Translate this page into:
Smart PDOs™ and the Cartesian Technique™: A milestone in facial rejuvenation with bioactive scaffolds
*Corresponding author: Dubraska Violeta Suarez-Vega, Department of Research, University of Los Andes, Faculty of Dentistry, Dental Research Center, Merida, Venezuela. dubraskasuarez.ula@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Velazco de Maldonado GJ, Suarez-Vega DV, Miller-Kobisher B, Garcia VJ. Smart PDOs™ and the Cartesian Technique™: A milestone in facial rejuvenation with bioactive scaffolds. J Cutan Aesthet Surg. 2024;17:292-306. doi: 10.25259/jcas_191_22
Abstract
Objectives:
Evaluate the controlled release of silicon from smart polydioxanone suture (Smart PDOs™) and the clinical effect of the Cartesian Technique™ in face lifting.
Material and Methods:
This study was preclinical and clinical trials randomized, uncontrolled, and phase I carried out. Preclinical trials included instrumental analysis of silicon-enriched sutures by light microscopy, electron microscopy, and Ultraviolet-visible (UV-vis) spectroscopy. The clinical trial included 35 patients with primary and secondary rhytides, grade I lipomatosis, and grade I deflation. Polydioxanone (PDO) sutures are inserted following the Cartesian Technique™, a vectorial lift from the intersection of the Cartesian planes of the face. Once the cannulas were inserted with the PDO thread, 0.1 mL of organic silicon was dosed. Turgidity was examined by the pinch test of skin turgor. To measure the position of flaccid or deflated tissues, the scale used was the deflation scale.
Results:
The controlled release of organic silicon from the PDO sutures was verified. Its clinical application revealed that after 8 days the improvement in turgidity, wrinkle reversal, and flaccidity tightening was maintained in 100% of the sample. At 15 days, reversal of rhytides was observed, softening of deep furrows in 80%, and the initial turgor and skin tightening maintained without deflation in 90% of cases. Histopathological findings reveal that silicon synergistically potentiates the tissue effect of the PDO suture, generating greater biostimulation of fibroblasts with better quality collagen fibers, greater restructuring and redensification of the skin, and avoiding the late inflammatory response.
Conclusion:
The Cartesian Technique™ with Smart PDOs™ is an effective protocol for skin replenishment that enhances cell biostimulation through the release of bioactive drugs.
Keywords
The Cartesian Technique™
Smart PDOs™
Facial rejuvenation
Polydioxanone thread lifts
Control release sutures
INTRODUCTION
One of the biggest challenges in facial rejuvenation is reversing rhytids or loss of definition of the facial contour. The results are not always as expected, because the deflation (fall, flaccidity, and subdermal displacement) that usually accompanies deep rhytides requires an effective tightening that is difficult to achieve without surgery.
Subdermal Polydioxanone (PDO) threads typically have a subtle and transient lifting effect for deflation. Its effect could be enhanced if PDO sutures are used as regenerative scaffolds. Polydioxanone has already been used as biomimetic support structures for cell cultures and grafted in vivo to repair damaged tissues or organs.1
The potential of PDO as a regenerative scaffold is due to its mechanical properties comparable to the structural components of the extracellular matrix.1 Its use in tissue engineering has increased since it allows the design of scaffolds in the form of nanoparticles, nano micelles, or nanofibers, important forms for the controlled administration of drugs and genes.2
In addition, PDO has a shape memory property, providing shape recovery and resistance to torsion, which extends its tensor effect once inserted into the dermis.3 PDO has been studied in tissue augmentation and regeneration. Histologically, type III collagen was found to be replaced by type I collagen in the scaffold. Surrounding cells infiltrated the scaffold, inducing tissue regeneration.4
Due to these properties, polydioxanone monofilament and multifilament scaffolds are useful for stimulating tissue remodeling in aged skin, promoting collagen synthesis, and partial restoration of dermal matrix components.5 Their use as support or niche structures or matrices can be successful in allowing cell proliferation, and as vehicles for bioactive agents that promote the exchange of nutrients and precursor substances during the development of new tissues.6
This principle is what has driven our idea of using PDO scaffolds enriched with other substances that give them such a bioactive character, to optimize the regenerative process or lead it toward a specific tissue response.
However, a large part of the success of PDO scaffold therapy depends not only on its properties as an intelligently controlled drug release system but also on a clinical protocol that organizes the distribution of clamping forces, giving each suture an optimal direction. Moreover, the sense of the traction force and altogether facial mesh from the subcutaneous plane provides biomechanical support, prolonging the lifting effect.
Under these precepts, we propose the Cartesian Technique™, a new and effective technique that reverses rhytids and facial deflation, using Smart PDOs™ intelligent scaffolds, which exert controlled release while promoting facial tightening.
Hypothesis
“The implantation of enriched polydioxanone sutures smart polydioxanone suture (Smart PDOs™) following a vector order of forces in a facial Cartesian tracing (the Cartesian Technique™), will improve the clinical performance of the sutures and optimize the results of the treatment of rhytides and skin deflation.”
MATERIAL AND METHODS
In this quantitative, correlational research, with an experimental design, the effect of subcutaneous implantation of Smart PDOs™ using the Cartesian Technique™ (independent variable) on tissue restructuring (turgor, removal of roughness, and skin tightening) was studied. The clinical performance of the suture represents the dependent variable.
Preclinical trials : Development of smart PDOs™
To verify the feasibility of polydioxanone sutures as scaffolds for the controlled release of cosmeceutical drugs, preclinical laboratory tests were performed by subjecting PDO sutures to capillarity, biodegradation, and controlled release tests.
PDO sutures used in facial tightening are known to be polymeric biomaterials that slowly biodegrade through hydrolysis (cite article biodegradation). That is why, before proposing their use as bioactive scaffolds for controlled release, it had verified whether the suture had the capillarity to be enriched with cosmeceutical active ingredients, that is, the ability to hold liquid substances in its structure without said wetting producing biodegradation immediate of the PDO suture.
To do this, we started with the instrumental analysis of the PDO suture impregnated with the active ingredient, evaluating the absorption of fluids by observation by optical microscopy and scanning electron microscopy (SEM). Controlled release analyzed by ultraviolet-visible (UV-vis) spectroscopy.
Sample
Three specimens were studied: A suture for the control-control group (PDO), a PDO suture embedded in distilled water for the control group (PDO H2O), and a PDO suture embedded in Organic Silicon for the experimental group (PDO C-Si).
Materials
Organic silicon at 1% w/v (Methylsilanol Mannuronate) in Organic Silicon® brand solution (SIMILDIET laboratories; Zaragoza Spain) vial of 5 mL
JBP V-Lift Premium® brand Poly (dioxanone) monofilament (JBP KOREA CO., LTD.), with a 23G (4– 0) caliber diameter of 150 mm length
Ultrapure water 18 MΩ•cm
BD™ Syringe with Luer Slip hypodermic syringes (BD plastipak® New Jersey-United States) of 1 mL with an interchangeable needle to subtract the peptide
Eppendorf™ (Hamburg-Germany) DNA LoBind Polypropylene Microcentrifuge Tubes 3 mL.
Optical microscope observation
At the end of the evaluation period (24, 48, and 72 h after immersion), the PDO suture segments were placed on slides and observed under a Nikon® reflection optical microscope at ×4 and ×10.
Scanning electron microscopy (SEM)
The PDO suture embedded with Arg for 1 min, after drying in the environment, was fixed with a 3:3 mixture at 4°C, for 24 h for SEM observation (3% formaldehyde + 3% glutaraldehyde in 0.1 M cacodylate buffer), pH6.3. Subsequently, the alcoholic dehydration, desiccation, and metallization of the samples were carried out for observation under a scanning electron microscope (Hitachi S-2500).
