Translate this page into:
A pilot study on the efficacy of 10600 nm carbon dioxide laser ablation in treatment of eyelid margin lesions
*Corresponding author: Dr. Yogesh M Bhingradia, Shivani Skin Care and Cosmetic Clinic, 4th Floor Sarathi Doctor House, Varachha Road Hirabag, Surat, Gujarat, India. yogeshbhingradia@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: JPP, Bhingradia YM, Priya D, Pawar SB, Muthukumarasamy V. A pilot study on the efficacy of 10600 nm carbon dioxide laser ablation in treatment of eyelid margin lesions. J Cutan Aesthet Surg. 2024;17:320-4. doi: 10.25259/jcas_145_23
Abstract
Objectives:
Eyelid margin lesions cause discomfort by impeding both central and peripheral vision, depending on their position on the eyelids, thus hindering everyday routines. However, surgical excision, radiofrequency, electrocautery, and cryosurgery are employed for treatment, although they are complicated and have functional limitations. Carbon dioxide (CO2) lasers were used to assess the efficacy, safety, and patient satisfaction with CO2 laser ablation in managing eyelid margin lesions.
Material and Methods:
This is a pilot study of patients with eyelid margin lesions presented to a private clinic in urban Gujarat between June 2020 and June 2023. All patients were treated with a 10600 nm CO2 laser with a power of 1–2 W in continuous mode. The eyelid lesions were classified into three categories based on their size: Small (1–3 mm), medium (4–6 mm), and large (7–10 mm). The clinical response was assessed by the treating physician at week 1 and week 4, and categorized as excellent (complete clearance of lesion), moderate (>50%), or poor (<50%). Patients were asked to rate their level of satisfaction on a three-point scale at the end of the follow-up period: Dissatisfied, somewhat satisfied, or very satisfied.
Results:
Ten patients of all females with six of them having compound melanocytic nevi, two of them each had cystic hidradenoma, and one each had cyst of zeis and verruca vulgaris. Six of them had small lesions, two had medium, and two had large lesions. The clinical response grading of physicians at both 1 week and 4 weeks was excellent, and the patient satisfaction questionnaire yielded excellent outcomes.
Conclusion:
The ablative CO2 laser is an excellent device used for the treatment of eyelid margin lesions, particularly when performed by an expert and skilled dermatologist. The application of this treatment approach has proven to be very beneficial and shows excellent results in terms of both the esthetic appearance and structural function of the eyelids.
Keywords
Eyelid margin lesions
Carbon dioxide (CO2) laser
Ablative
INTRODUCTION
Lesions affecting the eyelid margin can cause discomfort by impeding both central and peripheral vision depending on their location on the eyelids, hindering normal daily activities. Given the potential impact on vision, it is imperative to remove these lesions as soon as possible. Eyelid lesion lesions are more commonly benign than malignant.1 The majority of eyelid lesions include chalazion, melanocytic, hidradenoma, molluscum contagiosum, mucosal cysts (cysts of Moll, Zeis), and epidermoid cyst, seborrheic keratosis, actinic keratosis, and acrochordon. Basal cell carcinoma, squamous cell carcinoma, sebaceous cell carcinoma, melanoma, and Merkel cell carcinoma are all malignant. There are extremely limited or no available data regarding eyelid margin lesions. The majority of the articles focus on eyelid lesions as opposed to eyelid margin lesions. Prior research in this area is lacking. Gradual enlargement, central ulceration or induration, irregular margins, destruction of the eyelid margin or loss of eyelashes, and telangiectasia are features suggestive of malignancy that should be further investigated.2 However, if any of these are not present, treatment options include surgical excision, laser curettage, radiofrequency, electrocautery, and cryosurgery; however, all of these procedures have limitations due to their complexity and intricacy, as well as the resulting functional defects of the eyelids, such as scarring, irritation bleeding, infections, skin discoloration, hypotrichosis, ciliary madarosis, scarring with ectropion, trichiasis, dry eyes, asymmetrical eyelids, lagophthalmos, ptosis, and epiphora. Photodynamic therapy has been used for the treatment of eyelid margin tumors as cryotherapy, surgical excision has limitations related to the complexity and functional deficiencies. In 1976, Apfelberg et al. described the use of lasers in the treatment of benign skin lesions.3 The carbon dioxide (CO2) laser is one of the most frequently used lasers in dermatology. The high water content of the skin makes the CO2 laser an ideal option for precise ablation with minimal bleeding and excellent hemostasis along with minimal collateral tissue damage. Zhang et al. and Ozaki et al. used CO2 laser to acquire melanocytic nevi safely.4,5 As a result, a CO2 laser was utilized to treat the eyelid margin lesions. This case series focused on the efficacy, safety, and patient satisfaction with continuous CO2 laser ablation for the treatment of eyelid margin lesions. No articles, case series, or studies on the treatment and prognosis of benign eyelid margin lesions with CO2 lasers have been published to our knowledge, so we opted to publish this article.
