Translate this page into:
Giant neglected unresectable ulcerated basal cell carcinoma of face: Radiotherapy at rescue
*Corresponding author: Suman Patra, Department of Dermatology, Venereology and Leprology, All India Institute of Medical Sciences (AIIMS), Jodhpur, Rajasthan, India. patrohere@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar S, Patra S, Devnani B, Rajagopalan V, Kaur M. Giant neglected unresectable ulcerated basal cell carcinoma of face: Radiotherapy at rescue. J Cutan Aesthet Surg. doi: 10.4103/JCAS.JCAS_62_23
Abstract
Basal cell carcinomas (BCCs) are typically considered indolent and slowly progressing tumors, but giant basal cell carcinomas are more aggressive with more risk of invasion and poor prognosis. Management of such giant BCCs (GBCCs) is difficult due to difficulty in surgical approach. We hereby report a case of giant ulcerated BCC of face treated with radiotherapy as a rescue treatment.
Keywords
Head and neck
Giant basal cell carcinoma
Radiotherapy
INTRODUCTION
Basal cell carcinomas (BCCs) are typically considered indolent, slowly progressing tumors. Giant BCCs (GBCCs), classified as greater than 5 cm in diameter, are considered more aggressive in behavior, with local tissue invasion and poor prognosis.1 They also have a higher mitotic rate and increased perineural invasion compared with conventional BCCs and are reported to be associated with patient neglect, low socioeconomic status, and immunosuppression.1 Management of such lesions is always difficult due to the difficulty in the surgical approach. We report a case of giant ulcerated BCC of the face near the outer canthus of the left eye successfully treated with radiotherapy.
CASE REPORT
A 71-year-old male, farmer by occupation, visited the dermatology outpatient department of AIIMS Jodhpur with the complaint of a large malodorous, painless ulcer near the left eye for 10–12 years. It started as a single pea size raised lesion over the lateral aspect of the left eye. It gradually progressed in size and later got ulcerated. Examination revealed, a single well-defined, malodorous, ulcer of size 6 cm × 5 cm, with rolled out margin [Figure 1]. The margin of the lesion was indurated, the surface showing hemorrhage, and purulent discharge at places. The left eye was completely replaced by the ulcerated plaque and multiple maggots were seen coming out of it. Owing to the large size of the lesion, it was not amenable to surgical options. The lesion was progressive and the ulcer over the left eyelid has associated myiasis. The lesion was initially managed with mechanical removal of maggots and oral antibiotics. He was planned for localized radiotherapy. He was treated with electron beam radiotherapy 60 Gy in 30 fractions over the left side of the face and forehead, 5 fractions weekly for 6 weeks with excellent response in terms of complete healing of the ulcer [Figure 2a and b]. Few residual lesions over the left ear and nasal bridge were treated with topical imiquimod. At 6 months follow-up [Figure 3], there was no recurrence over the treated sites.

- Large ulcer over left half of face extending from nose to left pinna including left eye with destruction of eye, yellow necrotic slough, hemorrhage over floor and rolled out margins, smaller ulcerated plaques over the right side of cheek and forehead.
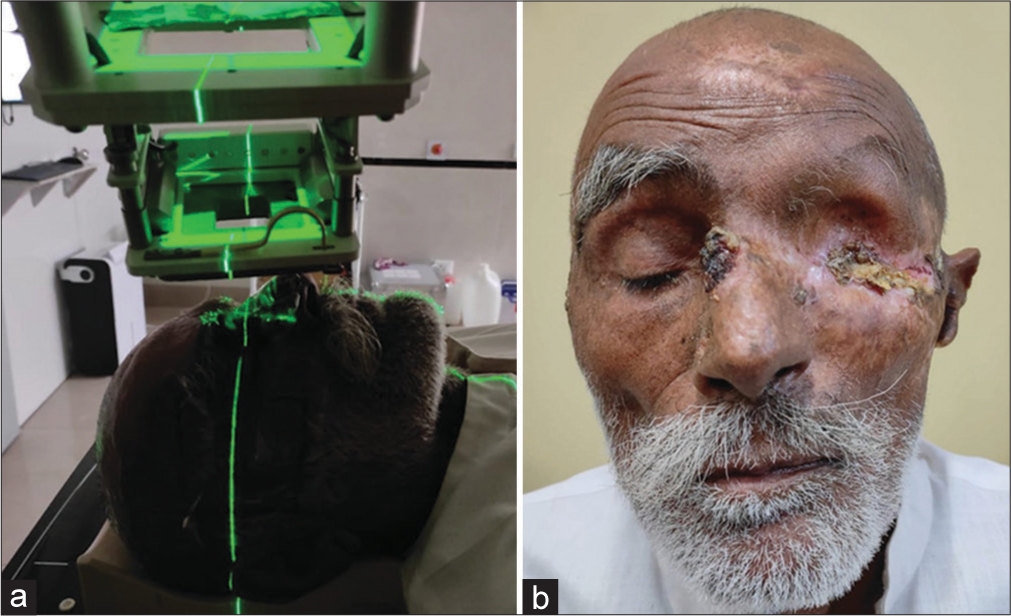
- (a) Treatment of basal cell carcinoma (BCC) with electron beam radiotherapy. (b) Depigmented atrophic scar extending from medial canthus to preauricular region and one crusted ulcer of size 0.5X1 cm over dorsum of nose and yellowish crusting over lateral canthus.

