Translate this page into:
A study to determine the efficacy of intense pulse light in vascular mode for topical steroid damaged facies
*Corresponding author: Avani Jatinkumar Shah, Department of Dermatology, Seth G.S. Medical College and KEM Hospital, Mumbai, Maharashtra, India. avanishah28396@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chikhalkar SB, Shah AJ, Chikhalkar GB. A study to determine the efficacy of intense pulse light in vascular mode for topical steroid damaged facies. J Cutan Aesthet Surg. doi: 10.25259/jcas_42_24
Abstract
Objectives:
Misuse of topical corticosteroids on the face has gradually evolved over the years and has now reached phenomenal proportions on account of easy availability, widespread misinformation, and the fairness craze sweeping across the land. Topical steroid-damaged/dependent facies (TSDFs) may present with diffuse erythema, telangiectasia, papules, and atrophy. Current modalities used for the management of TSDF, such as topical tacrolimus and oral antibiotics, have shown a variable response. Intense pulsed light (IPL) systems are economical, have a higher safety margin, and are widely available. The goal of treating vascular lesions with IPL is to raise blood vessel temperature high enough to cause coagulation, leading to destruction and healing with fibrosis. In our study, we exploit these properties of IPL for the management of TSDF.
Material and Methods:
A total of 15 patients of TSDF were recruited and were treated with three sessions of IPL treatments (vascular mode) 3 weeks apart and were assessed based on a clinical score for TSDF, visual analog scale (VAS) for erythema assessed by the physician and patient at the end of 9 weeks.
Results:
There was a significant response with a reduction in clinical score of 5.4 points (P > 0.001) and a reduction in physician and patient-assessed VAS for erythema of 3.47 and 3.73, respectively.
Conclusion:
There is a scarcity of data regarding the efficacy of various treatment modalities for TSDF. Our study establishes IPL (vascular mode) as an innovative emerging modality of treatment.
Keywords
Steroid damaged facies
Intense Pulse light
TSDF
INTRODUCTION
Misuse of topical corticosteroids (TCs) on the face has gradually evolved over the years and has now reached phenomenal proportions on account of easy availability, widespread misinformation, and the obsession with fair skin.1
Many synonyms such as light-sensitive seborrheid, rosacea-like dermatitis, steroid rosacea, steroid dermatitis resembling rosacea, and steroid-induced rosacea-like dermatitis have been used to describe topical steroid damaged/dependent face (TSDF).2 It has been clinically defined as semi permanent or permanent damage to the skin of the face precipitated by the irrational, indiscriminate, unsupervised, or prolonged use of TCs resulting in a plethora of cutaneous signs and symptoms3 TSDF is clinically characterized by centrofacial, perioral, and periocular inflammatory papules and pustules with erythema, telangiectasia, and scaling with atrophy of skin and hypertrichosis.2
While the inherent thinness of the facial skin makes it more susceptible to the side effects of TCs, the clinical picture has been attributed to a combination of dermal atrophy as a result of inhibition of hyaluronic acid and collagen synthesis as well as the local immunosuppression. Its role in inhibiting nitric oxide plays an important role in rebound erythema, which occurs during steroid withdrawal.4
On dermoscopy, various findings have been observed, such as dilated vessels, brown globules, diffuse red areas, white structureless areas, hypertrichosis, white hair and desquamation.5
Previously, various modalities such as topical tacrolimus and tretinoin creams have been tried to manage TSDF; however, they have an increased propensity to irritate. Other agents such as oral antibiotics, platelet-rich plasma and topical vasoconstrictive agents have also been used with a variable response.
The lack of a standardized treatment protocol for the management of TSDF prompts patients with TSDF to undergo a variety of long-term treatments before their symptoms are relieved.6,7
The skin of the face being visible to the whole world is an important aspect of a person’s body image, causing significant psychological distress; hence, these patients are often on the lookout for quick and effective remedies.8
Intense pulse light devices are non-laser high intensity light sources which utilize various cutoff filters to enable its use for various targets.
While using it for TSDF, the aim is to target hemoglobin which acts as a chromophore in its vascular mode, which, in turn, targets the telangiectasias.