CSi release rate from PDO
The PDO thread with Organic Silicon (CSi) and the PDO suture without medication were analyzed in a UV-vis spectrophotometer to determine their controlled release capacity and to detect if there is degradation or loss of thread mass.
The prolonged release of the drug was assessed by recording the rate of release of CSi from the PDO suture and, a curve of concentration released over time (at 5, 15, 30, 60, and 2400 min or 24 h) was constructed.
Design of the “the Cartesian Technique™” protocol
During facial aging, two major phenomena contribute to the loss of firmness of the soft tissues of the face: lipomatosis and deflation. Lipomatosis refers to the increase in facial volumetric weight due to fat infiltration in adipose compartments of the middle and lower third of the face. Deflation refers to skin flaccidity or laxity in which the skin results and falls forming deep furrows and causing loss of mandibular contour.7
The Cartesian Technique™ clinical protocol is a set of facial lifting techniques designed from the application of spatial geometry to the face, which is part of our paradigm called facial morpho geometric analysis.8
The theory that underlies the Cartesian Technique™ implies that to achieve a more effective tightening of the aged face, before intervening with facial support sutures, dermal repositioning must be planned. This plan is based on a logical system of redistribution of forces, which allows for optimizing the results of a facelift with threads while improving the clinical performance of the suture with the use of Smart PDOs™.
Our theory proposes that there are unalterable or visually easy to locate craniometric points, known as anthropometric landmarks [Figure 1], which are useful for locating and tracing horizontal and vertical planes. The following points are considered anthropometric milestones: Trichion, glabella, nasion, endocanthon and exocanthon (internal and external canthus, which form the ocular intercanthal plane), pupillary, infraorbital, subnasal, stomion (between the upper and lower lip, through which the bicommissural plane is drawn) pupillary, infraorbital, subnasal, stomion (between the upper and lower lip, through which the bicommissural plane is drawn), gnathic (or mental point) and gonion (at the level of the gonial angle of the mandible).”
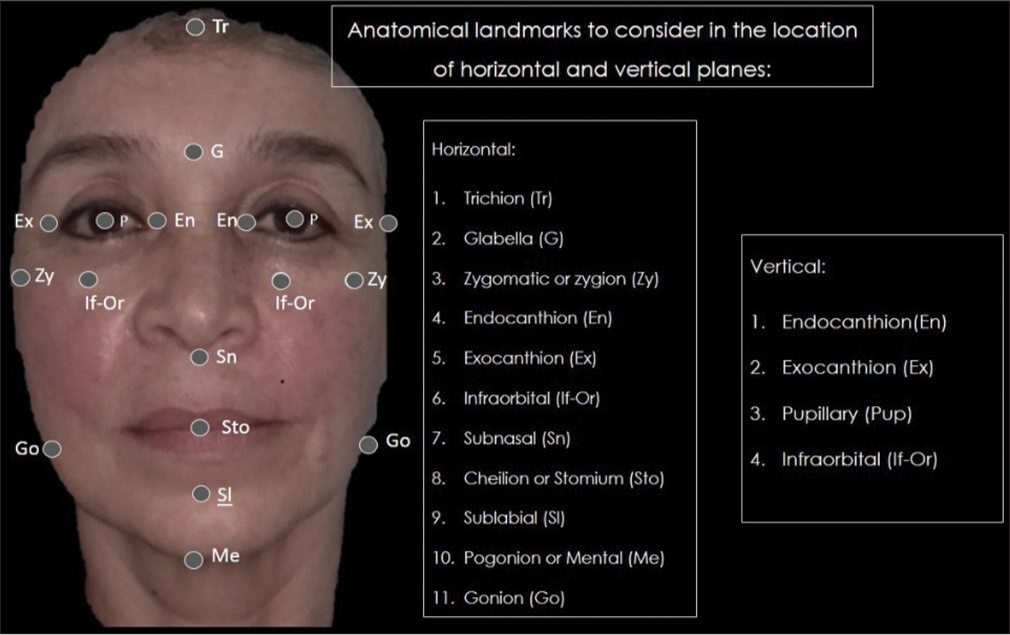
- Referential anatomical landmarks for drawing Cartesian planes.
These points, when connected, become vertical and horizontal planes. The line that joins the milestones from trichion to gnathion (vertical) divides the face into two halves (right and left), similar to the vertical line or Y-axis in a Cartesian plane, which we call the sagittal plane of the face or facial midline.
In the horizontal sense, from the union of the infraorbital anthropometric points (or infraorbital foramen) and the porion (highest point of the external auditory canal), the layout of a straight line is derived, called the “X axis”, which is the transverse or midfacial plane [Figure 2]. This X plane cuts perpendicular to the facial midline or Y-axis, coinciding with the well-known Frankfort cephalometric plane (projection of an imaginary line that starts from the tragus of the ears passing at the level of the cheekbones to join in the center). The crossing or point where the vertical line and the horizontal line intersect perpendicularly is known in Cartesian terms as the zero point or origin of the lines.

- Cartesian planes applied to the face.
Likewise, the tracing of vertical lines from the endocanthion and exocanthion (inner and outer edge of the eyes) generates four columns or spaces called vertical planes. The central plane (Pc) of the face, or “central facial column”, between the inner edges of the inner corners of the eyes. On each side in parallel, the column between the internal canthal and pupillary midline is the internal canthal plane (Pci).
The space from the pupillary point to the external canthal is known as the median canthal plane (Pcm) and the outermost from the external edge to the tragus area of the ear, the external canthal plane (Pce), which is the most stable area of the face despite aging, so it is an area of fixation and traction par excellence [Figure 3].
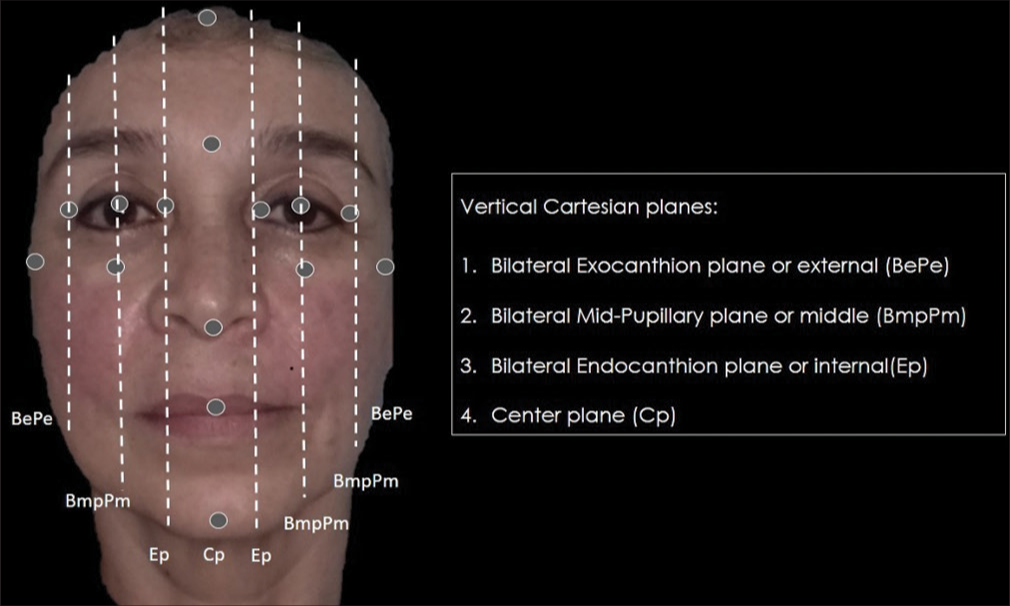
- Vertical Cartesian planes of the face.