MATERIAL AND METHODS
Patients with eyelid margin lesions who presented to a private clinic in urban Gujarat between 2020 and 2023 were included in the study. All cases were clinically diagnosed; benign lesions that were long-standing, asymptomatic, and non-inflammatory were included, whereas any with malignancy features such as gradual enlargement, central ulceration or induration, irregular borders, eyelid margin destruction or loss of lashes, and telangiectasia were excluded and referred to an ophthalmologist for further evaluation. Patients were Fitzpatrick skin type III to V. Age, gender, clinical diagnosis and size, laterality, comorbidities, treatment, and outcome were all recorded. Patients under the age of 18 with a known lignocaine allergy, anticoagulant medication, pacemakers, a known cardiac problem, and a keloidal tendency, participants who declined participation, and pre-and post-treatment photos were excluded from the study. The study adhered to the tenets of the Declaration of Helsinki.
An in-depth description of CO2 laser ablation treatment was provided to all patients, including details about the treatment process, related expenses, possible benefits, expected duration, possible adverse effects, and prognosis. Oral, written, and photographic consent was taken from each patient before the procedure. Digital images of the lesion were captured before and after the procedure, and also during subsequent follow-up.
Procedure
The treatment areas were cleaned of dirt, makeup, and powder using a mild cleanser and 70% isopropyl alcohol. After the application of procaine eye drops, metal corneal eye shields were inserted to protect the patients’ eyes from laser treatment. Inj. Lignocaine 2% through an insulin syringe with a 26 G needle given at the base of the lesion. We categorized the eyelid lesions as small (1–3 mm), medium (4–6 mm), and large (7–10 mm). All patients were treated with a 10600 nm CO2 laser with a power of 1–2 W in continuous mode. The procedure was carried out in an aseptic environment. Laser ablation was performed to the base of the lesion. Ablated tissue was removed with a saline gauze piece and topical antiseptic cream was applied. Post-operative patients were instructed to apply topical antiseptic cream and the patient was examined after a week. The CO2 laser ablation was carried out in a single session and, if deemed necessary, was repeated after a week or 2. The treating physician graded the clinical response by focusing on three categories: Excellent – complete clearance (100%) of the lesion, moderate clearance (>50 cleared), and poor clearance (<50% cleared). This grading was performed at week 1 and after 4 weeks. Patients’ satisfaction questionnaire with a 3-point grading scale as follows: Very satisfied, somewhat satisfied, and dissatisfied, was completed by every patient at the end of the follow-up period. During post-operative follow-ups, any potential complications, adverse effects, texture changes, scarring, post-inflammatory pigmentation, or loss of eyelashes that occurred were documented. All patients received a similar treatment protocol (parameters). The same dermatologist provided treatment and assigned grades during each visit.
RESULTS
All ten cases were women aged 25–65 years. Six had compound melanocytic nevi, two had cystic hidradenoma, and one each cyst of zeis and verruca vulgaris. Six patients had small lesions, two patients had medium lesions, and two had large lesions. Six had upper eyelid margin involvement, three had lower eyelid margin involvement, and one had right lateral canthus involving both the upper and lower eyelid. Details are given in Table 1. The clinical response grading of all patients by the dermatologist at 1 week and 4 weeks was excellent [Figures 1a and b, 2a-d, 3a and b, 4a-c]. The patient satisfaction questionnaire with a 3-point grading scale was very satisfied at the end of 1 week and also at the end of 4 weeks. All patients had mild erythema and crusting at the end of a week but at the end of 4 weeks, skin was fully reepithelialized. There was no evidence of residual or recurrence of lesions in any of the patients, especially in melanocytic nevi and verruca vulgaris. There was no loss of eyelashes or structural or morphological deformity of the eyelid.
