Translate this page into:
Comparative study of microneedling monotherapy versus microneedling with autologous platelet-rich plasma for the treatment of stretch marks (striae distensae) and post-surgical scars: Clinical and dermoscopy outcomes
*Corresponding author: Dr. Tejinder Kaur, Department of Dermatology, Leprosy and Venereology, Government Medical College, Amritsar, India. tejinderkaurdr@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kaur T, Kaur S, Bagga PK, Sidhu S, Raj RT. Comparative study of microneedling monotherapy versus microneedling with autologous platelet-rich plasma for the treatment of stretch marks (striae distensae) and post-surgical scars: Clinical and dermoscopy outcomes. J Cutan Aesthet Surg. 2024;17:307-14. doi: 10.25259/jcas_45_23
Abstract
Objectives:
Stretch marks and post-surgical scar marks may have negative cosmetic and psychological impacts.. Thus, this study aimed to compare the efficacy and safety of microneedling monotherapy versus microneedling in combination with autologous platelet-rich plasma (PRP) for the treatment of stretch marks and post-surgical scars.
Material and Methods:
This was a prospective randomized non-controlled study. A total of 30 study participants with stretch marks and post-surgery scars were enrolled and randomly divided into two groups, each with 15 study participants. All received three treatment sessions using microneedling monotherapy (Group A) or autologous PRP with microneedling (Group B) at 4-week intervals. Clinical response to treatment was assessed at the end of 20 weeks by comparing clinical photographs, Manchester Scar scale (MSS) score, dermoscopy images, and patient satisfaction scores.
Results:
At the end of the study, statistically significant esthetic improvement in terms of MSS scores was seen in Group B when compared to Group A. In Group A, 73.3% of the study participants were satisfied while in Group B, 86.6% were very satisfied with the results. Dermoscopy pictures substantiated the findings of clinical improvement. No major side effects were documented.
Conclusion:
PRP in combination with microneedling has a better outcome as compared to microneedling monotherapy. Furthermore, dermoscopy is a non-invasive tool that can be used to evaluate therapeutic response.
Keywords
Microneedling
Autologous platelet-rich plasma
Stretch marks
Dermoscopy
Scar marks
INTRODUCTION
Striae distensae, commonly known as stretch marks, are dermal scars of a disfiguring nature and are characterized by linear bands or streaks of flattened, atrophic-looking skin. Their prevalence ranges from 11 to 88%, seen in the majority of pregnant women and adolescents. Another condition leading to dermal scarring includes post-surgical scars which often leave behind a disfiguring and cosmetically unacceptable impression. The physical and psychological aspects related to these conditions have a significant impact on well-being, social engagement, and quality of life. Treatment of stretch marks and post-surgical scars is very challenging and no definite treatment modality is yet established.1
Microneedling and autologous platelet-rich plasma (PRP) are both novel therapeutic modalities in dermatology. Microneedling helps in collagen induction and has the beneficial properties of being minimally invasive and cost-effective with fewer side effects. It is also known to enhance drug delivery by depositing drug directly into the vascularized dermis, thus bypassing the stratum corneum.2
PRP, a platelet concentrate, has a high concentration of growth factors that help promote wound healing and tissue regeneration. Being autologous reduces the risk of adverse reactions and infections transmitted through transfusion.3
The use of autologous PRP in combination with microneedling has been hypothesized to have augmenting effects, supplementing each other’s actions when used together.
This study aimed to compare the efficacy and safety of the combination of microneedling and autologous PRP versus microneedling monotherapy for the treatment of stretch marks and post-surgical scars so that a dermatologist can opt for the best technique and help in improving these cosmetic problems at a cost-effective and safer way.
MATERIAL AND METHODS
After obtaining approval from the Institutional Ethics Committee (IEC No-3384/D-26/2020), a total of 30 study participants with stretch marks and post-surgical scar(s) were selected at random, from the Outpatient Department of Dermatology, Venereology, and Leprosy of a tertiary care hospital in North India between July 2020 and December 2022. The selected participants fulfilled the following criteria:
Inclusion criteria
Study participants within the age group of 18–40 years with atrophic scar marks and stretch marks having realistic expectations with ability and willingness to comply with the requirements of treatment protocols were included in the study.
Exclusion criteria
Study participants who do not give consent, those below 18 years and above 40 years, pregnant and lactating women, having active infections like herpes-type I OR II, human immunodeficiency virus, hepatitis B virus, hepatitis C virus, patients with any inflammatory dermatoses (atopic dermatitis, psoriasis), immunocompromised individuals and patients on immunosuppressive therapy, patients with the tendency of delayed wound healing like in diabetes, history of keloid scarring, bleeding disorder, collagen vascular disease, anticoagulant therapy, retinoid therapy, hormone therapy, presence of skin cancers, warts, solar keratoses, or any other skin infections, study participants who have received any treatment procedure for stretch marks and post-surgical scars including any type of laser modality within 1 year of study initiation, and those with unrealistic expectations were excluded from the study.
Written informed consent was obtained, and the selected study participants were randomized into two groups of 15 each by lottery method (Group A received microneedling monotherapy and Group B received a combination of microneedling with autologous PRP).
In both the groups, before the start of the procedure, a cosmetic assessment was done using the Manchester scar scale (MSS) [Figure 1],4 clinical photographs, and dermoscopy (using AM7515MZT Dino-lite dermatoscope with ×20–×220 magnification, Amno Electronics Pvt. Ltd., Taiwan) pictures. Scores on the MSS range from a maximum of 18 points to a minimum of 5, with lower scores indicating better esthetic appearance.