- Post 6 months follow-up clinical image with resolution of almost all previous ulcerated and crusted lesions and no recurrence.
DISCUSSION
BCC is known for its slow progression, rarity of metastasis, and good prognosis,2 but it is locally invasive and it can cause destruction of important structures nearby like eyes and ears. In GBCCs larger than 10 cm in diameter, the incidence of metastasis or death is nearly 50%.3 BCCs larger than 20 cm have recently been defined as “super-giant BCCs.”4 BCCs may attain giant or supergiant proportions primarily because of neglect or the poor socioeconomic status of the patient. Most GBCCs are located on the trunk, where the lesions are easily hidden. A GBCC on the outer canthus of the left eye without treatment for 12 years, as in our case, is uncommon.
Multiple modalities of treatment have been developed for non-melanomatous skin cancers, although no clear guidelines on the preferred method of treating large, progressive, and neglected tumors such as GBCCs have been mentioned. Various treatment options for GBCCs as per literature include wide local excision with a split-thickness skin graft,5 and chemotherapy with vismodegib.6
Surgical excision remains the gold standard and preferred modality in most cases. However, some patients may be poor candidates for surgical intervention, particularly the elderly and patients receiving anticoagulation. In addition, the location and size of the skin lesion can hinder an adequate surgical approach that would otherwise result in unacceptable cosmetic or functional outcomes, primarily in areas around the nose, lip, eyelids, medial canthus, and pinna. As such, these patients may be potential candidates for radiation therapy (RT) as an alternative primary treatment modality.7 Previous studies demonstrated cure rate ranging from 80% to 100%,8 but radiotherapy remain underutilized in the management of BCCs.
CONCLUSION
We hereby present a case of GBCC over the face near the eye with a good response to radiotherapy.
Acknowledgement
We have taken appropriate patient consent for using the clinical details and clinical images for publication.
Authors’ contributions
All the authors contributed to the research study. Shubham Kumar: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Suman Patra: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Bharti Devnani: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Varun Rajagopalan: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Maninder Kaur: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Giant mushroom-like neglected basal cell carcinoma of the shoulder with spontaneous bleeding: A successful surgical approach. Eur J Case Rep Intern Med. 2021;8:3089. doi:10.12890/2021_003089
- [CrossRef] [PubMed] [Google Scholar]
- Mushroom-like giant basal cell carcinoma on the nasal tip. Dermatol Surg. 2014;40:343-5.
- [CrossRef] [PubMed] [Google Scholar]
- Basal cell carcinoma: Influence of tumor size on mortality and morbidity. Int J Dermatol. 1995;34:319-21.
- [CrossRef] [PubMed] [Google Scholar]
- Super giant basal cell carcinoma of the abdominal wall: Still possible in the 21st century. Int J Dermatol. 2010;49:806-9.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of vismodegib in advanced basal-cell carcinoma. N Engl J Med. 2012;366:2171-9.
- [CrossRef] [PubMed] [Google Scholar]
- Electronic brachytherapy for treatment of non-melanoma skin cancers: Clinical results and toxicities. J Contemp Brachytherapy. 2021;13:497-503.
- [CrossRef] [PubMed] [Google Scholar]
- Utility of radiotherapy for treatment of basal cell carcinoma: A review. Br J Dermatol. 2014;171:968-73.
- [CrossRef] [PubMed] [Google Scholar]






