Translate this page into:
Otoplasty for moderately severe constricted ear deformity
*Corresponding author: Mohammad Ali Bin Mat Zain, Department of Plastic and Reconstructive Surgery, Hospital Kuala Lumpur, Jalan Pahang, Kuala Lumpur, Malaysia. alim1587@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Yii RS, Chai SC, Wan Sulaiman WA, Mat Zain MA. Otoplasty for moderately severe constricted ear deformity. J Cutan Aesthet Surg. doi: 10.4103/JCAS.JCAS_161_22
Abstract
Constricted ears showed a spectrum of deformities confined to the upper third of the ear. Characteristically, constricted ears presented with four anatomical features including helical lidding, protrusion, decreased ear size, and low ear position. Based on these features, Tanzer and Cosman had classified the deformities into groups and proposed treatment to each group. Numerous surgical techniques in correction of constricted ears had been described in the previous literature. We demonstrated a simple one-stage modified Chong-chet technique via posterior approach consisting of anterior cartilage scoring, mastoid hitch, and an inverted triangular supraauricular skin incision in the surgical correction of a moderately severe Tanzer IIA constricted ear deformity with satisfactory outcome. In addition, the details of surgical techniques including its benefits, shortfalls, and outcomes were reported, and literature review on surgical approach to moderately severe constricted ear deformities were shown.
Keywords
Mastoid hitch
Moderately severe constricted ears
Modified chong-chet technique
Tanzer IIA
INTRODUCTION
Constricted ear represented a spectrum of deformities involving the superior third of ear that was attributed to a relative deficiency of helical circumference to scapha. Recognizing the heterogeneity of the deformities, Tanzer classified constricted ear into three categories—Groups I, IIA, IIB, and III and proposed surgical approaches to each group of deformities [Table 1].1 Group IIA deformity was defined as the presence of a significant compression of both the helix and scapha with obvious loss of vertical height not requiring additional soft tissue coverage.
| Constricted ear deformities | Descriptions | Proposed treatment |
|---|---|---|
| Group I | Involvement of helix only | Limited resection of the hooding without any significant cartilage manipulation |
| Group IIA | Involvement of helix and scapha; No supplemental skin needed at the margin of auricle | Cartilage expansion and skin redraping |
| Group IIB | Involvement of helix and scapha; supplemental skin needed at margin of auricle | Skeletal expansion and introduction of soft tissue for coverage |
| Group III | Extreme cupping deformity, with involvement of the helix, scapha, antihelix, and conchal wall | Unfurl and use the remnants for the superior and middle thirds and reconstruct the remainder with contralateral conchal cartilage. Some authors regarded this as a form of microtia requiring autologous reconstruction with rib cartilage graft |
Numerous surgical techniques utilizing cartilage expansion approach had been described for the correction of moderately severe constricted ear deformities over the years [Table 2]. All of which shared a common goal in achieving elongation of the upper third of the auricle. We illustrated a case of group IIA constricted ear deformity that was approached surgically using modified Chong-chet technique and mastoid hitch, without the need of cartilage expansion.
| Authors | Techniques | Description |
|---|---|---|
| Ragnell A (1951)2 | Cartilage splitting technique | The lidded cartilage was split into several transversely oriented interdigitating leaves followed by pulling apart the leaves for expansion and suturing the tips together |
| Stephenson KL (1960)3 | Radial incision technique | Multiple radial cartilaginous incisions were made to expand the cartilage in a fan-shaped fashion that was held by a rib cartilage graft |
| Tanzer RC (1975)1 | Banner flap | The helical overhang was incised from the helix but left attached superiorly at the helical crus followed by advancement and resuturing of flap onto the cut edge of the helix, and thus increasing height and removing the helical curl |
| Tanzer RC (1975)1 | Double banner flap | Two interdigitating flaps were created from the helical overhang with one attached superiorly and the other inferiorly. Both flaps were turned 180 degrees, and their tips were sutured together to form a new helical arch. The resulting cartilage defect was filled with a conchal cartilage graft |
| Cosman B (1978)4 | Floating cartilage technique | Freed helical rim was advanced and rotated superiorly. Mustardé mattress sutures were placed between the concha and scapha to recreate antihelical tubing, while mastoid hitch involved suturing between posterior aspect of neohelix and mastoid fascia to prevent the recurrence of the cupping deformity |
| Elsahy NI (1990)5 | Antihelical cartilage flip-flap | The lid-like turned down cartilage was excised, and a superiorly based cartilage flap was turned upward 180° to be inset into the fossa triangularis to create height and increased the area of the scapha |
| Park C (2000)6 | Tumbling concha-cartilage flap technique | A superiorly based rectangular or T-shaped cartilage flap was raised and tumbled backward through a tunnel under the postauricular skin. The tip of the tumbling flap was fixed to the lidded helix or scapha. The recoiling forces exerted from the flap’s conchal aspect enabled the hooded helix to be in a normal, erect anatomical position |
| Al-Qattan MM (2005)7 | Antihelical recreation and excision of lidding | Antihelix was recreated using Mustardé-type mattress sutures followed by excision of the lidding and mastoid hitch |
| Ho et al. (2006)8 | Reverse conchal cartilaginous graft | The conchal graft was harvested, trimmed to an appropriate size, reversed so that the anterior surface faced posteriorly, and sutured to the unfurled antihelix to support the corrected ear |
CASE REPORT
The patient was a 6-year-old boy who had presented with group IIA left constricted ear deformity since birth with features of superior lidding, protrusion, vertical height difference by 1.5 cm, smaller ear size, and low ear position [Figure 1]. The child had left otoplasty after consent was obtained from his parent.