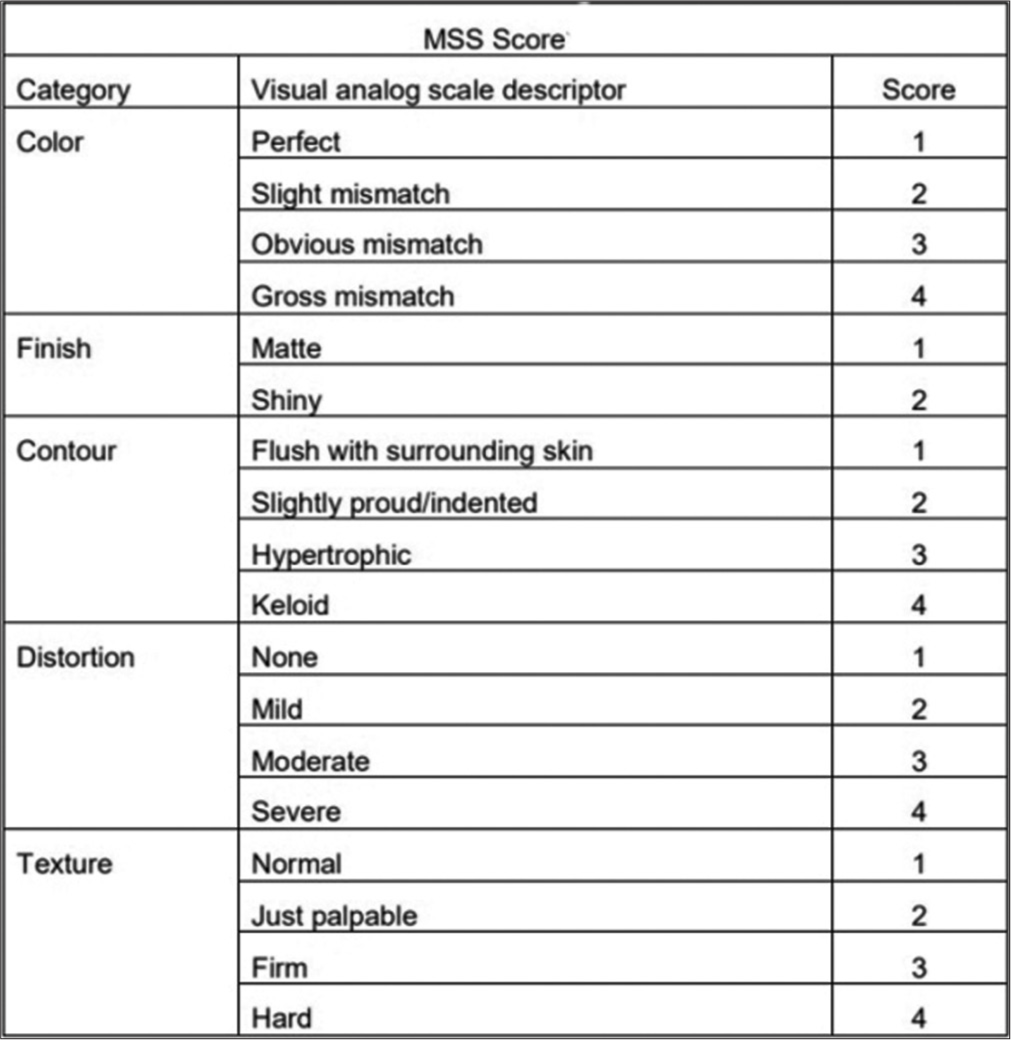
- Manchester scar scale (MSS) score.
The procedure was performed over three sessions, separated by 4 weeks, and 4 weekly follow-ups of the study participants were done up to 20 weeks. During each visit, pre- and post-treatment clinical and dermoscopy photographs were taken. Clinical improvement was assessed statistically with the help of MSS score and patient satisfaction score (PSS).5 At the end of 20 weeks, global improvement scores were assessed (Study design [Figure 2]).6
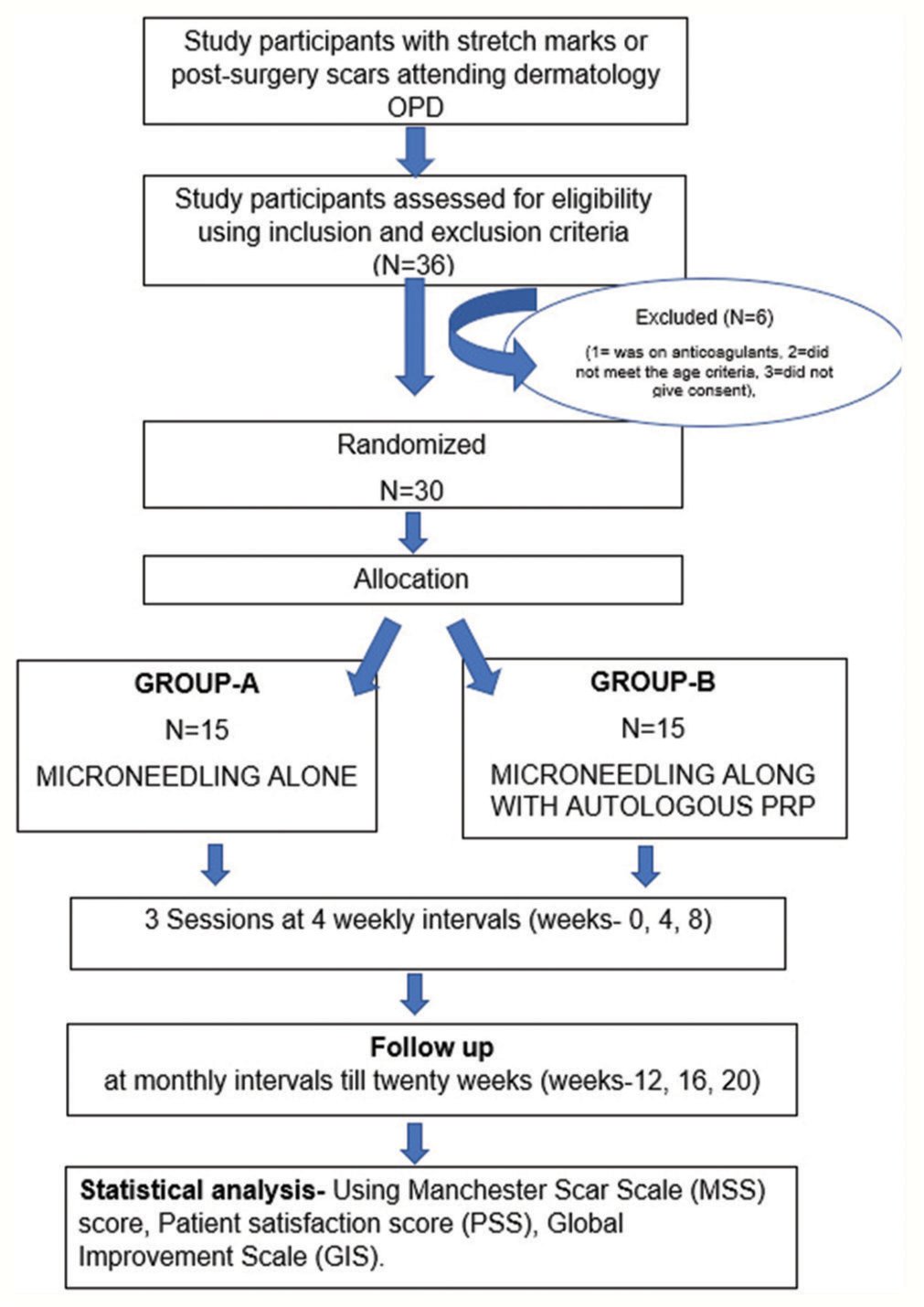
- Flowchart depicting the randomization of the study. OPD: out-patient department. PRP: platelet-rich plasma
Procedure for autologous PRP preparation
Preparation of PRP was done using the double spin method. Steps of preparations as shown in Figure 3 and 4 were followed and PRP, thus, obtained was used for the procedure.