| Gender | Female | 10 |
| Laterality | Right eye | 8 |
| Left eye | 2 | |
| Site | Upper eyelid | 6 |
| lower eyelid | 3 | |
| lateral canthus | 1 | |
| Type of lesion | CML (compound melanocytic nevi) | 6 |
| cystic hidradenoma | 2 | |
| Verruca vulgaris | 1 | |
| cyst of Zeis | 1 | |
| Size of lesion | Small lesion | 6 |
| Medium lesion | 2 | |
| Large lesion | 2 | |
| Physician assessment of clinical response CO2 Ablation | Excellent | 10 |
| Patient satisfaction questionnaire | Very satisfactory | 10 |
| Post-CO2 ablation complication | Nil |
CO2: Carbon dioxide, CML: Compound melanocytic nevi
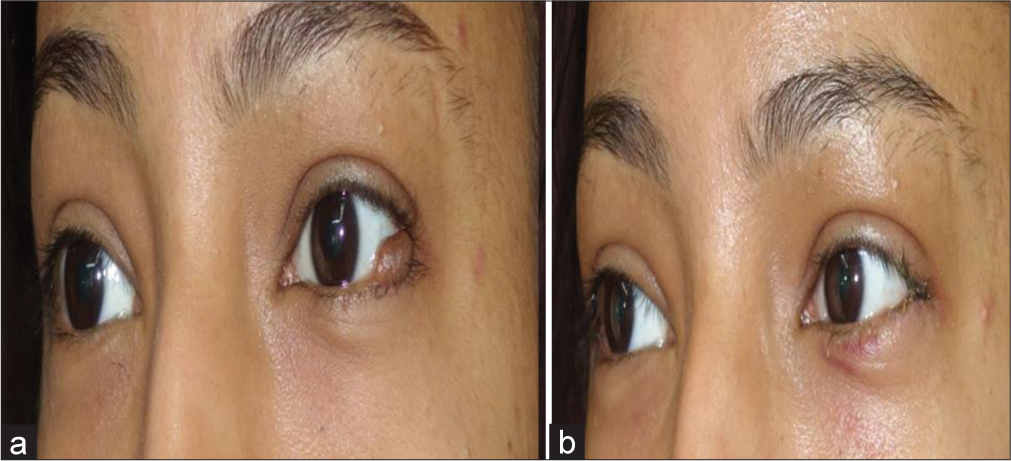
- (a) Large melanocytic nevi pre-procedure and (b) 1 week post-procedure.

- (a) Cystic hidradenoma on upper eyelid pre-procedure, (b) during the procedure, (c) immediately post-procedure, and (d) 4 weeks after the procedure.
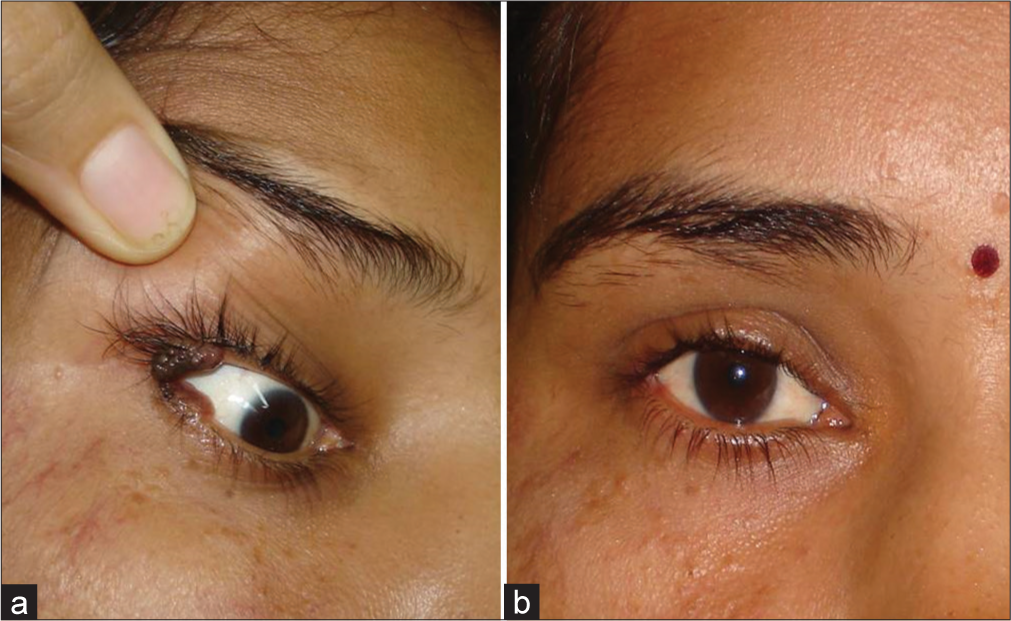
- (a) Large melanocytic nevus of the upper and lower eyelids affecting the lateral canthus of the right eye and (b) 4 weeks after the procedure.