In the same way, in the frontal position horizontally, other important planes are generated [Figure 4] that also intersect the vertical planes:
Frontal plane (Pf) or space between Trichion and glabella;
Superior ocular plane (Pos) between glabellar and interpupillary;
Inferior ocular plane (Poi) between the interpupillary and infraorbital lines;
Nasal oculus plane (Pon) between infraorbital and subnasal;
Nasolabial plane (Pnl) between subnasal and commissural;
Labio-mental (Plm) between commissural and mental.
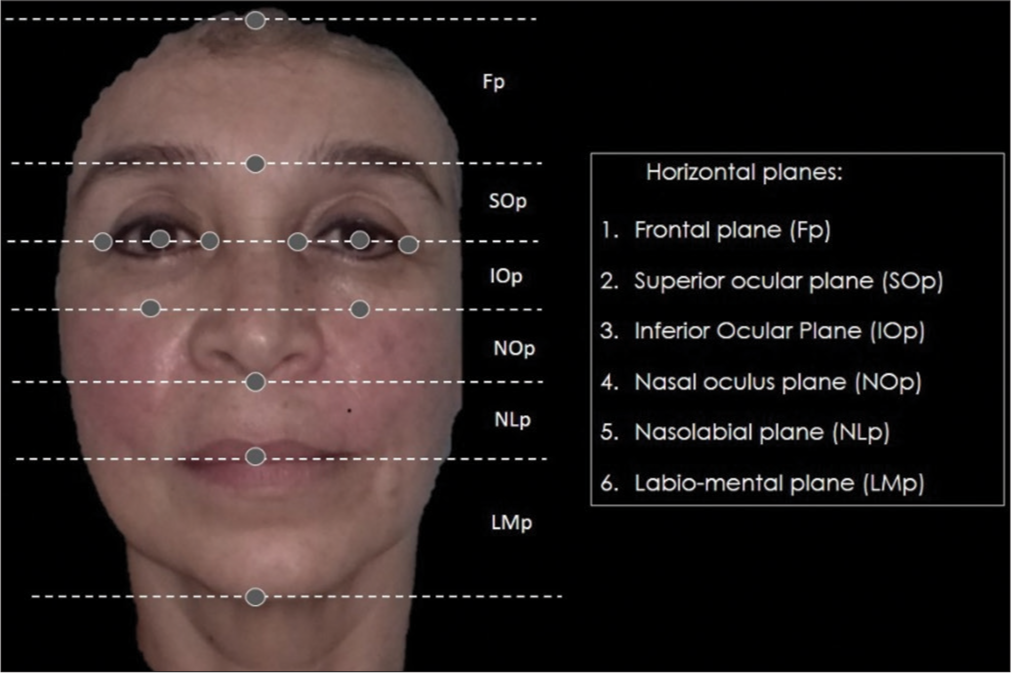
- Construction of horizontal planes in frontal position.
In this way, the intersection of these horizontal and vertical lines converts the face into a squared canvas which, in itself, is a spatial coordinate system, useful for orienting an effective dermo-support [Figure 5]. Within this coordinate system, more Cartesian planes form new zero points in each of the resulting sections, thus giving the possibility of creating a vector system of threads PDO scaffolding.
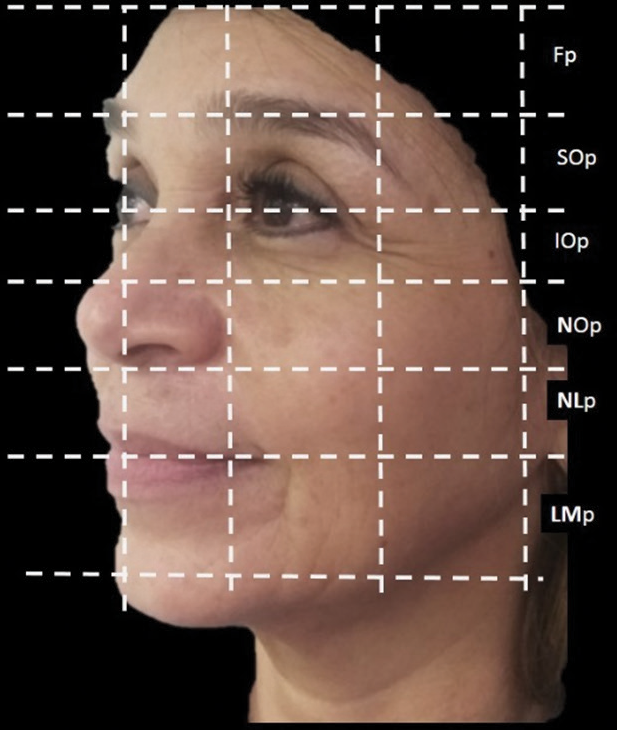
- Horizontal Cartesian planes of the face. Fp: Frontal plane, SOp: Superior ocular plane, IOp: Interior Ocular Plane, NOp: Nasal oculus plane, NLp: Nasolabial plane, LMp: Labio-mental plane.
According to the Cartesian Technique™, the PDO sutures should be positioned as vectors between each quadrant, in an upward oblique direction, which will allow the suture thread to provide a sustaining force with a coherent vector sense, direction, and magnitude, thus generating scaffolding forces with sufficient anchorage to produce greater facial tension, which optimizes the polydioxanone thread insertion technique. The arrangement of the PDO threads in diagonal vectors to the Cartesian system is illustrated below:
The white drop of material represents the zero point or origin of the Cartesian planes, which must be crossed by the PDO suture (orange thread) in an ascending oblique direction as vectors toward the external canthal plane and toward the internal canthal plane, forming a mesh that constitutes a vectorial scaffolding system for the polydioxanone threads [Figure 6a].
In turn, with the Cartesian Technique™, at least, three internal vectors could be designed for this sectorization in each grid, using active ingredients such as liquid PDO to reinforce the facelift [Figure 6b].
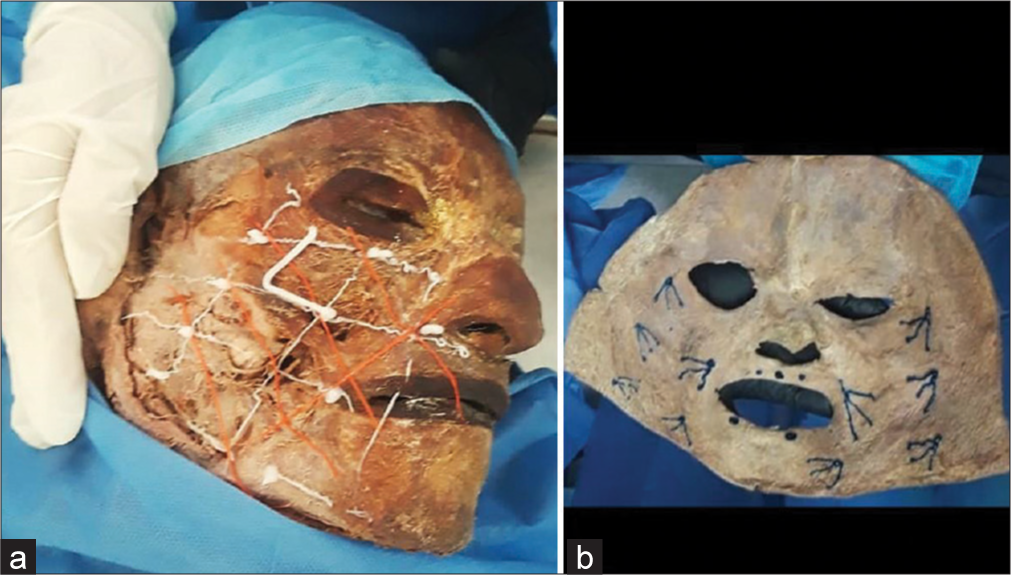
- (a) and (b) Cadaveric configuration for the Cartesian Technique™.