- Pre- and postoperative comparison showed good outcome at 6 months post repair of left constricted ear: (a) Preoperative, posterior view showed marked vertical height difference by 1.5 cm and smaller ear size. (b) Preoperative, posterior view showed slight reduction in vertical height by 5 mm and increased ear size. (c) Preoperative, lateral view showed superior lidding of the helix with absent antihelical fold. (d) Postoperative, lateral view showed correction of superior helical lidding with increased vertical height, more superiorly placed ear position and antihelical fold visualized. There was a mild degree of lidding at the anterior helix post correction. (e) Preoperative, anterior view showed a marked vertical height difference by 1.5 cm with superior lidding and protrusion of left ear. (f) Postoperative, anterior view showed an improved vertical height and corrected superior lidding and protrusion of the left ear.
Intraoperatively, the affected ear was folded back to its normal position revealing an antihelical fold. The height of antihelical fold was marked with Bonney’s blue using a needle [Figure 2a]. Several passes of needle at four to five places at height of the antihelical fold through the full thickness of the ear had been performed. With each pass of needle, the needle tip was inked and withdrawn to tattoo the cranial aspect of antihelical cartilage.
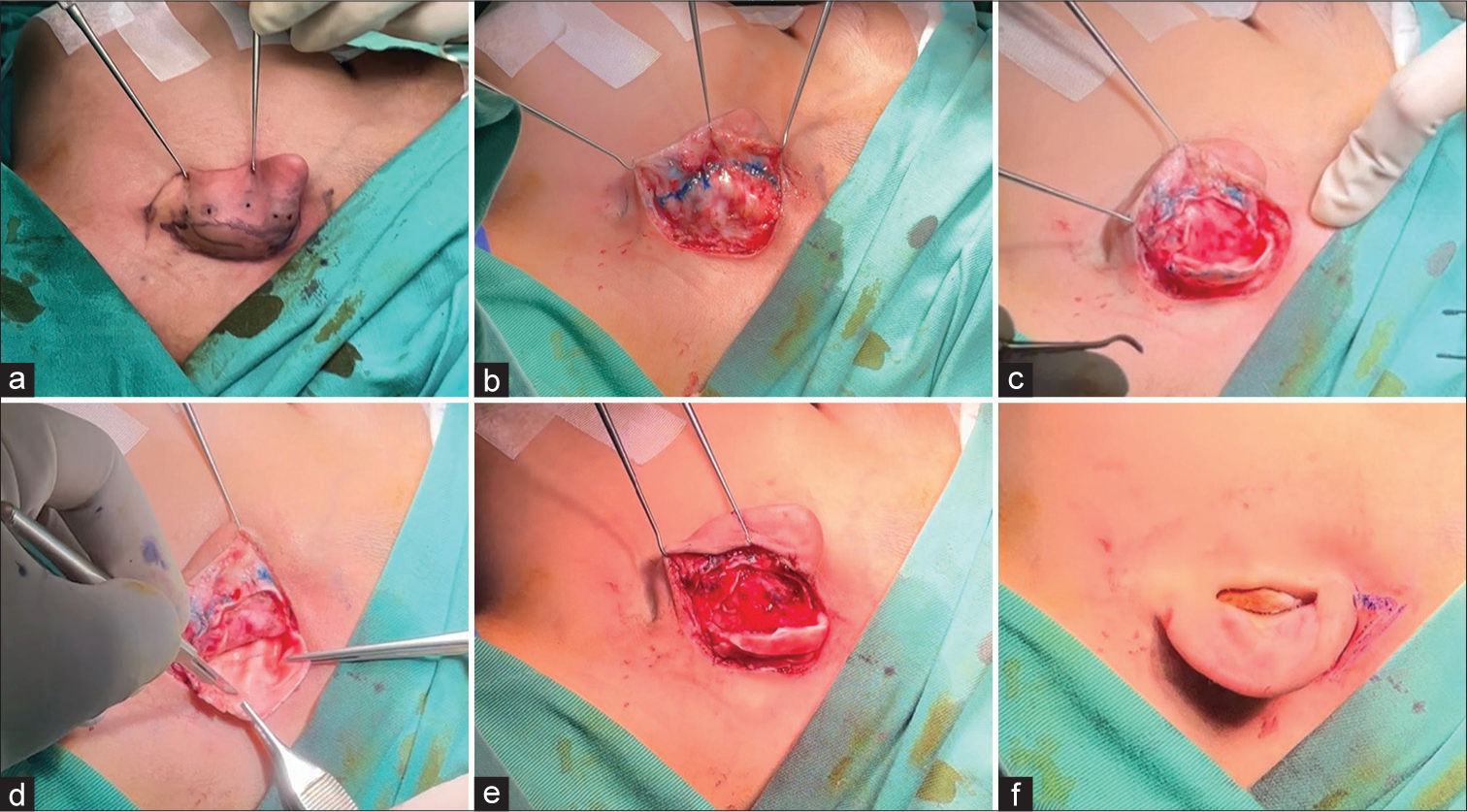
- Otoplasty techniques: (a) Ear was folded back to form antihelical fold and the height of antihelical fold was tattooed with Bonney’s blue using a needle. An elliptical post-auricular skin incision was designed. (b) Perichondrium with the previous tattoo marking visualized. (c) Full thickness cartilage incision made along the scapha, preserving at least 6 mm of helical rim to maintain structural integrity. Anterior surface of cartilage was degloved of its skin and perichondrium. (d) Multiple superficial curved scores were made in the cartilage along the proposed antihelix to break the outer layer of cartilage. (e) The cartilage folded by virtue of these parallel