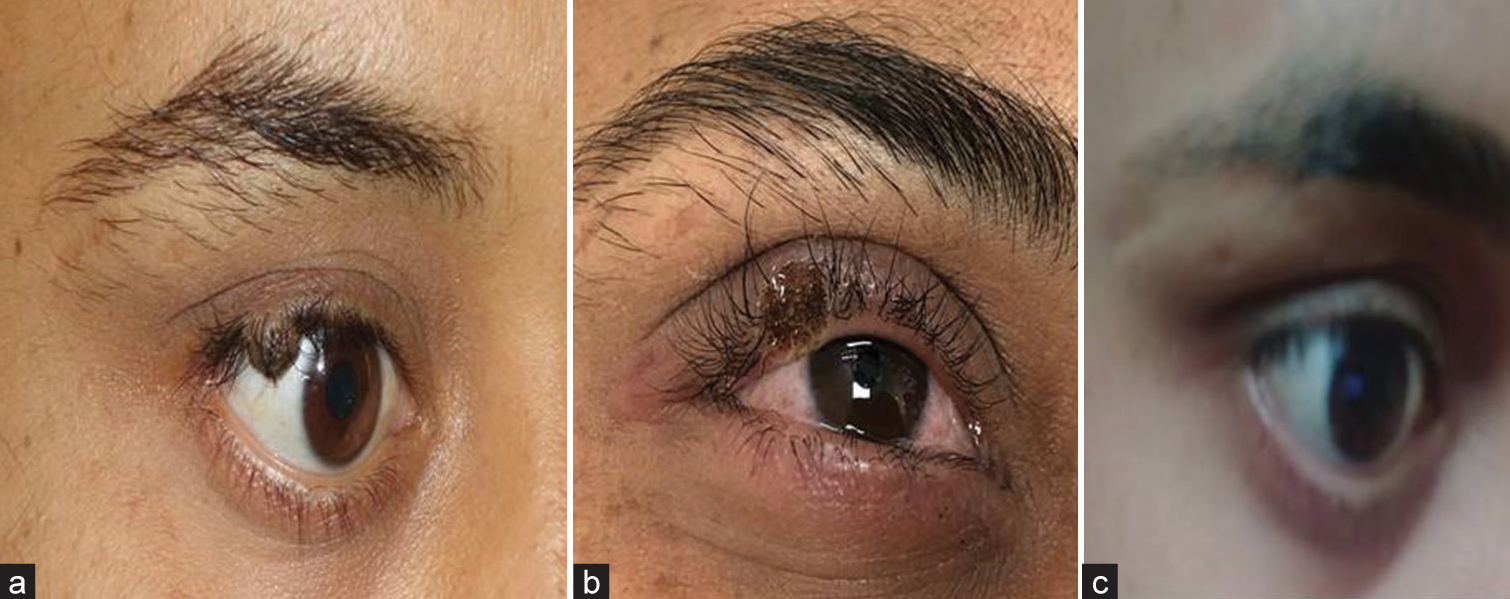
- (a) Medium melanocytic nevi, (b) immediate post-procedure, and (c) 4 weeks later.
