Malignant proliferating trichilemmal tumor in male: A rare case entity with diagnostic dilemma
*Corresponding author: Avishek Koley, Department Of General Surgery, GSVM Medical College, Kanpur, India. avish5407@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Yadav GD, Shanker P, Singh S, Koley A. Malignant proliferating trichilemmal tumor in male: A rare case entity with diagnostic dilemma. J Cutan Aesthet Surg. doi: 10.4103/JCAS.JCAS_90_23
Abstract
Trichilemmal tumor is a rare hair follicle tumor that is thought to occur from a malignant transformation of a benign trichilemmoma. The tumor develops from the outer root sheath of the hair follicle. The patient underwent a wide local excision with 1 cm clear margin. The defect was covered by a split thick skin graft harvested from the ipsilateral thigh after consulting the plastic surgery department. Trichilemmal cyst can be misdiagnosed as other cutaneous lesions. Like in our case, initial fine needle aspiration cytology (FNAC) was suggestive of an epidermoid cyst but post excision Histopathological examination gave us the real picture of a trichilemmal tumor. Recurrent tumors are very rare and can get misdiagnosed as squamous cell carcinoma. Malignant proliferating trichilemmal tumors (MPTTs) are rare cutaneous tumors that are very rare in males. These tumors can be misdiagnosed as squamous cell carcinoma and require external stimuli for malignant conversion from benign counterparts. Wide local excision is sufficient for treatment.
Keywords
Case report
Cutaneous tumor
Malignant
Rare
Trichilemmal cyst
INTRODUCTION
A proliferating trichilemmal cyst is a keratin-filled lesion that derives from the outer hair root sheath. Usually, proliferating trichilemmal cysts are benign, although rarely, can undergo malignant transformation, at which point they are referred to as malignant proliferating trichilemmal tumors (MPTTs).1
Trichilemmal tumor is a rare hair follicle tumor that is thought to occur from a malignant transformation of a benign trichilemmoma. The tumor develops from the outer root sheath of the hair follicle. It is most often found in areas that are exposed to the sun, particularly on the face and ears of elderly women. Trichilemmal carcinoma is considered to have low metastatic potential, meaning it is a low-grade carcinoma that rarely spreads to other parts of the body.2
Trichilemmal carcinoma is rare and its presentation is similar to other skin tumors, diagnosis is based on the presence of certain features on histological examination of a skin biopsy.
Trichilemmal carcinoma should be differentiated from other skin tumors, such as squamous cell carcinoma and basal cell carcinoma, which are more common.
CASE REPORT
A 50-year-old male patient came to our side with a chief complaint of swelling over the right occipital region of the scalp since birth with no other complaint. A workup was done and non-contrast computed tomography head (NCCT HEAD) showed no intracranial connection fine needle aspiration cytology (FNAC) suggested an epidermoid cyst. The cyst was excised in daycare surgery and sent for histopathological examination. The histopathological examination of the cyst was revealed to be MPTT.
The patient had ulcero-proliferative growth at the site of the excised cyst after 1 month of surgical excision. The growth of diameter was roughly around 5 cm with irregular margins which were grayish and tan-yellow in color with ulcerated surface, firm in consistency, bled on touch, and non-fixity to underlying cranial bone [Figure 1].

- Ulcero-proliferative growth seen at site of excision of previous cyst.
The patient underwent a wide local excision with 1 cm clear margin. The defect was covered by a split thick skin graft harvested from the ipsilateral thigh after consulting the plastic surgery department.
Methods
After obtaining the informed written consent and pre-procedural photographs for record, the patient was prepared for surgical excision keeping all aseptic precautions in mind. The patient was given general anesthesia after a proper preanesthetic check up. The site was draped with a sterile sheet and thoroughly cleaned it with spirit, betadine, and normal saline. Marking was done by taking 1 cm margin around the tumor. Wide local excision was done by using blade no. 15, and was hemostasis achieved by bipolar cautery [Figure 2]. The exposed raw area of the scalp was covered by split thick skin graft harvested from the ipsilateral thigh. The graft was fixed by the skin stapler. Aseptic dressing was done [Figure 3]. The histopathological examination of the lesion was revealed to be MPTT [Figure 4]. The patient was regularly followed up with no complications.

