Translate this page into:
Comparative evaluation of conventional versus modified lip repositioning surgery for gummy smile: A two-year follow-up study
*Corresponding author: Sneha Puri, Department of Periodontology, Swargiya Dadasaheb Kalmegh Smruti Dental College and Hospital, Nagpur, Maharashtra, India. snehaghenekar@gmail.com
-
Accepted: ,
How to cite this article: Puri S, Shewale A. Comparative evaluation of conventional versus modified lip repositioning surgery for gummy smile: A two-year follow-up study. J Cutan Aesthet Surg. doi: 10.4103/JCAS.JCAS_173_20
Abstract
Excessive gingival display can be managed by a variety of treatment modalities, depending on the specific diagnosis. Lip repositioning surgery is a largely unknown and underutilized treatment modality for excessive gingival display. The aim of the present study was to minimize gingival display by comparing the modified lip repositioning procedure with the conventional lip repositioning procedure. A total of 12 patients with gummy smile were selected for the study. The patients were randomly divided into two groups (group A and group B), consisting of six patients each. Group A patients were treated with conventional lip repositioning procedure and group B patients were treated with modified lip repositioning procedure. The procedure resulted in a narrower vestibule and restricted muscle pull, thereby reducing gingival display during smiling. The lip repositioning technique that was meant to decrease the amount of gingival display proved to be more conservative and provided a good aesthetic outcome.
Keywords
Gummy smile
Hypermobile lip
Lip repositioning procedure
Modified lip reposition procedure
INTRODUCTION
Currently, a growing concern for beauty and physical appearance has motivated the clinician to consider the person’s smile and the relationship between the dentition, gingiva, and lips while smiling. There has also been a steady rise in the importance of the potential of plastic periodontal surgical procedures to enhance the smile line. An exposed gingiva of 2–3 mm is cosmetically acceptable; however, more than this is considered to be unattractive and is commonly known as “gummy smile.”(Silberberg, 2009)1 It is a condition that is caused primarily by a skeletal deformity in which there is vertical maxillary excess tissue, a soft-tissue deformity in which there is a short upper lip or a combination of the two (Garber, 1996).2 Variable treatment outcomes have been reported for the gummy smile, such as botulinum toxin injection (Mazzuco 2010),3 lip elongation associated with rhinoplasty, detachment of lip muscles, myectomy and partial removal, and lip repositioning.
Lip repositioning surgery was introduced as a minimally invasive surgery wherein a strip of lip mucosa, including the labial frenum, was detached and the boundaries were sutured for the approximation. Co Silva modified the technique and suggested preservation of the labial frenum to facilitate the position of the labial midline and to reduce the postoperative morbidity.
As per our knowledge, till date, only one comparative long-term clinical trial has been carried out to evaluate the outcomes of both the techniques. The present trial is an attempt to compare and evaluate the long-term outcomes of both the modalities.
MATERIALS AND METHODS
Twelve patients (seven females, five males) aged between 17 and 25 years (20.5) were divided randomly into two groups. The study sampling power was 80v% (1-β = 0.8). All patients presented to the department of Periodontology, SDKS Dental College and Hospital, Nagpur, between April 2014 and May 2015.
Group A (6 patients)—Conventional lip repositioning procedure
Group B (6 patients)—Modified lip repositioning procedure
Both the procedures were carried out by a single operator.
Criteria
Inclusion criteria were adult patients aged between 18 and 38 years, with a gummy smile of 4 to 6 mm related to a short upper lip or hyperactive lip elevator muscles, in good periodontal health, as well as systemically healthy patients.
Exclusion criteria were smokers, pregnant or lactating women, < 3 mm attached gingivae, and vertical maxillary excess of more than 6 mm.
Clinical measurements
The clinical measurements recorded at baseline and at three months postoperatively with the help of a University of North Carolina (UNC) calibrated probe were lip length and the distance between the gingival margins and the lower border of the upper lip [Figure 1a].