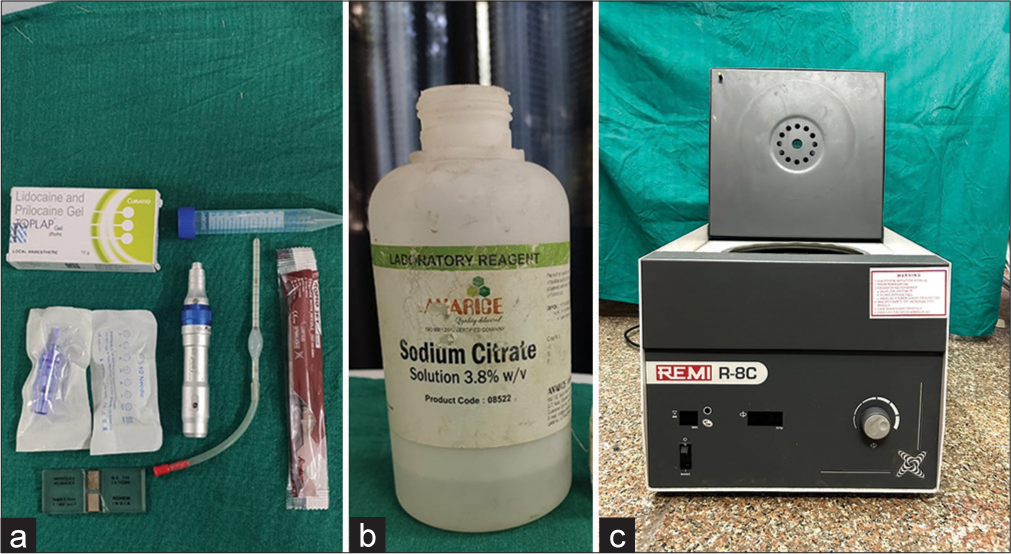
- (a) Materials utilized for the procedure Dermapen (model: Dr.pen Ultima A-6), disposable cartridges, EMLA cream, falcon tube, neubauer chamber, RBC pipette and sterile syringe. (b) 3.8% sodium citrate (as an anticoagulant was used for platelet rich plasma preparation), 1% ammonium oxalate (as diluent during platelet counting). (c) Centrifugation machine (model: REMI R-8C). RBC: Red Blood Cell.
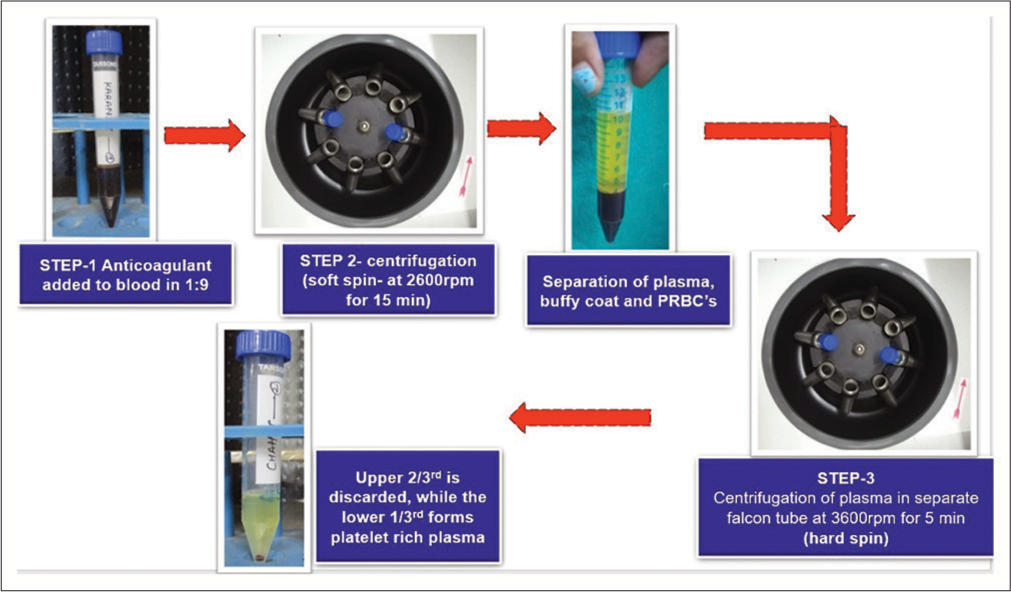
- Steps for preparation of autologous platelet rich plasma using double spin method. PRBC: Peripheral Red Blood Cell.
Procedure of microneedling
After gentle cleansing, topical EMLA cream (Prilox, Uttaranchal Biotech Limited, Dineshpur road, Rudrapur Uttarakhand) (2.5% lignocaine and 2.5% prilocaine) was applied to procedure areas under occlusion for 45–60 min [Figure 5a]. In Group A participants, microneedling was done using dermapen (model: Dr pen Ultima A6, Welshpool WA 6106, Australia) until uniform pin-point bleeding points appeared [Figures 5b and c]. Following the procedure, sunscreen and emollient application were advised. In Group B participants, after noting the baseline platelet count, autologous PRP was prepared with a platelet count 4–7 times the patient’s baseline platelet count, which was confirmed using an improved Neubauer cell counting chamber visualized under a high-definition light microscope. Microneedling (MN) was done until uniform pin-point bleeding points appeared. Just before the application, platelets in PRP prepared were activated using 1 drop of 10% Calcium Chloride. This activated PRP was topically applied over the area and the procedure was repeated. Strict photoprotection after the procedure was advised. A total of three sessions, each separated by 4 weeks were performed.