In addition, there are studies to show that intense pulsed light (IPL) devices affect the strengthening of the epidermal barrier by increasing collagen synthesis and thus holistically work for steroid damaged facies.9,10
MATERIAL AND METHODS
The study was conducted at a tertiary care hospital for 6 months after obtaining Institutional Ethics approval. Patients were selected based on the inclusion and exclusion criteria.
Patients with the clinical diagnosis of TSDF dermatitis, aged 18–65 years, history of topical steroid application for ≥1 month immediately preceding their presentation, visible telangiectasia and erythema on the face, and patients willing for regular follow-up visits were included in the study after taking informed consent. Patients taking photosensitizing drugs, suffering from any other concurrent illness affecting the face, history of rosacea prior to the use of topical steroids, pregnant or lactating females, and those unwilling to participate in the study were excluded from the study.
A detailed history and examination were performed along with the grading of severity based on the clinical score for steroid dermatitis and grading the erythema based on a visual analog scale (VAS) of 0–10 assessed by the clinician as well as the patient at baseline and 3, 6, and 9 weeks.
The clinical score for steroid dermatitis is a 24-point score taking into consideration eight parameters graded on a severity scale including erythema, papule, edema, dryness, telangiectasia, a sensation of tightness, itching, and burning sensation8 [Table 1].
| 0 | 1 | 2 | 3 | |
|---|---|---|---|---|
| Erythema | Absent | mild | moderate | severe |
| Papule | Absent | mild | moderate | severe |
| Edema | Absent | mild | moderate | severe |
| Dryness | Absent | mild | moderate | severe |
| Telangiectasia | Absent | mild | moderate | severe |
| Itching | Absent | mild | moderate | severe |
| Burning Sensation | Absent | mild | moderate | severe |
| Sensation of tightness | Absent | mild | moderate | severe |
All patients were subject to dermoscopic analysis at the time of initial assessment and every follow-up. If there was the presence of non-follicular and perifollicular gelatinous threads or filaments protruding out of follicular openings in the form of Demodex tails, tablet ivermectin 12 mg single dose was given and started on intense pulse light therapy after 2 weeks. The dosage given was done to avoid IPL-induced exacerbation due to its effect on heat and light-sensitive demodex folliculorum, which is often overgrown in TSDF.
Three sessions of IPL treatments were administered at 3 weekly intervals. To ensure an even contact surface of the treatment tip, a thin coat of coupling gel was used before each session.
A 590 nm vascular filter was used with a fluence fixed at 20/cm2 with four pulses and a discharge interval of 4 msec.
Patients were advised to apply an identical sunscreen and moisturizer and follow strict sun protection.
Final statistics were done using paired t-test and independent t-test using the Statistical Package for the Social Sciences 22.00 with significant P < 0.001.
RESULTS
A total of 15 patients were recruited for the study. The mean age of the patients was 34.2 years (19–51 years), with a female preponderance of 12 females (80%) and 3 males (20%).
We observed that the most common complaints of the patients were burning and erythema, pigmentary alterations, papules, and pustules, with the commonest aggravating factor being sun exposure and heat.
While the majority (50%) of the patients had used TCs on recommendation by friends or family, 3 (20%) patients had used it on advice by quacks and beauticians, with a desire for fair skin and to reduce pigmentation to be the most common reason for the abuse.
Mid-potency steroids in combination creams were the most commonly applied TCs among the patients, with an average duration of TCs used before the onset of symptoms to be 8.9 months.
On dermoscopy, the common findings were linear, serpentine, and branched vessels (93.3%), diffuse red areas (86.6%), and hypertrichosis (86.6%) [Figure 1].