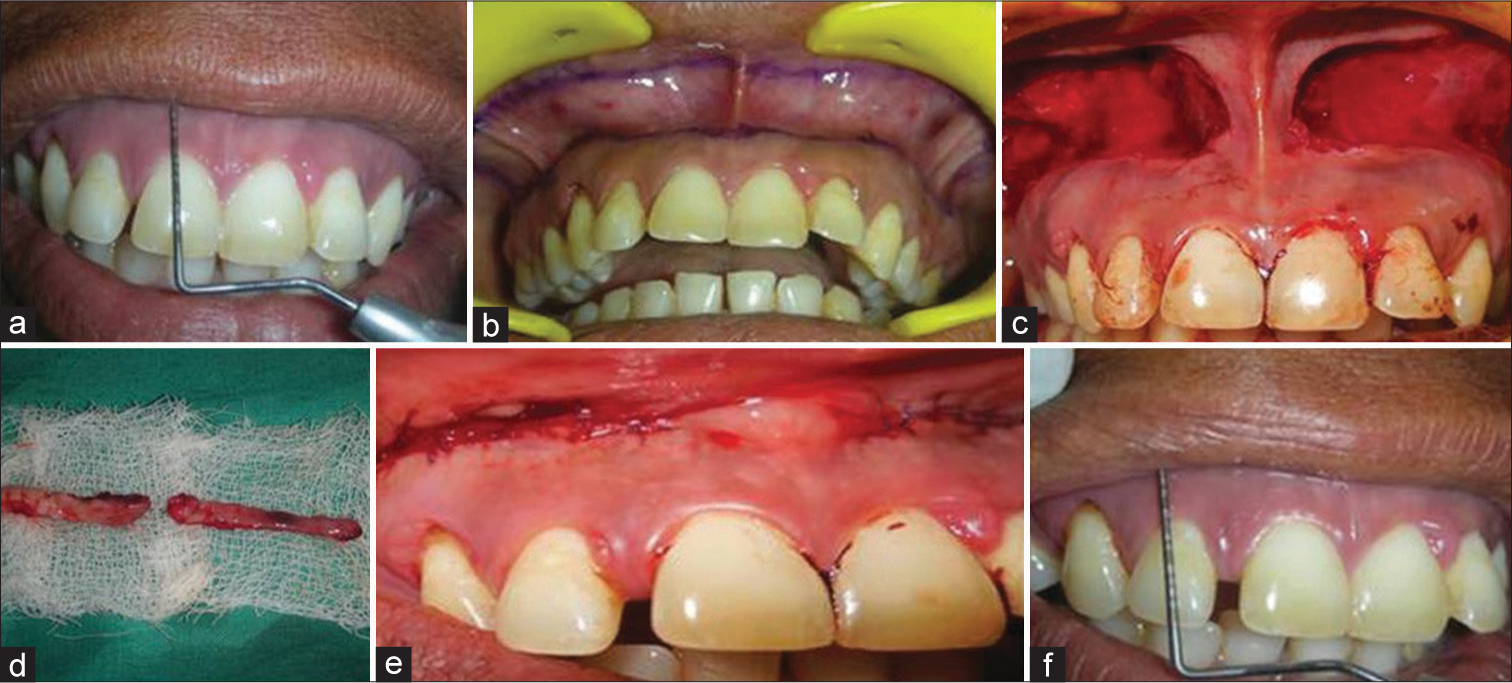
- Surgical procedure for Group A. (a) Preoperative measurements. (b) Outline marked. (c) Dissection of mucosa. (d) Excised mucosa. (e) Sutures placed. (f) Postoperative measurements.
