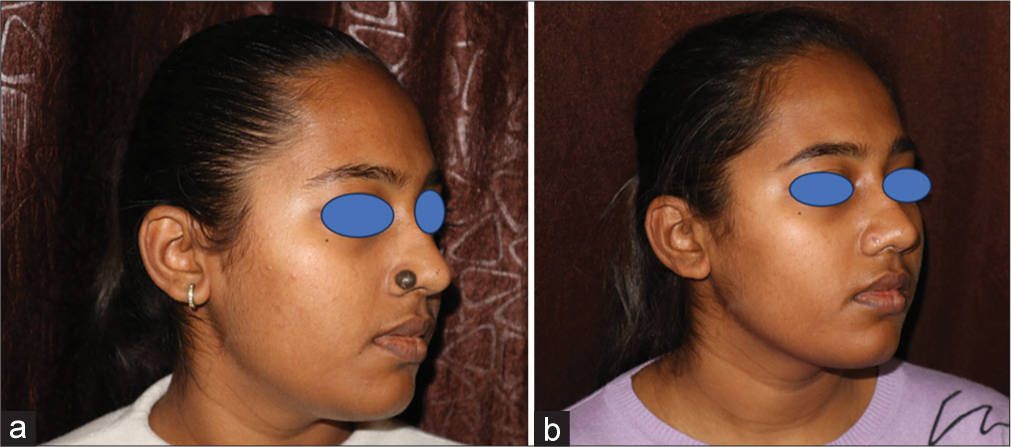
- (a) A singular melanocytic nevus measuring 1 cm diameter present on alae. (b) After 6 months of surgery, a hypertrophic scar with a width >2 mm had a stony brook scar evaluation scale score of 3.
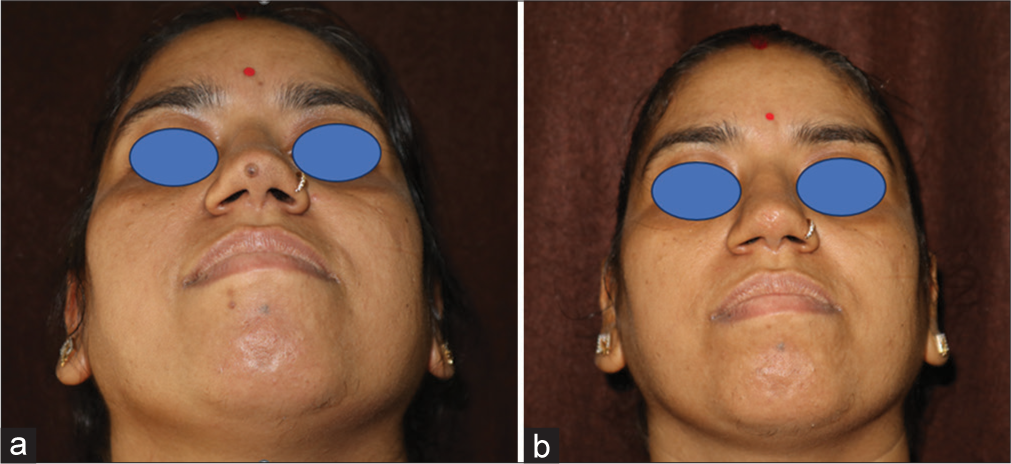
- (a) Singular melanocytic lesion on the tip of the nose measuring 0.5 cm in diameter. (b) A slightly depressed scar, 6 months after surgery with a stony brook scar evaluation scale score of 4.
DISCUSSION
The nose is divided into nine esthetic subunits including the tip subunit, columellar subunit, right and left alar base subunits, right and left alar side wall subunits, right and left dorsal side wall subunits, and dorsal subunit.6 These subunits were originally conceptualized to describe the perceived shapes of the nose based on the contour created by highlights and shadows. The subunit principle is based on reconstructing nasal defects by subunits for the optimum cosmetic outcome. It was originally proposed that if the defect is >50%, it is better to resect the whole subunit. This principle is not applicable to skin graft or flap and only applies to subunits having convex surfaces such as nasal tip and ala.8 Lesions having size <1.5 cm rarely involve more than 50% of a subunit and are also generally an exception of the subunit rule.9
There is a dearth of studies focusing on the management of small nasal lesions and not much is written on the approach for the management of these lesions. Their size is an advantage as all the techniques for the reconstruction including flap, graft, healing with secondary intention, and primary elliptical closure can be done but not all give the desired esthetic result. Healing with flaps includes a more invasive closure with an additional incision site, a takedown procedure several weeks later, and an unfavorable appearance while the primary flap is in place.10
Healing with secondary intention was not favored as the esthetic results are likely to be unacceptable if not done in the correct setting. They require weeks of careful wound care with chances of surgical site infection and scarring.9
In this study, we performed simple elliptical excision with primary closure in all of our patients having nasal defects <1.5 cm. There was no statistically significant difference among the cosmetic outcomes of surgical scars on different nasal subunits. The lesion present on the dorsum and on the root had a slightly better result than the lesion seen on the alae and lateral wall of the nose. This difference in scar appearance can be attributed to the skin quality and shape of the particular subunit. The skin on the nasal tip, nasal alae, and cranium dorsum is thicker with more pilosebaceous units and more adherent to the underlying structure. These characteristic increases tension on the suture line and risk distortion of the subunit.8 The skin on the proximal subunit of the nose is thinner with more skin laxity, leading to a better cosmetic result.7
Elliptical excision is a common technique used by dermatologists; however, it is often overlooked in the nose in favor of more technologically demanding methods such as flap or graft. This is in part due to the paucity of skin laxity on the face and the risk of subunit distortion.4 However, studies have shown that for small (<1 cm) to medium-sized defects (1–1.5 cm) linear closure delivers a more cosmetic and functional result than flap/graft.11 Elliptical excision and its variation are easily adaptable to the contour of the nose resulting in a scar that can be easily hidden along a relaxed skin tension line.12
Reducing tractional force over the cutaneous sutures is crucial for improving the appearance of the scar, and this is accomplished by closing the subcutaneous incision with non-absorbable (polyamide black) buried interrupted suture (6–0) and closing the cutaneous wound with non-absorbable suture in a vertical mattress pattern.13