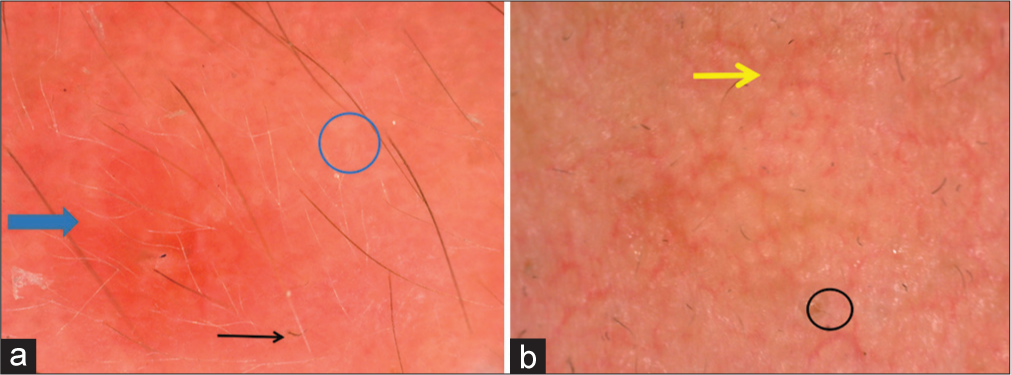
- (a and b) Dermoscopic findings seen as - diffuse red areas (blue arrow), white structureless areas (blue circle), hypertrichosis and white hair (black arrow), branched vessels (yellow arrow), follicular plugging (black circle).
Outcome measures
Patients reported a significant clinical improvement in terms of symptomatic relief in the form of a reduction in burning sensation and irritation as early as 6 weeks.
The improvement was observed with a mean reduction in the clinical score of steroid dermatitis of 1.53 points at 3 weeks, 3.73 points at 6 weeks, and 5.47 points at 9 weeks, which is statistically significant with P < 0.0001 [Table 2].2
| Mean +/-SD | P-value | Mean reduction from baseline | Calculated t value |
95% confidence interval | ||
|---|---|---|---|---|---|---|
| Clinical Score | Baseline | 9.73 +/- 2.63 | <0.001 | |||
| 3 weeks | 8.20 +/- 2.43 | <0.001 | 1.53 | 9.28 | 1.18-1.89 | |
| 6 weeks | 6.00 +/- 2.45 | <0.001 | 3.37 | 14 | 3.16-4.31 | |
| 9 weeks | 4.27 +/- 2.25 | <0.001 | 5.47 | 12.89 | 4.56-6.38 | |
| Erythema by VAS assessed by the physician |
Baseline | 6.40+/- 1.55 | <0.001 | |||
| 9 weeks | 2.93 +/- 1.53 | <0.001 | 3.47 | 8.4 | 2.58-4.35 | |
| Erythema by VAS assessed by the patient |
Baseline | 6.53 +/-1.41 | <0.001 | |||
| 9 weeks | 2.80 +/- 1.26 | <0.001 | 3.73 | 10.83 | 2.99-4.47 |
VAS: Visual analog scale, SD: Standard deviation
Erythema, as assessed by VAS of 0–10 by the patient and the clinician, showed a mean reduction of 3.73 and 3.47, respectively, at the end of treatment at 9 weeks [Figures 2 and 3].

- Marked reduction in erythema and clinical improvement seen from (a) baseline (b) at 6 weeks and (c) 9 weeks. Symptomatic improvement in terms of reduced burning sensation and sensation of tightness seen as early as 6 weeks.

- Significant clinical improvement is seen from (a) baseline, (b) at 6 weeks and (c) at 9 weeks.
DISCUSSION
Intense pulse light devices are non-laser high-intensity light sources that produce non-coherent light of the wavelength 500–1200 nm which utilize various cutoff filters to enable its use for various targets.
The working basis of IPL rests on the principle of selective photothermolysis. While using an IPL device in its vascular mode, the goal is to raise the temperature of the blood vessel high enough to cause its coagulation and destruction, which ultimately leads to the formation of fibrous granulation tissue.
In addition to its effect on telangiectasia, IPL devices have the unique ability to strengthen the epidermal barrier by increasing the collagen synthesis and remodeling of the dystrophic dermal connective tissue.9 This has been confirmed histologically by a study by Zelickson and Kist11, which showed increased synthesis of collagen 1 and 3, procollagen, collagenase, and elastin and increased hyaluronate receptor expression.12
In our study, there was a female preponderance in our study with a ratio of M: F 1:4, which has been replicated in various studies; a study by Rathi13 showed 89% females, while another study by Rather et al.14 showed 65% females. It has largely been attributed to the rising societal pressure and a higher cosmetic concern.
On dermoscopy, the common findings were linear, serpentine, and branched vessels (93.3%), diffuse red areas (86.6%), and hypertrichosis (86.6%).
The mentioned list was similar to the study by Sethi et al.,5 where the most common findings were brown globules (96.2%) and diffuse red areas (92.4%).