Surgical procedure for group A
A sterile surgical marking pen was used to mark incision outlines on the dried mucosa of each patient [Figures 1b and 1c]. A partial-thickness horizontal incision was made 1 mm coronally to the mucogingival junction (MGJ) from the mesial line angle of the right maxillary first molar to the mesial line angle of the left maxillary first molar. A V shape was inserted in the upper lip frenum area to facilitate accurate positioning of the labial midline during closure. A second horizontal incision was made in the labial mucosa approximately 10 to 12 mm apical to the first incision. The two incisions were connected at the mesial line angles of the right maxillary first molar and the left maxillary first molar to create an elliptical outline. The strip of the outlined mucosa was removed by a superficial split-thickness dissection [Figure 1d], leaving the underlying connective tissue exposed [Figure 1c]. Bleeding was controlled by additional local anesthesia infiltration and the use of electrocoagulation. Care was taken to avoid damaging the minor salivary glands in the submucosa. The incision lines were approximated with interrupted stabilization sutures (silk 4/0) at the midline and other locations along the borders of the incision to ensure accurate alignment. Interrupted sutures were used to approximate flap ends [Figures 1e and f].
Surgical procedure for group B
The surgical procedure was similar to the one carried out in Group A, with the only difference of sparing the labial frenum from dissection [Figure 2].
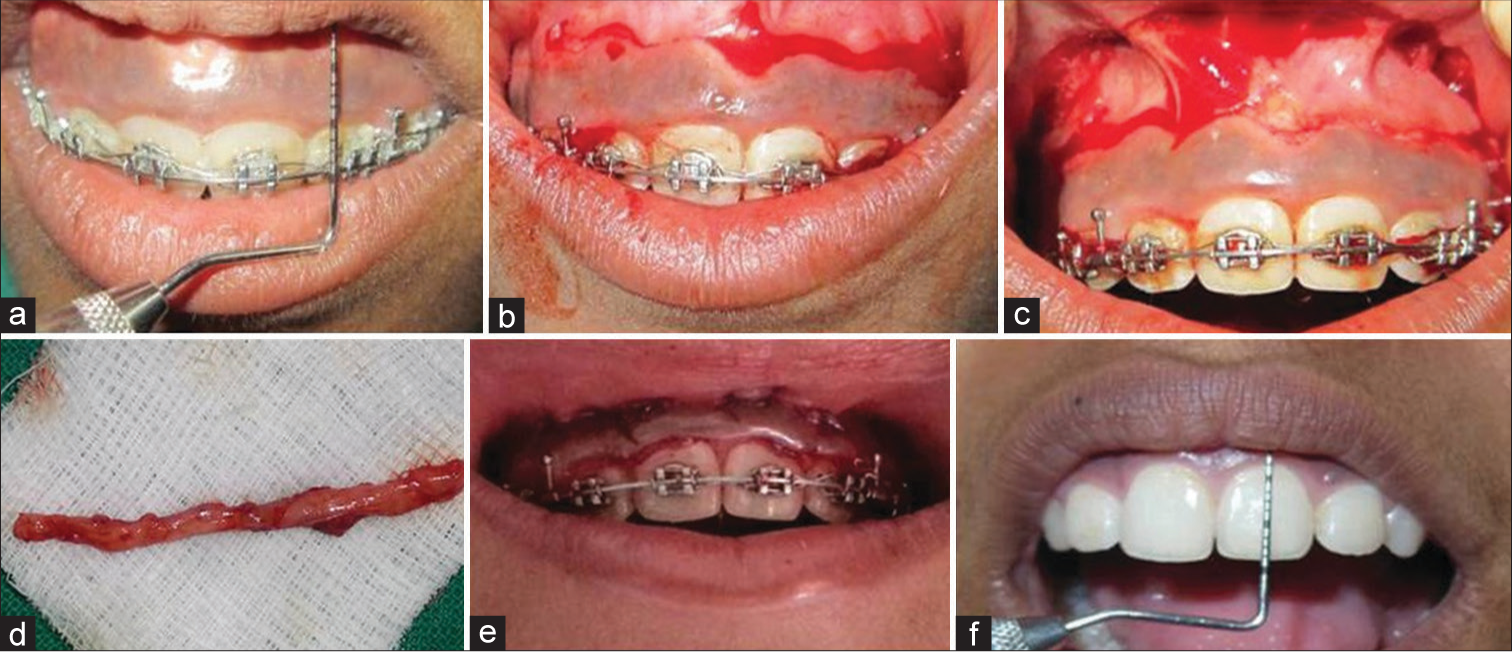
- Surgical procedure for Group B. (a) Preoperative measurements. (b) Incisions placed. (c) Dissection of mucosa. (d) Excised mucosa. (e) Sutures placed. (f) Postoperative measurements.