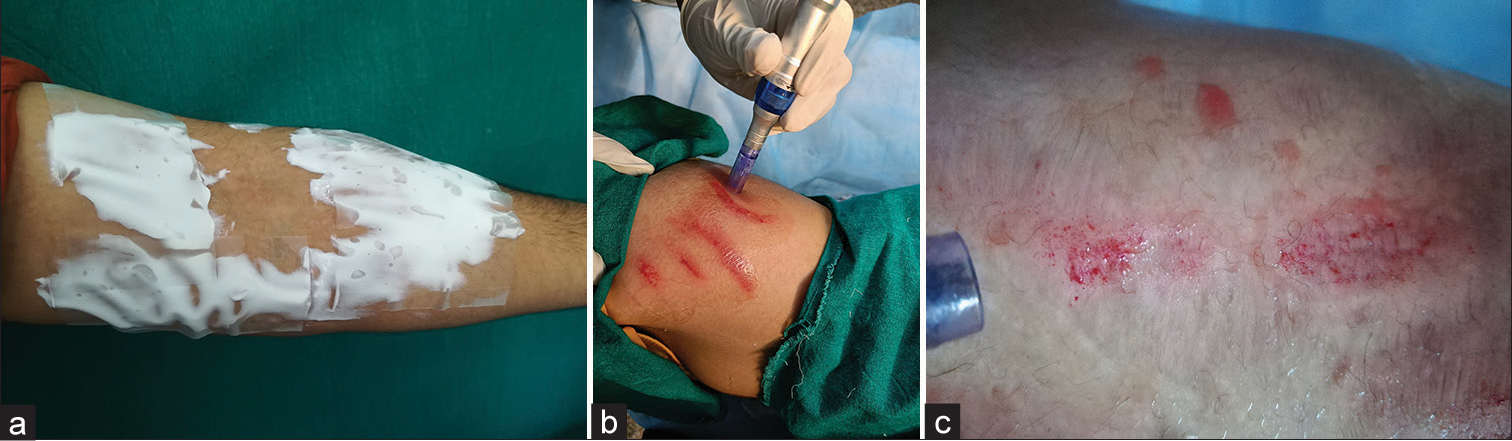
- Steps of procedure (a) EMLA cream was applied on the treatment area 40–45 min before the procedure. (b) Area cleaned with antiseptic solution and microneedling was done on stretch marks (or scar marks) using hand held Dermapen and disposable cartridges. In patients allocated to Group B, autologous platelet-rich plasma was additionally used topically during the procedure. (c) Pin-point bleeding points were considered as the end of the treatment.
Post-procedure follow-up
Study participants were assessed before each session and then 4 weekly till 20 weeks. Thus, 6 times in total, that is, 0, 4, 8, 12, 16, and 20 weeks. The assessment was done for esthetic improvement with (1) clinical photographs, (2) dermoscopy changes, (3) reduction in MSS score, (4) PSS (Not satisfied=1, slightly satisfied=2, satisfied=3, very satisfied=4, and extremely satisfied=5), (5) post-procedure pain score (Visual analog scale 0–10, 0=no pain; 10=worst possible pain), (6) side effects, and (7) global improvement scores at end of 20 weeks (Grade 0: No improvement, Grade I: <30% improvement-mild improvement, Grade II: 31–50% improvement-moderate improvement, Grade III: 51–80% improvement-good improvement, and Grade IV: >81% improvement-excellent improvement).
Statistical analysis was done using statistics software Statistical Package for Social Sciences version 22.0, IBM, USA. P < 0.05 was considered statistically significant.
RESULTS
A total of 30 subjects were evaluated, twenty-eight patients had stretch marks and two patients had post-surgical scars. Among the 30 cases included in the study, 8 (26.7%) were from the age group of 18 to 20 years. Seventeen (56.7%) patients belonged to the age group of 21–25 years, while the rest 5 (16.7%) patients were from the age group of 26 to 30 years. Females constituted 53.3% (n = 16) of the total study subjects. The female-to-male ratio was 1.14: 1.
Excessive weight gain was one of the most common reasons for stretch marks in 11 (36.7%) followed by pregnancy in 5 (16.7%). Other causes included growth spurt, steroid abuse, and gym training in 4 (13.3%) cases each. Among the 2 (6.7%) study participants with surgical scar marks, one had a scar mark on the right forearm and the other on the forehead. In 53.3% (n = 16) of the subjects, lesions were present for 1–2 years, in 36.6% (n = 11) lesions persisted for 3–4 years while in 10% (n = 3) lesions were >5 years old. The abdomen was the most frequently affected site among the study cases and was present in 56.6% (n = 17) of cases with stretch marks. Other sites included the arms in 10% (n = 3) and the back and thighs in 13.3 % (n = 4) cases each. Out of the total 30 study cases, 15 (50%) patients had body mass index (BMI) >25 (Overweight), 14 (46.7%) had a BMI within the normal range whereas 1 (3.3%) patient had a BMI <18.
MSS scoring was evaluated in each study participants at 0, 4, 12, 16, and 20 weeks. In Group A (MN monotherapy), the mean (±standard deviation [SD]) MSS of 12.20 (±1.859) at baseline decreased to a mean (±SD) value of 9.60 (±1.724) at 20 weeks. In Group B (MN+ PRP), the mean (±SD) MSS score at baseline was 11.87 (±1.407) at baseline to 6.87 (±1.834) at the end of 20 weeks [Figure 6]. The comparative results between Group A and Group B show statistically significant findings (P = 0.01) when the decrease in mean MSS score was evaluated [Table 1].