- Raw area after wide local excision.

- Post split thick skin grafting.
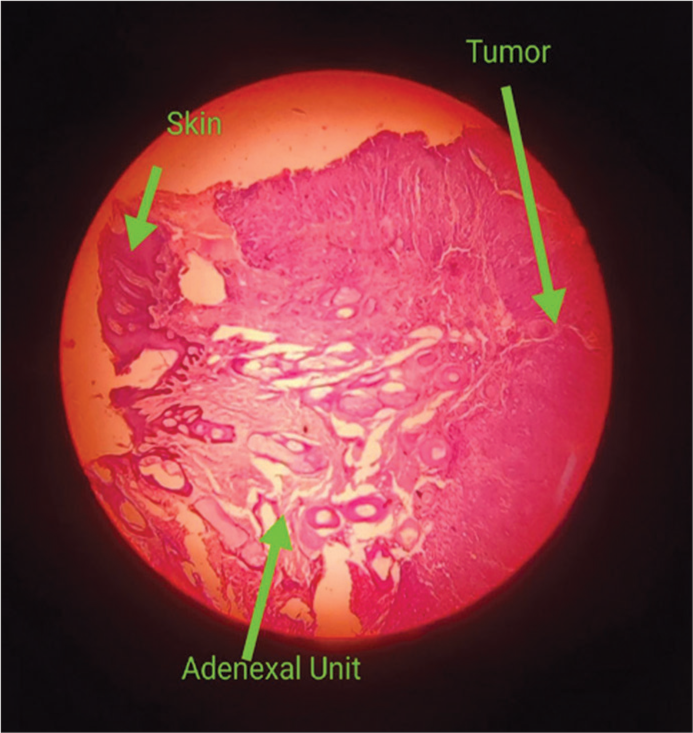
- Histopathological image showing skin adnexal unit and tumor.
DISCUSSION
Trichilemmal tumors are usually slow growing when benign but become locally aggressive when malignant transformation occurs after some external stimuli are applied. In our case, a previous surgery gave a stimulus for malignant conversion of a benign cyst.
Trichilemmal carcinoma should be differentiated from other skin tumors, such as squamous cell carcinoma and basal cell carcinoma, which are more common.
Trichilemmal cyst can be misdiagnosed as other cutaneous nous lesions. Like in our case, Initial FNAC was suggestive of epidermoid cyst but post excision Histopathological examination gave us the real picture of trichilemmal tumor. Recurrent tumors are very rare and can get misdiagnosed as squamous cell carcinoma. These tumors should therefore be thoroughly examined and newer modalities for differentiation from other skin tumors should be sought as immunohistochemistry. As of now, immunohistochemistry tests are financially burdening and patients from economically backward classes avoid them.3
These tumors are rare overall and usually seen in females. In this scenario, we are seeing such a tumor in a male patient.
Wide local excision is the treatment of choice for malignant trichilemmal tumors without any chemotherapy but metastatic disease may require postoperative chemotherapy as seen in squamous cell carcinoma.4
CONCLUSION
MPTTs are rare cutaneous tumors which are very rare in males. These tumors can be misdiagnosed as squamous cell carcinoma and require external stimuli for malignant conversion from benign counterparts. Wide local excision is sufficient for treatment.
Authors’ contributions
All the authors contributed to the research study. Gulab D. Yadav: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Prem Shanker: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Shubham Singh: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Avishek Koley: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has given his consent for his images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Malignant proliferating trichilemmal cyst: A case report with review of literature. Malays J Pathol. 2009;31:71-6.
- [Google Scholar]
- Proliferating trichilemmal tumors: Clinicopathologic evaluation is a guide to biologic behavior. J Cutan Pathol. 2003;30:492-8.
- [CrossRef] [PubMed] [Google Scholar]
- Management of trichilemmal carcinoma: An update and comprehensive review of the literature. Dermatol Surg. 2014;40:711-7.
- [Google Scholar]
- Tricholemmal carcinoma. A clinicopathologic study of 13 cases. Am J Dermatopathol. 1994;16:463-73.
- [CrossRef] [PubMed] [Google Scholar]