but superiority diverging cuts, thus forming a new antihelical fold. The neohelix was sutured to the mastoid fascia using Monosyn 6/0 (mastoid hitch) as means to maintain helical elevation and prevent recurrence. (f) An inverted triangular incision was made at the supra-auricular region, which was in continuity with the superior edge of the postauricular incision. Approximation between the two created an increased vertical height and correction of helical lidding.
An elliptical post-auricular skin incision [Figure 2a] was sited internal to the previously tattooed dots and marked. Skin on both aspects was infiltrated with local anesthesia containing adrenaline that would facilitate hydro-dissection separating skin from the cartilage and hemostasis. Skin and its attached soft tissues were excised down to the perichondrium. Posterior skin flap had been raised until the mastoid fascia was exposed.
Tattoo marks on the posterior aspects of cartilage were visualized [Figure 2b]. A full-thickness incision was made through the cartilage following the tattoo marks as the guide, beginning from the superior crus to the tail of antihelix [Figure 2c]. The skin overlying the cartilage was then carefully dissected. Once the anterior surface of cartilage had been exposed adequately, the cartilage was scored anteriorly by making a series of partial thickness parallel incision on the cartilage [Figure 2d]. The cartilage folded by virtue of these parallel but superiority diverging cuts, thus forming a new antihelical fold [Figure 2e]. The neohelix was sutured to the mastoid fascia using Monosyn 6/0 as means to maintain helical elevation and prevent recurrence [Figure 2e]. Increment in the vertical height of auricle had been achieved through an approximation between an inverted triangular incision at supra-auricular region and superior edge of postauricular incision [Figure 2f]. The skin closure was performed with Monosyn 6/0. Paraffin-oil gauze and flavine wool dressing were molded into the concavities of the fold followed by gauze overdressing and immobilization with crepe bandage.