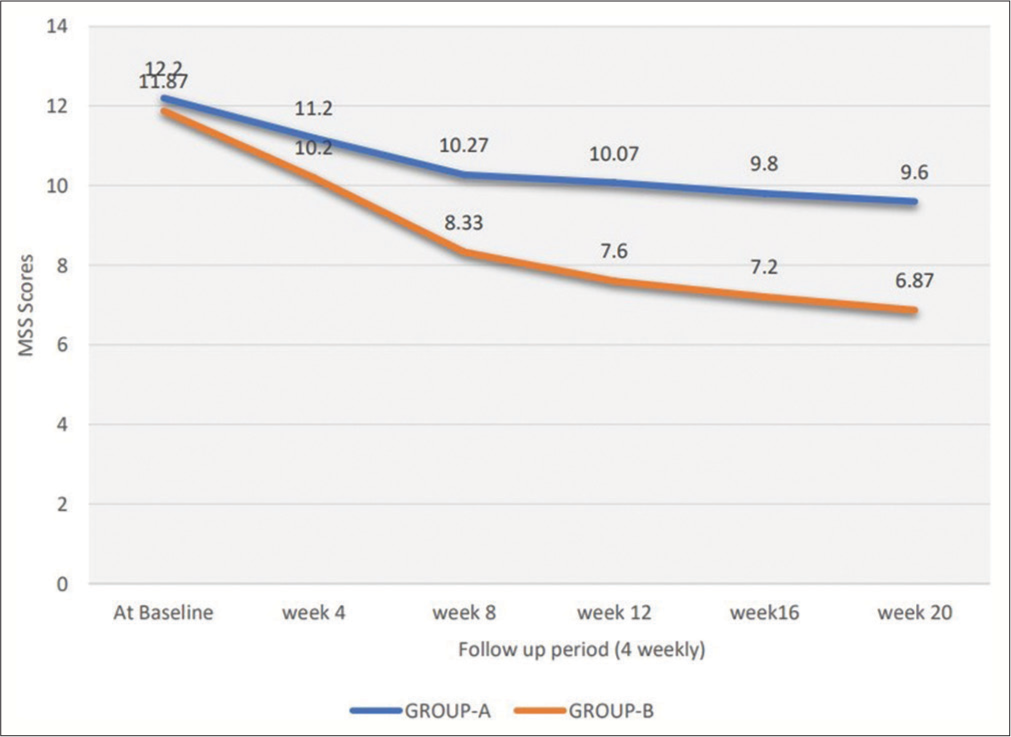
- Graph depicting trends of mean Manchester scar scale scores in Group A and Group B patients over a period of 20 weeks.
| Group A (Microneedling monotherapy) |
Group B (Microneedling with autologous PRP) |
P-value (P-value <0.05 considered statistically significant) |
|
|---|---|---|---|
| MSS Score (Mean±SD) at the end of 20 weeks. | 9.60±1.724 | 6.87±0.834 | 0.01 (t-test applied) |
| Patient satisfaction score (Mean±SD) at the end of 20 weeks. | 2.60 ±0.507 | 4.13 ±0.258 | 0.02 (t-test applied) |
| Global improvement scale (Mean±SD) at the end of 20 weeks. | 1.80±0.414 | 3.07 ± 0.258 | 0.019 (t-test applied) |
| Major side effects | nil | nil | - |
| Side effects documented | Pain: severe intensity=0 moderate intensity=1 (6.6%) participant. Mild intensity=10 (66%) No pain=4 (26.6%) Post-inflammatory hyperpigmentation-n=0 Mild burning sensations: n=2 (13.3%) Mild erythema: n=13 (86.6%) |
Pain: severe intensity=0 moderate intensity=0. Mild intensity=12 (80%) No pain=3 (80%) Post-inflammatory hyperpigmentation n=1 (3.33%) Mild burning sensations: n=3 (20%) Mild erythema: n=14 (93.3%) |
0.383 |
MSS: Manchester scar scale, SD: Standard deviation, PRP: Platelet-rich plasma
In Group A (MN monotherapy), 11 (73.3%) patients were satisfied (grade-3) with the treatment while 4 (26.6%) were only slightly satisfied (grade-2) with the treatment results. While, among the patients enrolled in Group B (MN+PRP), 13 (86.6%) patients were very satisfied (grade-3/4) with treatment, while 2 (13.3%) patients showed extreme satisfaction (grade-5) after 20 weeks follow-up period. In Group A (MN monotherapy), the mean PSS increased from 1.75 (±0.134) at 4 weeks to 2.6 (±0.507) at the end of 20 weeks. While in Group B (MN+PRP), the mean PSS increased from 2.8 (±0.214) at 4 weeks to 4.1 (±0.352) at the end of 20 weeks. On comparison of the two groups, the results were statistically significant (P < 0.05) [Table 1].
Global improvement scores were assessed at the end of 20 weeks. In Group A (microneedling monotherapy), 80% (n = 12) of patients showed moderate (grade-II) to good improvement (grade-III), while 20% (n = 3) showed minimal improvement (grade-I) [Figure 7 and 8]. In Group B (microneedling combined with autologous PRP), 6.6% (n = 1) patients had excellent improvement (grade IV), and 93.3% (n = 14) patients had moderate (grade III) to good improvement (grade II) in the esthetic appearance of the treated lesions [Figures 9-12]. The mean global improvement scale scores at the end of 20 weeks were 1.80 (±0.414) and 3.07 (±0.258) in Group A and Group B, respectively, which showed statistical significance (P = 0.019) [Table 1].
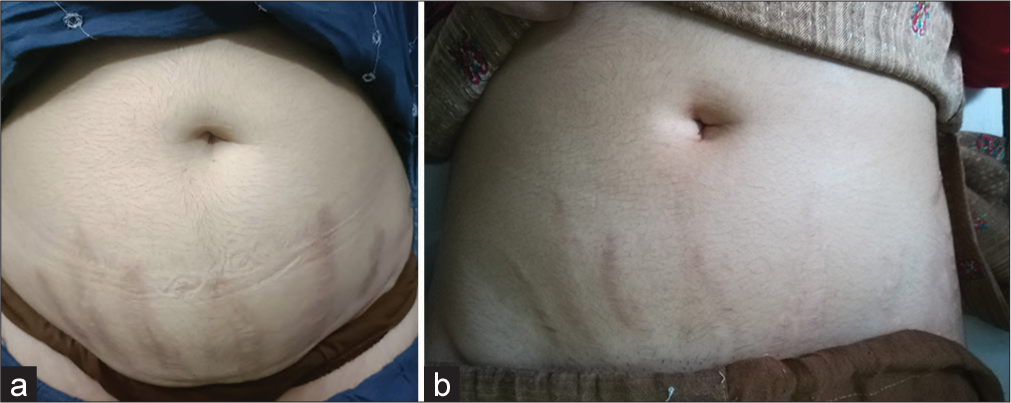
- (a) A 24-year-old female allotted to Group A (Microneedling alone). Clinical appearance of stretch marks over abdomen at the start of the study. (b) Clinical appearance of stretch marks present over abdomen at end of study (20 weeks).