Clinical trial
A homogeneous sample of 35 patients was studied, obtained under randomization, without a control group, with the following diagnoses in common: primary and secondary rhytides, grade I lipomatosis, and grade I deflation. After completing the clinical history and informed consent, the patients were photographed and treated with the Cartesian Technique™ implanting polydioxanone sutures on both sides of the face.
The arrangement of the PDO sutures is carried out following the logic of vectorial support, in which the lines of greatest traction force are obtained by intersecting the Cartesian planes traced on the face (the Cartesian Technique™).
There are no exit points, only the entry orifice, since this same port is where the cannula emerges, leaving the monofilament on the skin plane after its exit. The thread applied into the superficial muscular aponeurotic system (SMAS), but the extreme of the thread, has not tied at the end.
The insertion of the threads will always be where the Cartesian planes intersect, forming the zero point, with vector magnitudes always directed cranially.
The yellow lines are the Cartesian planes; the green lines represent the scaffolded sutures.
The circle at the beginning of the arrows indicates the entry hole of the cannula with the thread.
The arrowhead indicates the direction of thread insertion [Figure 7].
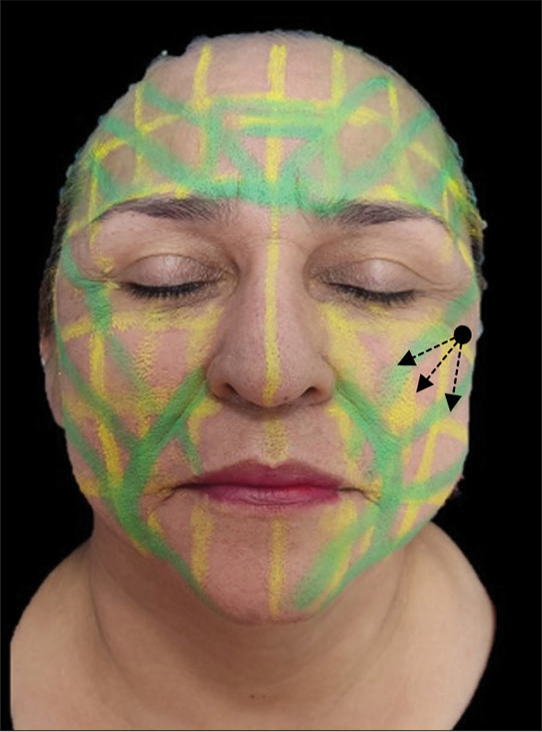
- Face paint illustrating the Smart Polydioxanone Suture (Smart PDOs™) vector scaffolding system. The black arrows indicate the direction in which the threads are inserted to obtain the maximum upward vector force., in an oblique direction towards the “zero” point, that is, towards the place of confluence of forces (crossing of horizontal, vertical and oblique lines) in the Cartesian coordinate plane
In each green line, a PDO number 27 G suture was inserted, motivated by the fact that it is a needle that allows an intradermal and subcutaneous application, even better redirecting the thread system and at the same time facilitating a better dosage of the cosmeceutical product used to enrich the thread (organic silicon).
To increase suture performance, the bioactive scaffolding technique was performed with Smart PDOs™. For this, organic silicon is incorporated into each thread at a dose of 0.1 mL, so with this technique, it is necessary to use 1 mL syringes with an interchangeable needle, which must be placed at the base of the needle or its pivot before withdrawing the thread to deliver the active ingredient through the cannula.
The evaluation of the tightening effect was carried out using clinical photographs immediately after the insertion of the sutures, 8 and 15 days later. In the photos, skin parameters of turgor, elimination of wrinkles (rhytids) and skin tightening were evaluated.
Clinical examination of the elastic resilience of the skin was then performed by the traditional method for the pinch test of skin turgor. A photographic record of the brightness or hydration of the skin was also carried out.
Based on previous methods, skin turgor assessment was finally classified on a visual turgor recovery scale whose values were: 0 = undetectable, 1 = low, 2 = moderate, and 3 = high.
On the other hand, to measure the position of flaccid or deflated tissues, the other scale used was the deflation scale (created by the authors8) which consists of:
“The level of deflation was measured with the vertical dimension scale [Figure 8]. The vertical dimension is the distance from the base of the nose to the chin. This distance must be compared with the distance from the tragus of the ear to the external canthus of the eye, which must be the same. This measurement is stable and therefore valid to verify if the lifting with threads or any other technique successfully achieves the replacement of the tissues.”8
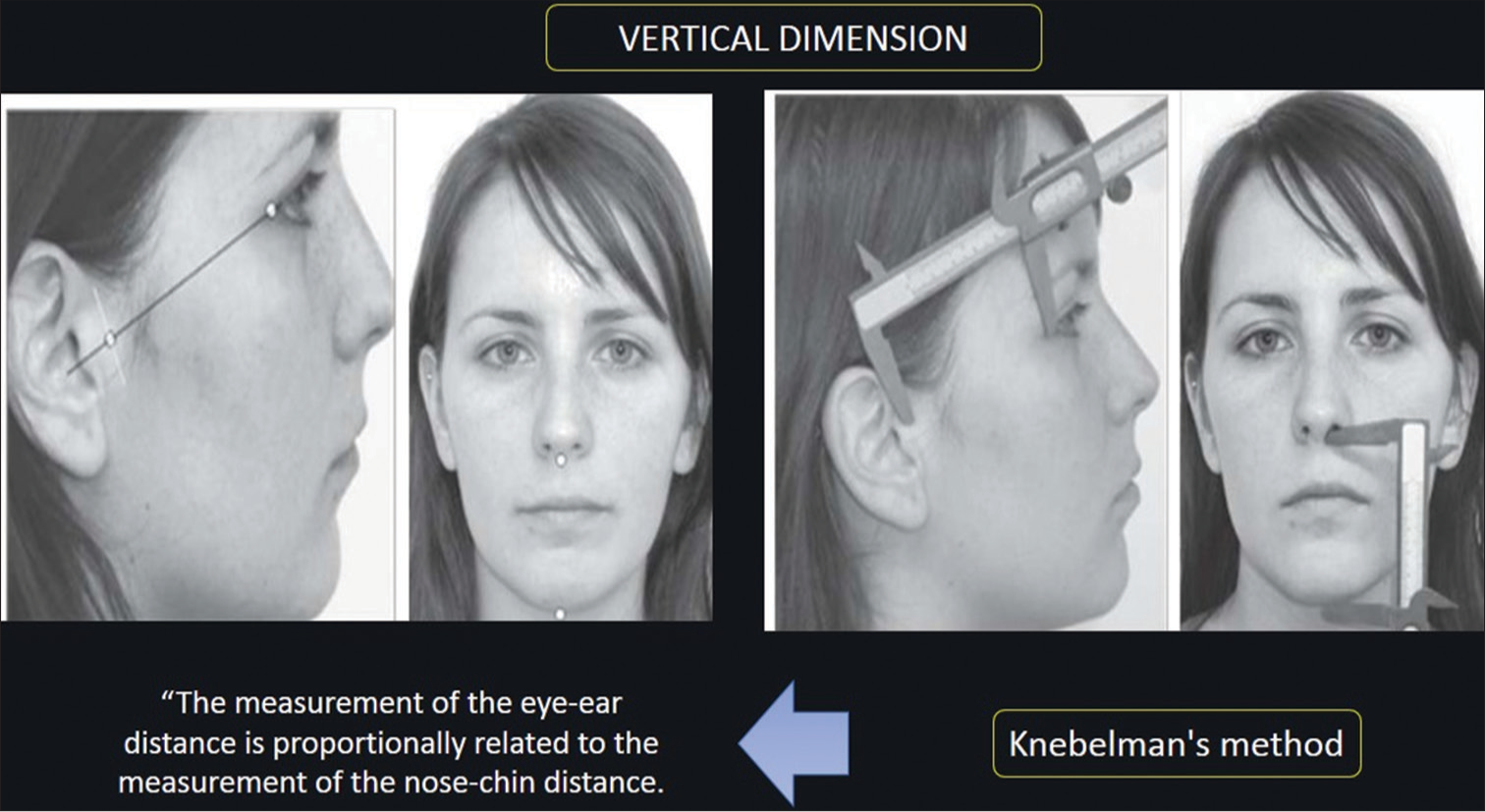
- Method for measurement of the esthetics vertical dimension.