Postoperative course was smooth with no complications. Upon review at 6 months post-operatively, the postauricular scar appeared to be optimal [Figure 1d]. The antihelical fold was well formed and prominence component had been corrected [Figure 1d and f]. The superior lidding had been markedly improved except at the anterior helix near to helical radix [Figure 1d]. In addition, the size of affected ear appeared to be close to that of contralateral normal ear with slight discrepancy of vertical height [Figure 1b and f]. There was no recurrence and both the patient and his parent felt satisfied with the outcome.
DISCUSSION
The present case has demonstrated the feasibility of ChongChet technique9 in the surgical correction of constricted ears. A new antihelical fold was formed by virtue of a series of partial thickness parallel incision on the anterior surface of cartilage. The superior crus of newly formed antihelix folded upward and forward and thus correcting the helical hooding as it forced the helix to stand up.10 Additionally, it also aided in correcting the prominence due to the flattening or absence of antihelix.11 Several modifications to the conventional Chongchet technique had been demonstrated in this case. First, the addition of mastoid hitch, where the perichondrium of neohelix was sutured to the mastoid fascia, served to maintain the height and shape of the neohelix.12 Moreover, the tightening of the sutures assumed an adaptic role in achieving a desired bending or contour of neohelix.13 The mastoid hitch mimicked the role of auricularis superior muscles where it acted as an antigravity device that would prevent recurrence of the lidding deformity.12 Second, an inverted triangular incision had been made at the supra-auricular region. The approximation between the supraauricular inverted triangular incision and the superior edge of the postauricular incision enabled an elevation of helical rim and increment in the vertical height. The good outcome obtained in this case corroborated with the findings from studies using anterior cartilage scoring as one of the combination techniques for correction of type IIA deformities.12,14
The cartilage expansion techniques utilizing various cartilage transections or flaps were technically more complicated and tedious, frequently required anterior skin incision, and might need additional cartilage grafts and the use of local skin flaps to cover the expanded upper ear cartilage.6,8,15 On the contrary, our modified Chong-chet technique was simple, single-stage, and utilize a posterior approach. In addition, it had addressed the protrusion, superior lidding, and vertical height increment of the constricted ear deformity without the need of intrinsic cartilage modification or excision that would possibly weaken the structural integrity of cartilage or create donor site morbidity. Nonetheless, there remained mild superior lidding at the anterior helix with slight reduction of vertical height following surgical correction with our technique. Second revisional surgery with V-Y advancement of the helical root might solve the issue, which was offered to his parent. However, the parent was very satisfied with the current outcome and not keen for further revisional surgery.
CONCLUSION
We had demonstrated the feasibility of a simple one-stage modified Chong-chet technique with mastoid hitch and inverted triangular supra-auricular skin incision in correction of moderately severe Tanzer IIA constricted ear deformity with satisfactory outcome.
Authors’ Contributions
All the authors contributed to the research study. Raymond Shi Liang Yii: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Siew Cheng Chai: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Wan Azman Wan Sulaiman: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Mohammad Ali Bin Mat Zain: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Correction of a lop ear type deformity. Plast Reconstr Surg. 1960;26:540-5.
- [CrossRef] [Google Scholar]
- Technique for correction of lop ear. Plast Reconstr Surg. 1990;85:615-20.
- [CrossRef] [Google Scholar]
- Classification and algorithmic management of constricted ears. Plast Reconstr Surg. 2016;137:1523-38.
- [CrossRef] [Google Scholar]
- An alternative approach for correction of constricted ears of moderate severity. Br J Plast Surg. 2005;58:389-93.
- [CrossRef] [Google Scholar]
- Innovative technique for correction of the congenital lop ear. J Plast Reconstr Aesthetic Surg. 2006;59:494-8.
- [CrossRef] [Google Scholar]
- A simple, direct correction of the constricted ear. Br J Plast Surg. 1988;41:619-23.
- [CrossRef] [Google Scholar]
- Otoplasty: A modified Chong-Chet technique with positive long-term results. Medicine (Baltimore). 2021;100:e27554.
- [CrossRef] [Google Scholar]
- 5-year series of constricted (lop and cup) ear corrections: Development of the Mastoid Hitch as an adjunctive technique. Plast Reconstr Surg. 1998;102:2325-32.
- [CrossRef] [Google Scholar]
- Otoplasty: A modified anterior scoring technique. Facial Plast Surg. 2004;20:277-85.
- [CrossRef] [Google Scholar]
- Reconstruction of moderately constricted ears by combining V-Y advancement of helical root, Conchal cartilage graft, and Mastoid Hitch. Eplasty. 2016;16:e19.
- [Google Scholar]