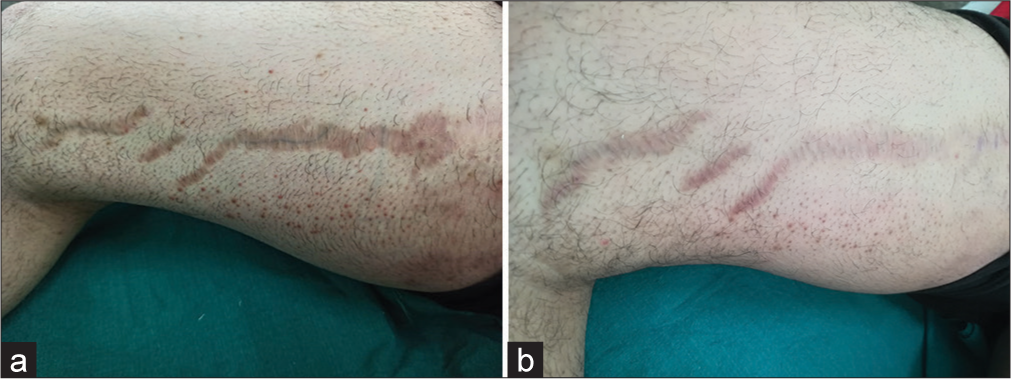
- (a) A 24-year-old male allotted to Group A (Microneedling alone). Clinical appearance of stretch marks over the right thigh (medial side) at the start of the study. (b) Clinical appearance of stretch marks present over the right thigh (medial side) at the end of study (20 weeks).
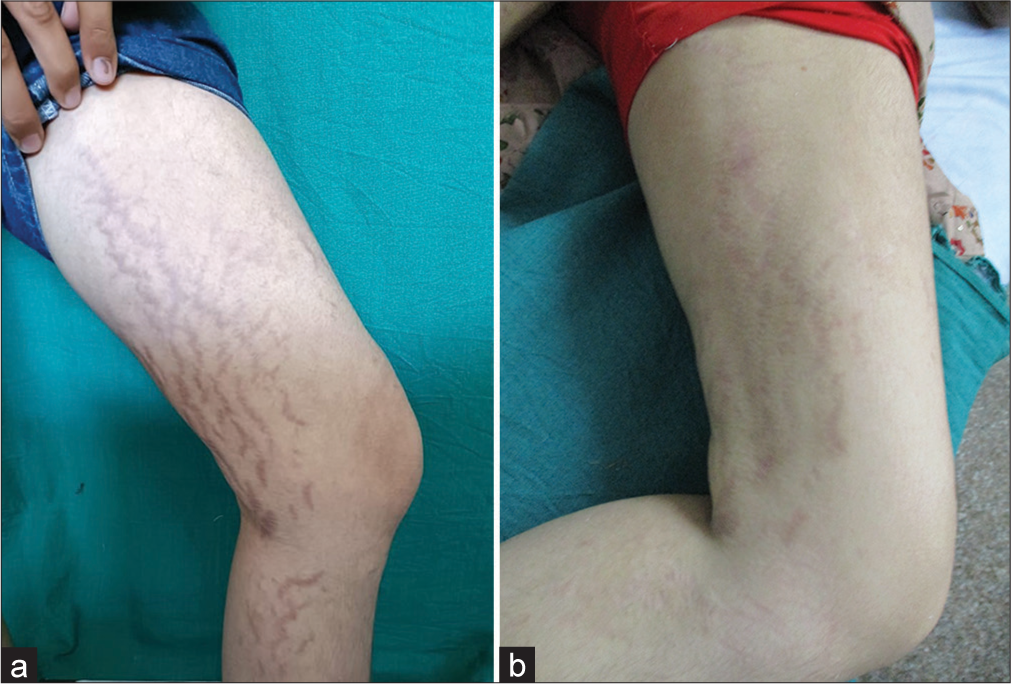
- (a) A 21-year-old female allotted to Group B (Microneedling with autologous platelet rich plasma). Clinical appearance of stretch marks over the left leg at the start of the study. (b) Clinical appearance of stretch marks present over the left leg at the end of study (20 weeks).
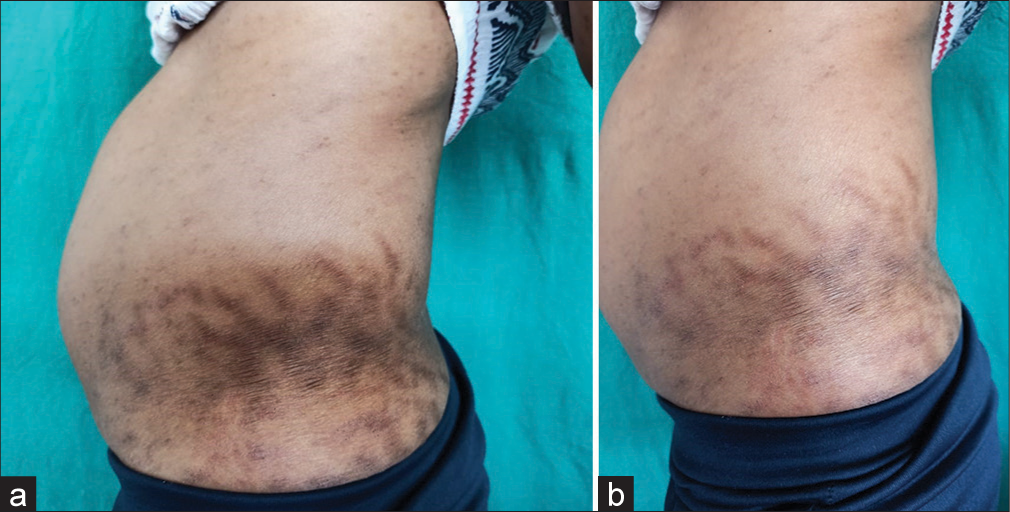
- (a) A 28-year-old male allotted to Group B (Microneedling with autologous platelet rich plasma). Clinical appearance of stretch marks over lateral abdomen at the start of the study. (b) Clinical appearance of stretch marks present over lateral abdomen at end of study (20 weeks).

- (a) A 32-year-old male allotted to Group A (Microneedling alone). Clinical appearance of post-surgery scar marks present over the forehead at the start of the study. (b) Clinical appearance of post-surgery scar marks present over the forehead after 20 weeks (at the end of the study).