Depending on the difference in millimeters that exists between these two distances (tragus-singing vs. nose-chin) a classification of the levels of descent, deflation, or sagging of the tissues was established [Figure 9]: Mild = difference between 2 and 5 mm, moderate: ≠ 7–10 mm, and severe: ≠ 10 mm.
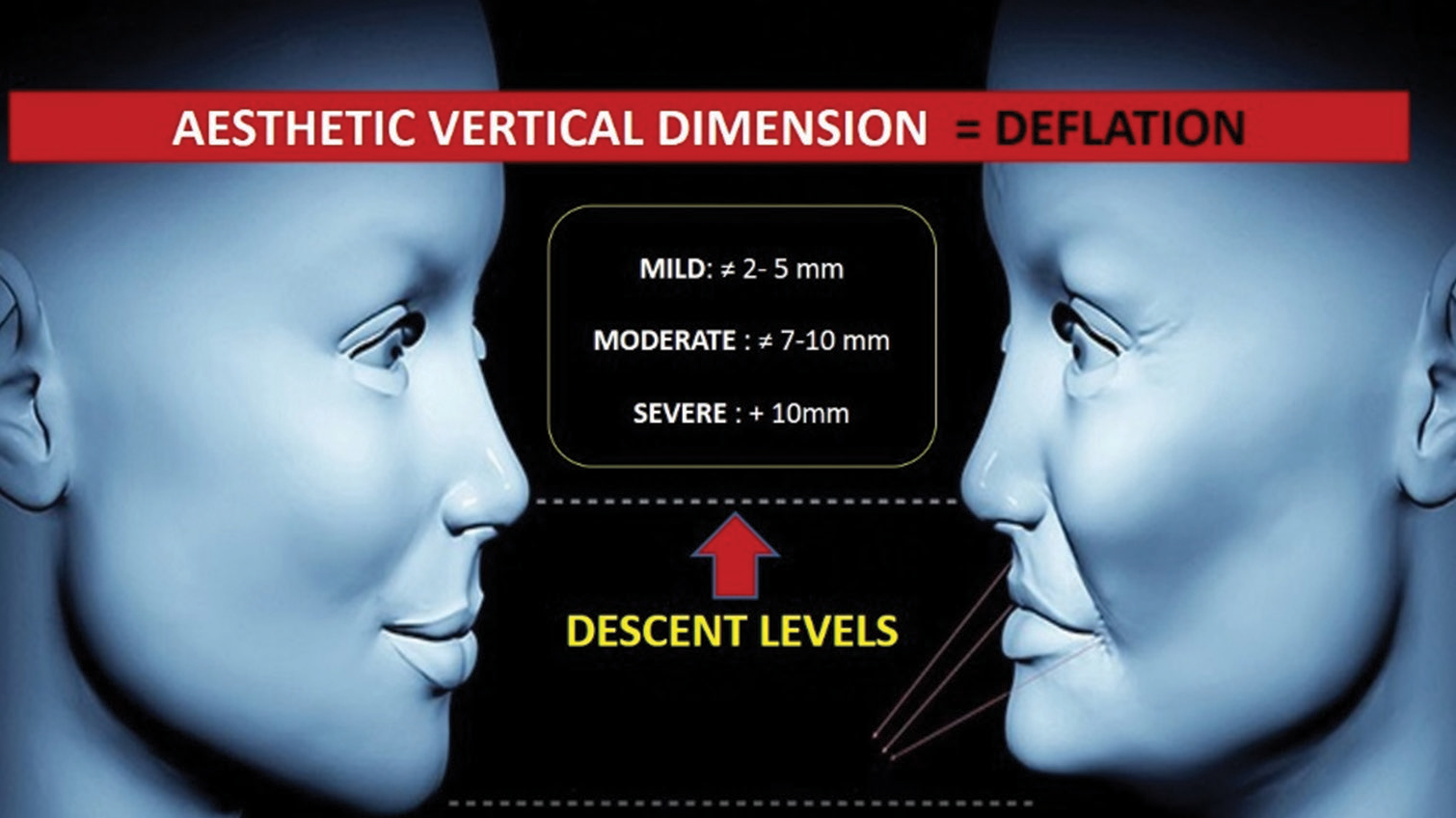
- Levels of loss of aesthetic vertical dimension (AVD) by descent of the aging tissues.
Based on this classification based on the loss of the esthetic vertical dimension, another scale was established to classify said deflation or severity of tissue sagging into three levels [Figure 10] that can be detected at the level of the facial contour by drawing a tangent line to the mandibular edge:
Grade 1 deflation: A discrete excess of the tissues below the mandibular line and corresponds to the level of slight descent (Decrease in Aesthetic Vertical Dimension (AVD) : ≠ 2–5 mm)
Degree 2 deflation: Deflation, moderate slump whose exceedance is proportional to the decrease in AVD moderate level (: ≠ 7–10 mm)
Grade 3 deflation: Severe sagging, mobile skin folding, with the collapse of the tissues of the mandibular area toward other tissues of the neck.

- Deflation scale by facial aging.
Said scales have been endorsed by the authors of this manuscript, which can be consulted in Velazco de Maldonado et al.8
The degree of recovery was clinically evaluated by three observers, specialists in dermatology, facial esthetics, and a plastic surgeon. The degree of satisfaction with the treatment was reported based on medical judgment, as shown in Table 1.
| Before | Immediate | 8 days | 15 days | |
|---|---|---|---|---|
| Turgor | Short 100% | High 100% | High 100% | High 90% |
| Rhytides | Accentuated 100% | Reversal of furrows and rhytides 100% | Reversal of furrows and rhytides 100% | Reversal of rhytides, smoothing of deep grooves 80% |
| Face tightening | Grade I deflation 100% | No deflation 100% | No deflation 100% | No deflation 90% |
Smart PDOs™: Smart polydioxanone suture
RESULTS
Capillarity test versus suture degradation with the technique Smart PDOs™
Optical microphotographs at 24, 48, and 72 h [Figure 11] show structural changes in the fibers of the PDO threads. The capillarity phenomenon is observed as a swelling in the yarn (retention of an aqueous content between the peripheral layers and the central core of the thread) accompanied by an increase in the interlaminar spaces (whitish stripes), indicative of the hygroscopic phenomenon experienced by the presence of organic silicon in the fiber.