DISCUSSION
Ablative lasers have been utilized to ablate superficial skin lesions. CO2 lasers with a wavelength of 10,600 nm are used to ablate skin lesions due to their precise ablation, lack of bleeding, least amount of collateral damage, and better homeostasis with convenience of usage. Smaller than 3 mm diameter melanocytic nevus was safe with CO2 according to Ozaki et al.5 Fractional ablative CO2 lasers have been used for acquired medium-sized melanocytic compound and dermal nevi.6 Due to the risk of scarring, some clinicians prefer surgical resection over CO2 laser excision for lesions larger than 3 mm. However, Zhang et al. used a CO2 laser 4-step approach to remove large melanocytic nevi with diameters of 3–7 mm, as well as melanocytic nevi at the lid margin.4 For this reason, we considered using a CO2 laser even for larger lesions and tried to remove the lesions in a single session. Carbon-di-oxide laser in continuous mode is among the effective ablative laser systems in the treatment of melanocytic nevi.5 Numerous authors have pointed out the advantages of CO2 laser over surgical excision, so we considered using CO2 laser in continuous mode for eyelid margin lesions. We exercised extreme caution in utilizing CO2 as it has an unpredictable penetration depth and carries a significant risk of lid deformities, textural changes, and post-laser pigmentation particularly in individuals with darker skin. Very few studies have been conducted on eyelid margin lesions and their treatment. According to our study and other researchers’ observations, eyelid margin lesions were more prevalent in females.7,8 There is currently no available data in scientific literature regarding the frequency, gender distribution, or age group affected by eyelid margin lesions. Benign eyelid lesions were observed more frequently in the middle age population, melanocytic nevi were the most common benign eyelid margin lesions observed in our case series, which was also supported by other studies. Eyelid tumors were observed to be more common in the right eye with upper lid involvement in six of our patients, as also documented by Banerjee et al.1 Eyelid nevi were seen in six patients in our study as against 8.5% noticed by Adamski et al.7 whereas hidrocystoma was the most common benign eyelid lesion by Al-Faky, as compared to only two patients in our case.9 Squamous papilloma was the most common by Gundogan et al.10 The functionality of CO2 laser involves the destruction of the target cells directly. CO2 laser has a greater ablation depth of 20–60 μm per pass and causes greater thermal coagulation, which explains its complete elimination of nevus cells, thus lowering the risk of recurrence.11 We did not see any recurrence or partial ablation of the lesions as all patients had an excellent outcome. Due to its unpredictable penetration depth, CO2 laser in continuous mode is thought to have the potential for textural changes; however, we did not see any of such changes postoperatively in any of our patients. The overall findings of our study demonstrated that CO2 ablative lasers can be used safely for treating benign eyelid margin lesions with a favorable outcome with minimal structural distortion. Overall results of our study pointed out that CO2 ablative lasers can be used safely to treat benign eyelid margin lesions with excellent outcomes and with no structural deformity.
CONCLUSION
The ablative CO2 laser is an amazing device, especially when utilized by a skilled dermatologist, and serves as a valuable therapeutic option for benign eyelid margin lesions and provides excellent outcomes in terms of both cosmetic appearance and the structural functionality of the eyelids.
Authors’ contributions
All authors did contribute for the research and analysis of the study.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964 and was conducted in the Urban Clinic in Surat Gujarat.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- The spectrum and clinicopathological correlation of eyelid lesions: Twenty years' experience at a tertiary eye care center in South India. Indian J Ophthalmol. 2022;70:43-50.
- [CrossRef] [PubMed] [Google Scholar]
- Eyelid lesions in general practice. Aust J Gen Pract. 2019;48:509-14.
- [CrossRef] [PubMed] [Google Scholar]
- Argon laser management of cutaneous vascular deformities. A preliminary report. West J Med. 1976;124:99-101.
- [Google Scholar]
- Aesthetic removal of large melanocytic nevi using CO2 lasers with a programmed 4-step approach. Int J Clin Exp Med. 2018;11:6309-15.
- [Google Scholar]
- Efficacy of serial excisions of melanocytic nevi on the face using a carbon dioxide laser: A cosmetic point of view. Aesthetic Plast Surg. 2014;38:316-21.
- [CrossRef] [PubMed] [Google Scholar]
- Carbon dioxide ablative laser treatment of acquired junctional melanocytic nevi. J Cosmet Dermatol. 2021;20:491-6.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of various eyelid skin lesions in a single-centre observation study. Postepy Dermatol Alergol. 2021;38:804-7.
- [CrossRef] [Google Scholar]
- A retrospective study of 2228 cases with eyelid tumors. Int J Ophthalmol. 2018;11:1835-41.
- [Google Scholar]
- Epidemiology of benign eyelid lesions in patients presenting to a teaching hospital. Saudi J Ophthalmol. 2012;26:211-6.
- [CrossRef] [PubMed] [Google Scholar]
- Eyelid tumors: Clinical data from an eye center in Ankara, Turkey. Asian Pac J Cancer Prev. 2015;16:4265-9.
- [CrossRef] [PubMed] [Google Scholar]
- Ultra-pulsed carbon dioxide laser for the treatment of melanocytic nevi. Dermatol Dermatit 2019 Doi: 10.31579/2578-8949/054
- [CrossRef] [Google Scholar]