While using IPL with a 590 nm vascular filter with a fluence fixed at 20 J/cm2, we found a reduction in VAS for erythema of 3.46 points; this was similar to a study by Maria et al.15 using a 560 nm filter with a mean reduction of 2.93.
While there is a lack of similar studies limited to TSDF, few studies for rosacea have found similar results, such as the study by Papageorgiou et al. for rosacea using a 560 nm filter with a fluence of 24–32 J/cm2 found a 3.5 point reduction in severity of rosacea on a 10 point VAS.12
A study by Kassir et al. using IPL for rosacea with 530 nm and 420 nm with a fluence of 10–30 J/cm2 found an 80% reduction in redness, 78% reduction in flushing, and an improved texture.10
CONCLUSION
IPL devices are economical and are widely available across dermatological clinics due to their unique advantage of using various cut-off filters to treat a multitude of conditions.
Our study establishes IPL as an effective modality for the management of TSDF.
While intense pulse light has been used frequently for rosacea, there is a shortage of data on its use in TSDFs.
On the basis of the findings of this study, it is worth conducting a large randomized controlled trial to evaluate the safety and efficacy of intense pulse light for the management of TSDF.
Authors’ contributions
Dr Siddhi Chikhalkar: Conceptualization, conceived and designed the analysis, data collection and supervision. Dr Avani Shah: Study design, Data collection, Data analysis and statistics, writing and editing the paper. Dr Gauri Chikhalkar: Contributed to data collection and analysis.
Ethical approval
The research/study approved by the Institutional Review Board at IEC Seth GSMC and KEM hospital, number EC-OA- 154/2023, dated December 02, 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Topical steroid damaged/dependent face (TSDF): A study from a tertiary care hospital in Eastern India. Indian J Dermatol. 2018;63:375-9.
- [CrossRef] [Google Scholar]
- Steroid-induced rosacea: A clinical study of 200 patients. Indian J Dermatol. 2011;56:30.
- [CrossRef] [Google Scholar]
- Steroid dermatitis resembling rosacea: A clinical evaluation of 75 patients. ISRN Dermatol. 2013;2013:491376.
- [CrossRef] [Google Scholar]
- Dermoscopy of topical steroid damaged/dependent face. Indian Dermatol Online J. 2018;9:286-7.
- [CrossRef] [Google Scholar]
- Dermoscopy of topical steroid-dependent or damaged face: A cross-sectional study. Indian J Dermatol Venereol Leprol. 2021;88:40-6.
- [CrossRef] [Google Scholar]
- Topical steroid-dependent face: Response to xylometazoline topical. Indian J Drugs Dermatol. 2017;3:87.
- [CrossRef] [Google Scholar]
- Successful treatment of corticosteroid-induced rosacea-like dermatitis with platelet-rich plasma mesotherapy: Report of seven cases. Dermatol Ther (Heidelb). 2021;11:615-23.
- [CrossRef] [Google Scholar]
- Quality of life in patients with facial steroid dermatitis before and after treatment. J Eur Acad Dermatol Venereol. 2008;22:663-9.
- [CrossRef] [Google Scholar]
- Intense pulsed light for the treatment of Rosacea and Telangiectasias. J Cosmet Laser Ther. 2011;13:216-22.
- [CrossRef] [Google Scholar]
- Effect of pulsed dye laser and intense pulsed light source on the dermal extracellular matrix remodeling. Lasers Surg Med. 2000;12(Suppl):17.
- [Google Scholar]
- Treatment of rosacea with intense pulsed light: Significant improvement and long-lasting results. Br J Dermatol. 2008;159:628-32.
- [CrossRef] [Google Scholar]
- Abuse of topical steroid as cosmetic cream: A social background of steroid dermatitis. Indian J Dermatol. 2006;51:154-5.
- [CrossRef] [Google Scholar]
- A clinicoepidemiological study on topical steroid misuse in a tertiary-care hospital in North India and the role of dermoscopy as a non-invasive diagnostic modality. Our Dermatol Online/Nasza Dermatol Online. 2022;13:380-6.
- [CrossRef] [Google Scholar]
- Effect of intense pulsed light on topical steroid-dependent facial dermatitis. J Pak Assoc Dermatol. 2018;28:139-45.
- [Google Scholar]