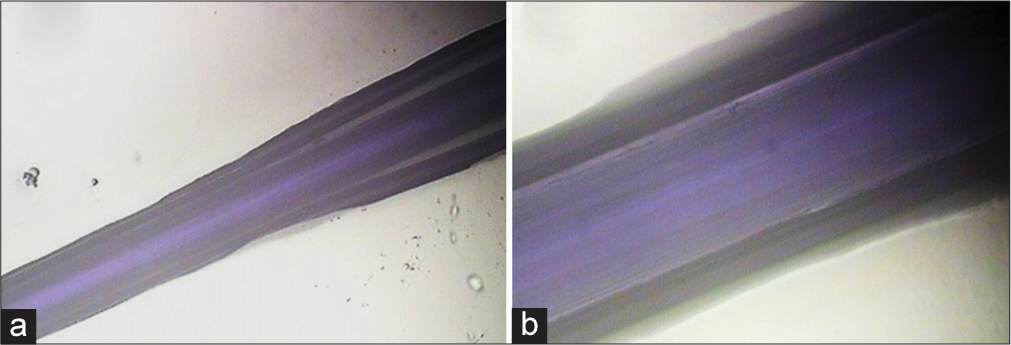
- Polydioxanone (PDO) thread after 24, 48, and 72 h of immersion in organic silicon. (a) ×4. The central area of the thread is surrounded by light-dark areas due to the retention of the drug. (b) ×10. An increase in interfibrillar and interlaminar spaces corresponds to the phenomenon of fluid absorption or capillarity of the PDO.
Sem
The smooth PDO threads are observed as cylinders with cuts on their periphery in the form of micro-spicules in opposite directions, which is possibly part of the factory design for their micro-anchoring [Figure 12a].
The silicon covers the thread and interpenetrates the fiber slit, demonstrating the indemnity of the PDO thread as it is enriched with CSi, which does not alter the structure of the thread, nor does it hydrolyze it, so it is presumed that the PDO thread with CSi is a scaffold physically stable [Figure 12b].
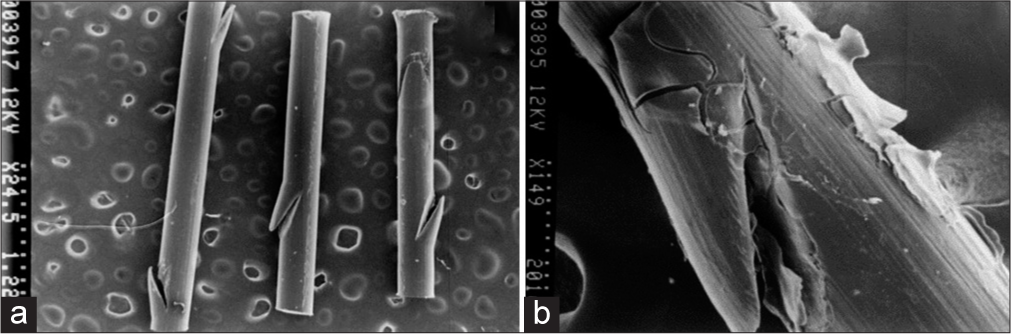
- (a) Topography of the polydioxanone (PDO) thread without the drug (control) scanning electron microscopy (SEM) microphotograph at ×25. Spicular slits are observed on the lateral edges. (b) PDO thread with Arg. SEM microphotograph at ×150. A layer covers the wire and interpenetrates the fiber cleft corresponding to the silicon on the PDO surface.
Controlled release of silicon from the PDO suture
Graph 1 evidences the UV-Vis spectrum of silicon release from PDO as a function of time. It can seem that at 24 h (pink) the highest absorbance peak is generated, this could correspond to an abrupt release of a large part of the drug into the medium, possibly due to partial and superficial degradation of the scaffold releasing the silicon into the medium. Graph 2 shows a slope in the form of a curve, one order higher than the zero-order, which indicates that it could be a first-order reaction; therefore, the release kinetics of silicon from PDO obey a controlled release system.
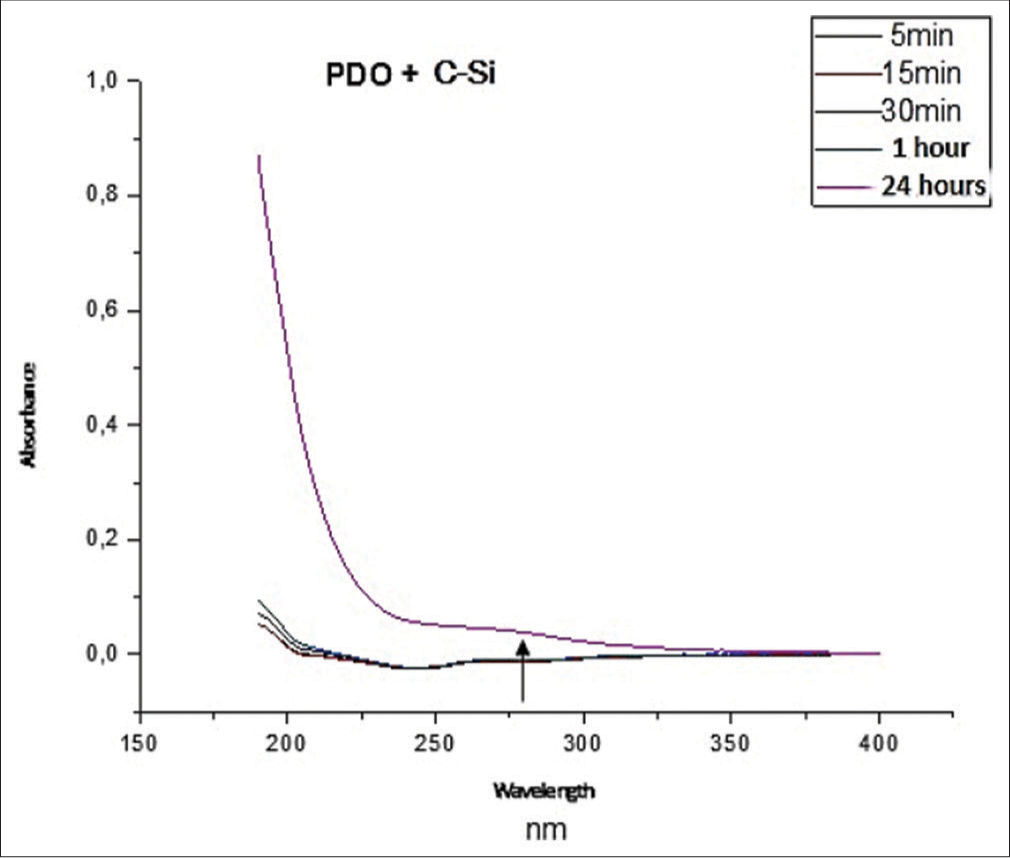
- Ultraviolet-visible spectrum of the polydioxanone (PDO) at the time intervals in which the release of organic silicon was measured. C-Si: Organic Silicon
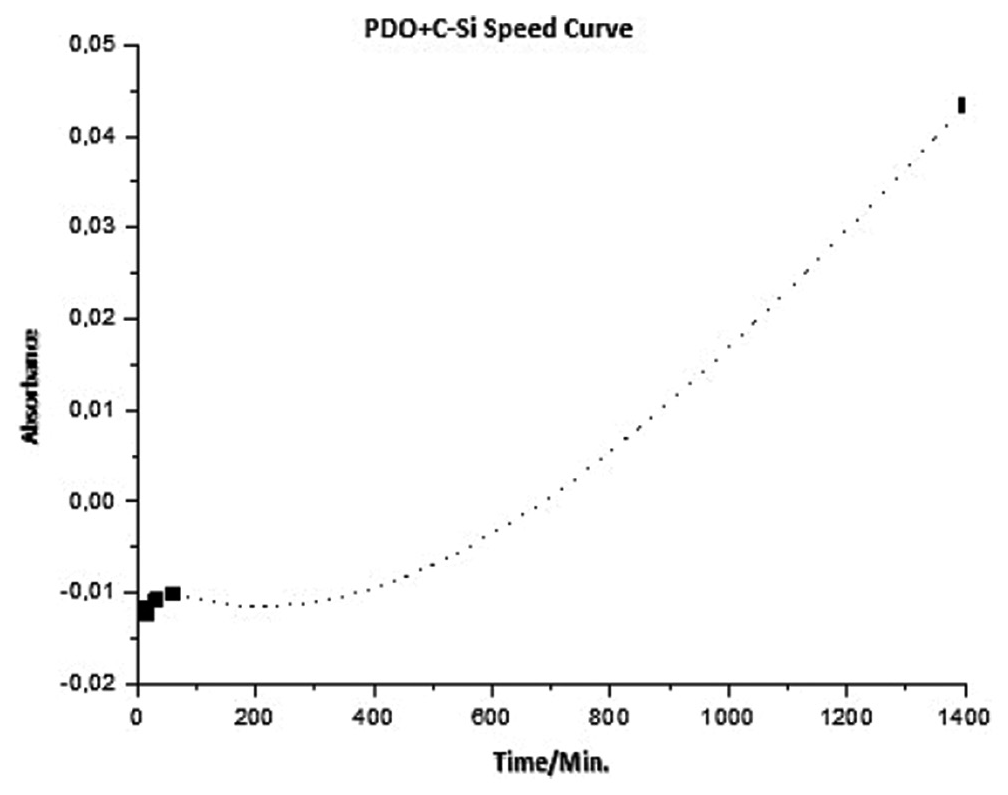
- Release curve of Organic Silicon (C-Si) from the Polydioxanone (PDO) thread plotting the absorbance as a function of time.