Statistical analysis
Comparisons of the treatment modality on the maximum lip length achieved were measured by using paired t-tests using a significance value of P<.05 (SPSS version 13).
RESULTS
Twelve patients (seven females and five males), comprising six patients in each group, and in the age range of 19 to 49 years were recruited for the study. The study participants were followed up at six months, at one and two years postoperatively. On the whole, patients were satisfied with both the procedures. The mean rates of gingival display at baseline were 6.45 mm in group 1 and 5.74 mm in group 2. There was no significant difference between the two groups for gingival display at baseline [Table 1]. However the changes were statistically significant at follow-up intervals, namely at six months, one and two years postoperatively (P < 0.05) [Tables 1, 2 and Figures 3, 4].
| Study period | Treatment technique | Number | Mean | Std. deviation | Std. error | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| Before treatment | Modified technique | 6 | 6.45 | 1.14 | 0.44 | 5 | 8 |
| Conventional technique | 6 | 5.74 | 0.82 | 0.23 | 5 | 7 | |
| After six months | Modified technique | 6 | 1.02 | 0.97 | 0.46 | 0 | 5 |
| Conventional technique | 6 | 1.85 | 0.81 | 0.26 | 1 | 5 | |
| After one year | Modified technique | 6 | 1.93 | 1.17 | 0.38 | 0 | 4 |
| Conventional technique | 6 | 2.91 | 1.01 | 0.28 | 2 | 5 | |
| After two years | Modified technique | 6 | 2.69 | 1.10 | 0.34 | 0 | 4 |
| Conventional technique | 6 | 3.75 | 0.75 | 0.24 | 2 | 5 |
| Studied period | Mean difference | t-test | P-value |
|---|---|---|---|
| Before treatment | 0.71 | 1.376 | 0.18 |
| After 6 months | −0.77 | −2.874 | 0.06 |
| After 1 year | −0.98 | −0.489 | 0.51 |
| After 2 years | −1.06 | −1.874 | 0.08 |
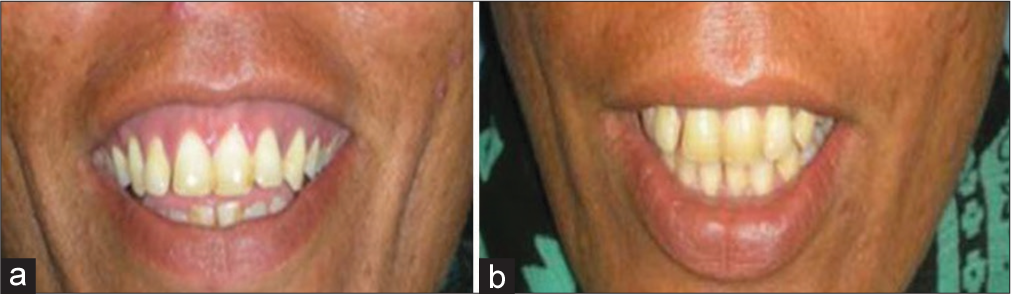
- Postoperative view after 2 years for Group A. (a) Preoperative view. (b) Postoperative view after 2 years.
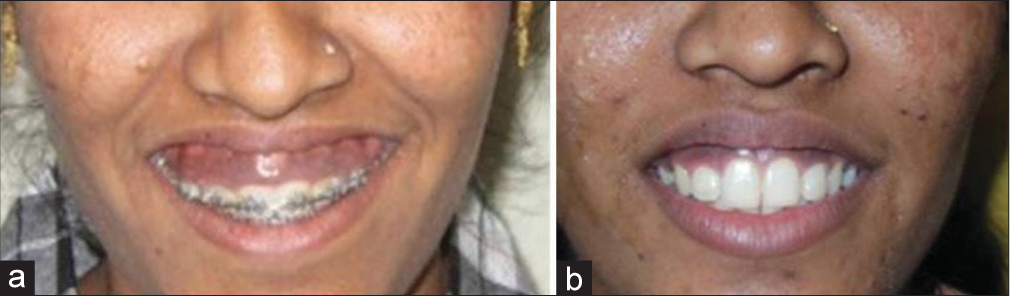
- Postoperative view after 2 years for Group B. (a) Preoperative view. (b) Postoperative view after 2 years.