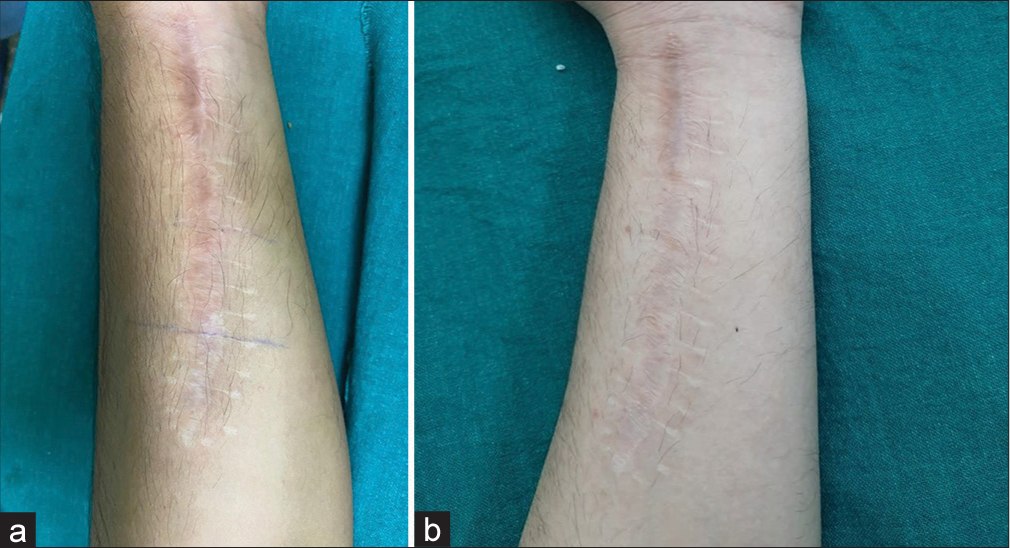
- (a) A 21-year-old male allotted to Group B (Microneedling with autologous platelet rich plasma). Clinical appearance of post-surgery scar marks present over the flexural aspect over the left forearm at the start of the study. (b) Clinical appearance of post-surgery scar marks present over the flexural aspect over the left forearm after 20 weeks (at the end of the study).
No major adverse effect has been recorded with the use of MN or PRP during or after the procedure and during the follow-up period. Minimal side effects included mild pain, erythema, and burning sensation which required no additional treatment and subsided by itself in about 4–6 h [Table 1].
A dermoscopy was done to assess for background erythema, pigmentation, alteration in melanocytic pattern, and atrophy. Among the study, participant’s improvement in terms of decrease in erythema and pigmentation was seen in 60% (n = 9) in Group A and 73.3% (n = 11) cases in Group B was seen. Pigmentation alteration in terms of a decrease in leukoderma was observed in 63.3% (n = 19) cases among the total after 20 weeks [Figure 13 and 14].
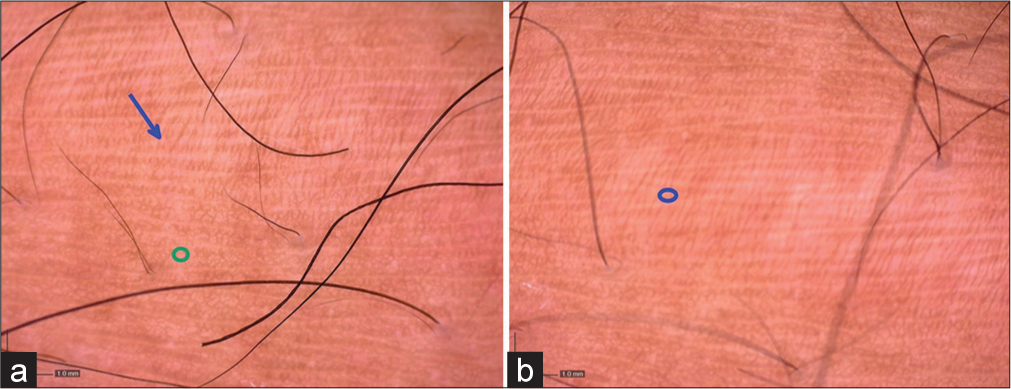
- (a) Dermoscopy findings (magnification: ×35) of the stretch marks at the start of the study showing atrophic skin (blue arrow) with normal adjacent skin (green circle). (b) Dermoscopy findings (magnification: ×35) of the stretch marks at the end of study (20 weeks) show decrease in atrophy and pigmentation (blue circle).
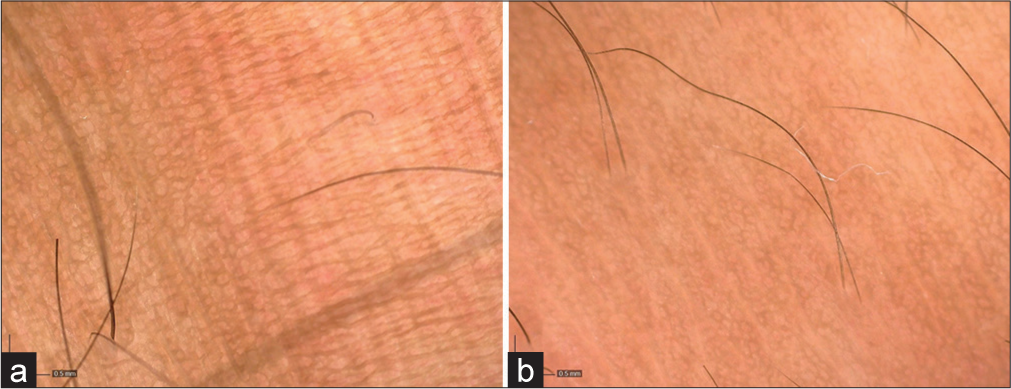
- (a) Dermoscopy findings (magnification: ×63) of the stretch marks at the start of the study showing atrophic skin with loss of pigmentation pattern. (b) Dermoscopy findings (magnification: ×63) of the stretch marks at the end of study (20 weeks) showing improvement in atrophy and pigmentation.
DISCUSSION
Stretch marks and post-surgical scars are residual impressions of underlying healed dermatosis. They tend to persist amidst various therapies. The ultimate goal appears to be a cosmetic improvement in appearance, even though no single therapy is effective. Thus, novel treatment options in combination with microneedling is the requirement of the present scenario that is cost effective with fewer side effects during the follow-up period.
Being a pioneer intervention, literature related to the comparison of quality and degree of improvement in the esthetic appearance of stretch marks and post-surgical scars achieved after microneedling with or without PRP combination is sparse. To the best of our knowledge, no such comparative study has ever been undertaken in this part of our country. Henceforth, we endeavored to compare the outcome of microneedling monotherapy and microneedling in combination with PRP.