Histopathology study
The technique of enriching PDO threads with active ingredients such as organic silicon was previously studied through preclinical laboratory tests, subjecting PDO sutures to capillarity, biodegradation, and controlled release tests. In addition, the enriched sutures were tested on the skin of Wistar rats in the facilities of the Animal Experimentation Biotery of the Universidad de los Andes, before project approval by the bioethics committee of the same university with endorsement number CEBIOULA N123 of July 22, 2019.
For this reason, given the biocompatibility that has already been scientifically supported for the use of PDO sutures in humans and active ingredients such as organic silicon, the bioethics committee did not consider it necessary to carry out a histopathological study in humans. Although it was not the intention of the team of authors of this manuscript to include all the results of said histopathological study, for reasons of length of the text, we included some representative images of the tissue changes observed in the dermis and epidermis of rats with this technique.
Thirteen rats from the BIOU line: Wistar were divided into a control- control group (3) and an experimental group PDO-Silicon (5), a control group PDO alone (5), to which treatment was administered intradermally on the back. Euthanasia was performed at 4 weeks; skin samples were fixed in 12% formalin for further histological analysis [Figure 13].
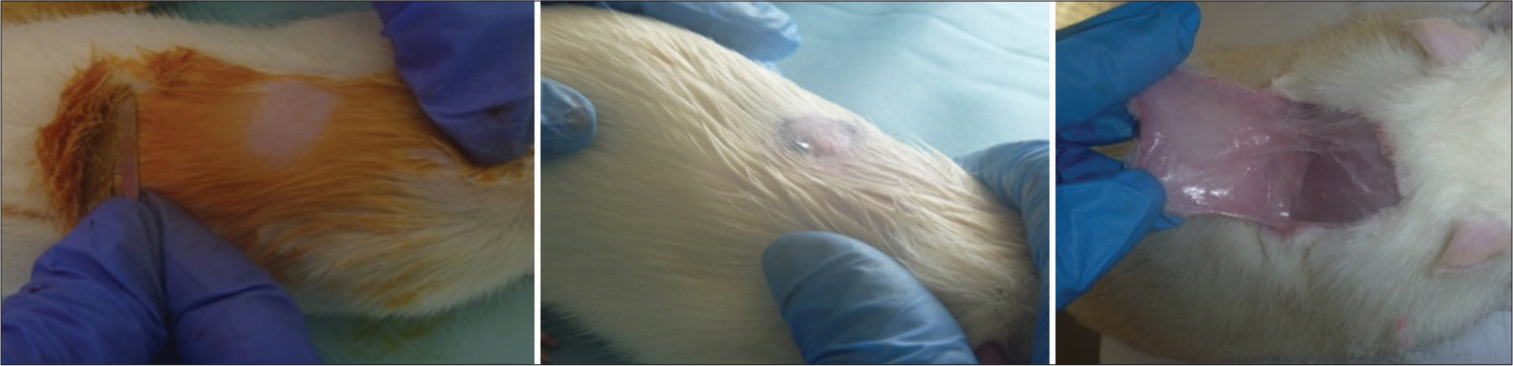
- Skin samples.
The observed results revealed characteristics similar to the young skin indicated in the control-control group [Figure 14]. The experimental group treated with the enriched suture technique showed the absence of inflammatory infiltrate and few blood vessels (100%) [Figure 15 and 16], few hair follicles (60%) [Similar to those observed in Figure 14], dense connective tissue (100%) with thick, intertwined collagenous fibers (100%) [Figure 17], no intercellular edema (100%), high fibroblast cellularity (100%) [Figure 18], thin epidermis with rectified basement membrane (60%) [Figure 19], and high dermal thickness (80%) [Figure 20]. It concluded that silicon synergistically potentiated the tissue effect of the PDO suture, generating greater biostimulation of fibroblasts with better quality collagen fibers, greater restructuring and redensification of the skin, and avoiding the late inflammatory response.
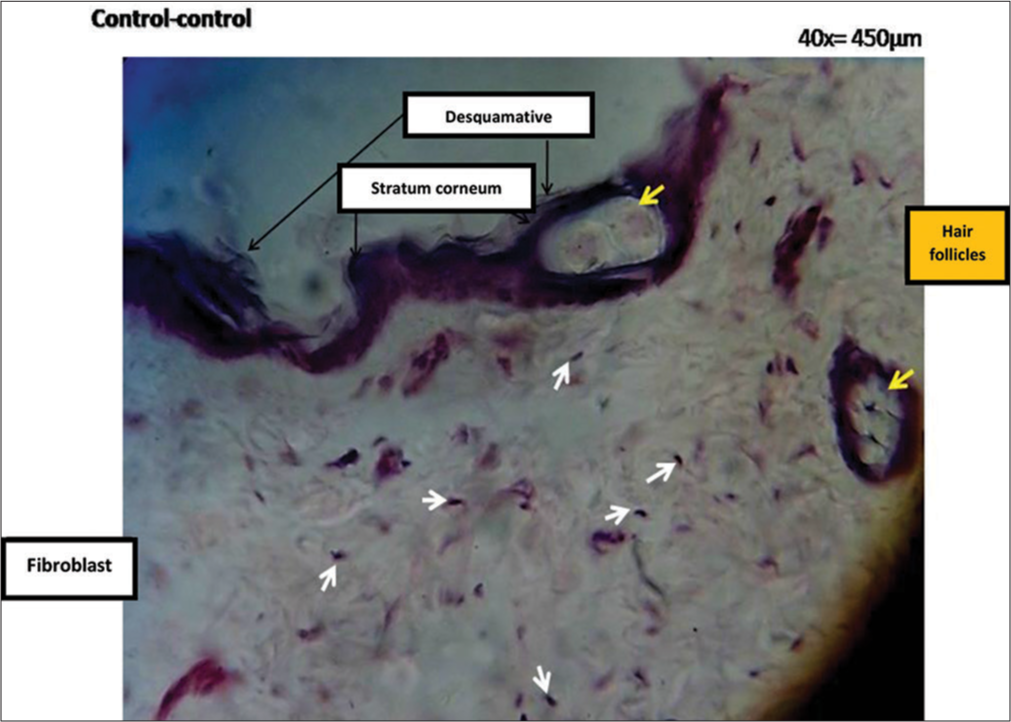
- Microphotograph of a histological section of the skin control-control group of the BIOU line: The stratum corneum is identified (the black arrows at the top of the histological preparation indicate the purple band corresponding to the stratum corneum) with its scaly cells (translucent strand located on the purple band or stratum corneum, layer indicated with black arrows), fibroblasts (white arrows indicating purple nuclei of fibroblasts in the dermis), pilosebaceous units in the dermis (yellow arrow on the right margin) and a follicle in the background behind the epidermis (yellow arrow in the purple stratum, above).