DISCUSSION
Gummy smiles or excessive gingival displays often causes aesthetic concern among the individuals exhibiting them. Scientific literature is abounding with case reports of different treatment options for this condition, depending on the etiology; however, it is lacking in outcome studies.4-6
However, as per our knowledge, till date, there is one reported study comparing modified and conventional lip repositioning techniques at six months of follow-up (Allamar 2018).7 The main goal of this study was to assess and compare the outcomes of modified and conventional techniques of lip repositioning surgery in the treatment of gummy smile caused only by soft tissue disorders (short upper lip—hyperactive lip elevator muscles) and to evaluate postoperative relapse with long-term follow-up.
The reduction in gingival display using the modified technique was greater compared with that in the conventional technique at six months, one and two years postoperatively.
The results of modified lip repositioning surgery were stable for up to two years postoperatively, with only minor relapse in some cases. This may be because of the muscle memory trying to restore its preoperative activity. These results are consistent with those of other studies regarding modified lip repositioning surgery.8-10 We encountered only two cases with complete relapse in the conventional lip repositioning group, which appeared to be because of excessive tension of lip elevator muscles. However, studies for longer follow-up periods postoperatively are necessary to establish the long-term stability of both modified and conventional techniques of lip repositioning surgery.
Occurrence of mucocele due to severing of minor salivary glands in the upper lip as evident in previous literature were not found in our study.
Other reported complications include a feeling of discomfort, numbness, and difficulty in some movements of the upper lip. However, our study participants have not reported any such complications during the follow-up intervals.
CONCLUSION
This study revealed that the modified technique contributed to the reduction in the relapse after surgery and offered better surgical results and more stability during follow-up periods compared with the conventional technique. Additional randomized controlled studies with longer follow-up periods are required to further evaluate the modified technique.
Authors’ Contributions
All the authors contributed to the research study. Sneha Puri: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Akhilesh Shewale: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Excessive gingival display–Etiology, diagnosis, and treatment modalities. Quintessence Int. 2009;40:809-18.
- [Google Scholar]
- The aesthetic smile: Diagnosis and treatment. Periodontol. 2000-1996;11:18-28.
- [CrossRef] [Google Scholar]
- Gummy smile and botulinum toxin: A new approach based on the gingival exposure area. Journal of the American Academy of Dermatology. 2010;63:1042-51.
- [CrossRef] [Google Scholar]
- An innovative cosmetic technique called lip repositioning. J Indian Soc Periodontol. 2010;14:266-9.
- [CrossRef] [Google Scholar]
- Lip repositioning for reduction of excessive gingival display: A clinical report. Int J Periodontics Restorative Dent. 2006;26:433-7.
- [Google Scholar]
- Eliminating a gummy smile with surgical lip repositioning. J Cosmetic Dent. 2007;23:102-9.
- [Google Scholar]
- A comparison between modified and conventional surgical techniques for surgical lip repositioning in the management of the gummy smile. J Esthet Restor Dent. 2018;30:523-31.
- [CrossRef] [Google Scholar]
- Modifying gummy smile: A minimally invasive approach. J Contemp Dent Pract. 2014;15:821-6.
- [CrossRef] [Google Scholar]
- A new approach to smiling deformity: Cutting of the superior part of the orbicularis oris. Aesthetic Plast Surg. 2005;29:373-7. discussion 378
- [CrossRef] [Google Scholar]
- Efficiency of gummy smile correction using the Myotomy of the elevator of the upper lip muscle. PlastReconstr Surg. 2009;124(4S):10-11.
- [Google Scholar]