The final esthetic outcome of the scar is one of the most important outcomes for both the dermatosurgeon and the patient. Scar evaluation scales are developed to evaluate wound outcomes after surgery. SBSES is a newer scale of five dichotomous, evenly weighted categories. It has a good inter-observer agreement and a high correlation with the visual analog scale.14 In our study, the mean SBSES was 3.79 ± 0.467, with the dorsum of the nose having the highest score (4.28). This outcome was consistent with a study that gave a score of 4.108 for the dorsal scar following wide open dorsal approach rhinoplasty.15
CONCLUSION
The study emphasizes the importance of scar evaluation and provides valuable insights for dermatosurgeons in selecting appropriate techniques for nasal defect correction. Before going on to a more technical, challenging operation such as a flap/graft and elliptical excision with primary skin closure is a good and simple technique for small nasal defects giving good cosmetic results.
Authors’ Contributions
All the authors contributed to the research study. Yogesh M. Bhingradia: data acquisition, experimental study, manuscript review. Chinmai Yadav: data analysis, manuscript preparation. Tejaswini S. Salunke: Data Analysis, manuscript editing.
Ethical approval
Institutional Review Board approval is not required as it is a retrospective study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Minimally invasive procedures for nasal aesthetics. J Cutan Aesthet Surg. 2012;5:115-20.
- [CrossRef] [PubMed] [Google Scholar]
- The subunit principle in nasal reconstruction. Plast Reconstr Surg. 1985;76:239-47.
- [CrossRef] [PubMed] [Google Scholar]
- Nasal reconstruction: An overview and nuances. Semin Plast Surg. 2008;22:257-68.
- [CrossRef] [PubMed] [Google Scholar]
- Reconstruction of small soft tissue nasal defects. Semin Plast Surg. 2013;27:110-6.
- [CrossRef] [PubMed] [Google Scholar]
- Development and validation of a novel scar evaluation scale. Plast Reconstr Surg. 2007;120:1892-7.
- [CrossRef] [PubMed] [Google Scholar]
- Use of keystone flaps in consideration of the facial aesthetic subunit concept as an alternative reconstructive option for nasal defect coverage. J Craniofac Surg. 2021;32:1864-9.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous reconstruction of the nasal distal third: Alternative local flaps for a complex region. Plast Reconstr Surg Glob Open. 2021;9:e3444.
- [CrossRef] [PubMed] [Google Scholar]
- Reconstruction of nasal defects: Contemporary approaches. Curr Opin Otolaryngol Head Neck Surg. 2016;24:453-60.
- [CrossRef] [PubMed] [Google Scholar]
- Reconstruction of the nose: Management of nasal cutaneous defects according to aesthetic subunit and defect size. A review. Medicina (Kaunas). 2020;56:639.
- [CrossRef] [PubMed] [Google Scholar]
- Linear closure of surgical defects on the nose after intraoperative tissue relaxation as an alternative to a skin flap or graft. JAAD Case Rep. 2020;6:679-82.
- [CrossRef] [PubMed] [Google Scholar]
- Linear closure for nasal defects after Mohs micrographic surgery. J Drugs Dermatol. 2009;8:23-8.
- [Google Scholar]
- Elliptical excisions: Variations and the eccentric parallelogram. Arch Dermatol. 2004;140:176-80.
- [CrossRef] [Google Scholar]
- Utilization of nonabsorbable (polyamide black) buried subcutaneous suture material in closure of elliptical excision in various indications for better aesthetic outcome. J Cutan Aesthet Surg. 2021;14:215-9.
- [CrossRef] [PubMed] [Google Scholar]
- How to assess postsurgical scars: A review of outcome measures. Disabil Rehabil. 2009;31:2055-63.
- [CrossRef] [PubMed] [Google Scholar]
- Wide-open dorsal approach rhinoplasty for droopy noses. Aesthetic Plast Surg. 2015;39:25-35.
- [CrossRef] [PubMed] [Google Scholar]