In our study, an esthetic improvement based on the reduction of mean MSS score and global improvement scores when compared between Groups A and B showed statistically significant results (P < 0.05). Our results were consistent with Ibrahim et al.7 who used microdermabrasion for collagen induction. The author enrolled 68 patients with stretch marks and compared the outcomes of microdermabrasion monotherapy, microdermabrasion using PRP, and PRP monotherapy. In his study, patients were split into three groups: Group I received intradermal injections of PRP; Group II received microdermabrasion; and Group III received both microdermabrasion and intradermal injections of PRP. Each patient underwent a total of six sessions at 2-week intervals. There was no statistically significant difference in the degree of clinical improvement between Groups I and III (P = 0.701), but there was a significant improvement in both groups (I and III) when compared to Group II (P = 0.001). Results from the study conducted by Park et al.8 were also more or less similar to our study. In his study, microneedling was performed on 16 patients with stretch marks and was evaluated after three treatment sessions at 4-week intervals, using a Quartile grading scale. The author reported excellent improvement in 43.8% of patients and minimal to moderate in the remaining. The two studies mentioned above support the findings of our study and place emphasis on the value of using MN and PRP to treat stretch marks.
Dermoscopy as a tool of evaluation has not been documented in the literature. Assessment of histopathological sections has been investigated by various authors documenting increased collagen deposition after the microneedling procedure. Our study has adopted the novel application of dermoscopy as a non-invasive assessment technique with the least intention to replace the investigational modality.
Several authors have used PSS as an evaluation tool for the treatment of stretch marks. In our study, comparing the mean PSSs after 20 weeks in Group A (2.60 ± 0.507) versus Group B (4.13 ± 0.352) were statistically significant (P < 0.05) concluding that the addition of PRP to microneedling results in a higher satisfaction score. A similar response to the needling therapy for stretch marks has been recorded by Park et al., who reported that 37.5% of patients were highly satisfied, 50% were somewhat satisfied, and 12.5% were unsatisfied after three sessions of procedure done at monthly intervals.8 PSSs using PRP for stretch marks treatment as reported by Ibrahim et al. in their study show that 36.4% of patients were very satisfied, 27.3% satisfied, and 36.4% slightly satisfied after six sessions of PRP in addition to dermabrasion.7 Comparable results have also been reported by Hodeib et al. and Gamil et al. in their respective studies.9,10
The procedure of microneedling is known to be safe and cost-effective with supporting evidence by El-Domyati et al., Majid et al., and Doddaballapu in their studies who have reported no note-able side effects with microneedling except minimal pain and mild erythema.11-13
In our study, out of 30 cases enrolled, in Group A or Group B, only one patient (3.33%) presented with post-inflammatory hyperpigmentation (PIH). No pigment alteration was seen in 29 (96.6%) of cases. Mild burning and pain sensation after the procedure were the complaints of 16.6% (n = 5) patients and 70% (n = 21) patients, respectively. None of the side effects demanded any additional treatment and resolved spontaneously within 4–6 h except for PIH which resolved on its own by 3 weeks. Similar to our study, Hodeib et al. report no major side effects after the use of PRP for the treatment of stretch marks.9
CONCLUSION
To the best of our knowledge, ours is the first study comparing microneedling monotherapy and a combination of microneedling with autologous PRP for the treatment of stretch marks and post-surgical scars.
From this study, it is concluded that the benefit of combining microneedling with PRP is better than microneedling monotherapy for the treatment of stretch marks and post-surgical scars. It can be further stated that this procedure is a safe, efficient, affordable, and simple therapeutic option and can be added to the armamentarium of cosmetic procedures for the treatment of the above dermal scarring conditions.
As collagen remodeling is a gradual process and may continue beyond 20 weeks following collagen induction procedures, it is recommended that a further study with a larger sample size who are followed up for longer periods (about 12 months) is required to identify the ideal modality, agent, and duration of therapy to stretch marks and post-surgical scars effectively.
Authors’ contributions
All authors participated in drafting the work or revising it critically for important intellectual content and provided final approval. Dr Tejinder Kaur: conceptualization, formal analysis and investigation, manuscript revision, drafting of manuscript, intellectual revisions, mentorship, final approval. Dr Sahibpreet Kaur: conceptualization, formal analysis and investigation, manuscript revision, drafting of manuscript, final approval. Dr Permeet Kaur Bagga: conceptualization, drafting of manuscript, final approval. Dr Rakesh Tilak Raj: formal analysis and investigation, drafting of manuscript, manuscript revision, intellectual revisions, final approval. Dr Sandeep Sidhu: formal analysis and investigation, drafting of manuscript, final approval.
Ethical approval
The Institutional Ethics Committee approval is taken prior to the commencement of the study. The Institutional Ethics Committee No. is IEC No-3384/D-26/2020
Declaration of patients consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Ultrasound and 3D skin imaging: Methods to evaluate efficacy of striae distensae treatment. Dermatol Res Pract. 2012;2012:673706.
- [CrossRef] [Google Scholar]
- Percutaneous collagen induction: Minimally invasive skin rejuvenation without risk of hyperpigmentation-fact or fiction? Plast Reconstr Surg. 2008;122:1553-63.
- [CrossRef] [Google Scholar]
- Platelet-rich plasma and its utility in medical dermatology: A systematic review. J Am Acad Dermatol. 2019;81:834-46.
- [CrossRef] [Google Scholar]
- Patient satisfaction and quality of care: A prospective study at outpatient dermatology clinics. Cutis. 2018;102:33-5.
- [Google Scholar]
- Use of patient and investigator global impression scales: A review of Food and Drug Administration-approved labeling, 2009 to 2019. Value Health. 2021;24:1016-23.
- [CrossRef] [Google Scholar]
- Comparison between the efficacy and safety of platelet-rich plasma vs. microdermabrasion in the treatment of striae distensae: Clinical and histopathological study. J Cosmet Dermatol. 2015;14:336-46.
- [CrossRef] [Google Scholar]
- Treatment of striae distensae using needling therapy: A pilot study. Dermatol Surg. 2012;38:1823-8.
- [CrossRef] [Google Scholar]
- Clinical and immunohistochemical comparative study of the efficacy of carboxytherapy vs platelet-rich plasma in treatment of stretch marks. J Cosmet Dermatol. 2018;17:1008-15.
- [CrossRef] [Google Scholar]
- Platelet-rich plasma versus tretinoin in treatment of striae distensae: A comparative study. Dermatol Surg. 2018;44:697-704.
- [CrossRef] [Google Scholar]
- Carboxytherapy for striae distensae: A promising modality. J Cosmet Dermatol. 2021;20:546-53.
- [CrossRef] [Google Scholar]
- Microneedling and its applications in dermatology. Prime Int J Aesthetic Anti Age Med Healthc. 2014;4:44-9.
- [Google Scholar]