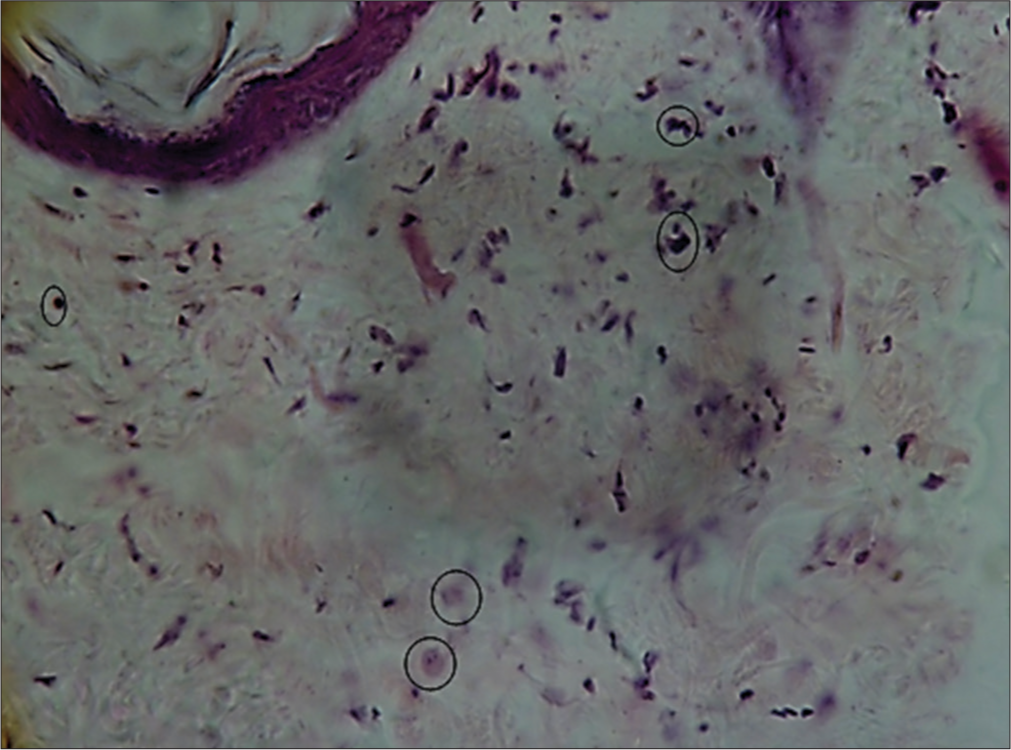
- Histological section micrograph of hematoxylin and eosin-stained skin (×40). A typical image of scant and perivascular inflammatory infiltrate (circle) was observed. Indicative that it is a mild, physiological inflammatory response, more typical of tissue biostimulation.
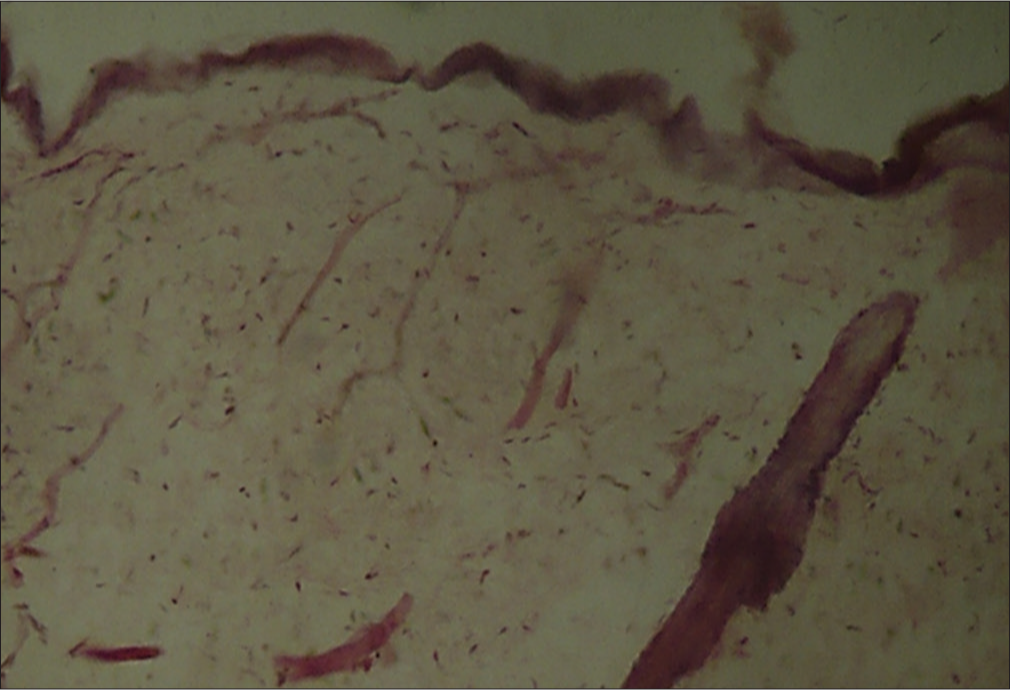
- Photomicrograph hematoxylin and eosin-stained histological section of skin (×40) representative of dense avascular connective tissue and absence of inflammatory infiltrate in the experimental group.

- Photomicrograph hematoxylin and eosin-stained histological section of skin (×40) representative of the dense connective tissue observed detailing the thickness and organization of the collagen fibers. The circle indicates the point from where the cannula should be accessed. From the same opening hole in the skin you can enter in several directions as indicated by the 3 oblique black arrows.
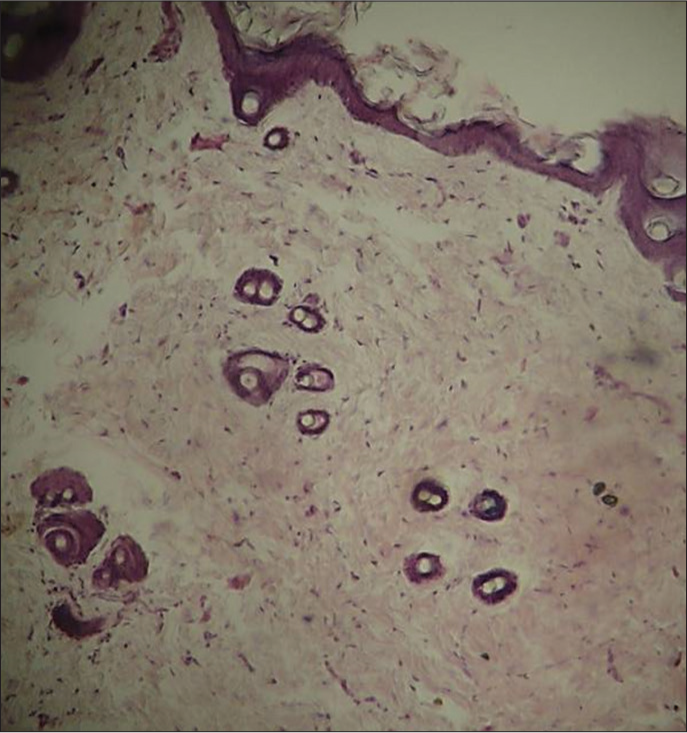
- Photomicrograph hematoxylin and eosin-stained histological section of skin (×40). Elevated fibroblast cellularity was observed in the experimental group.
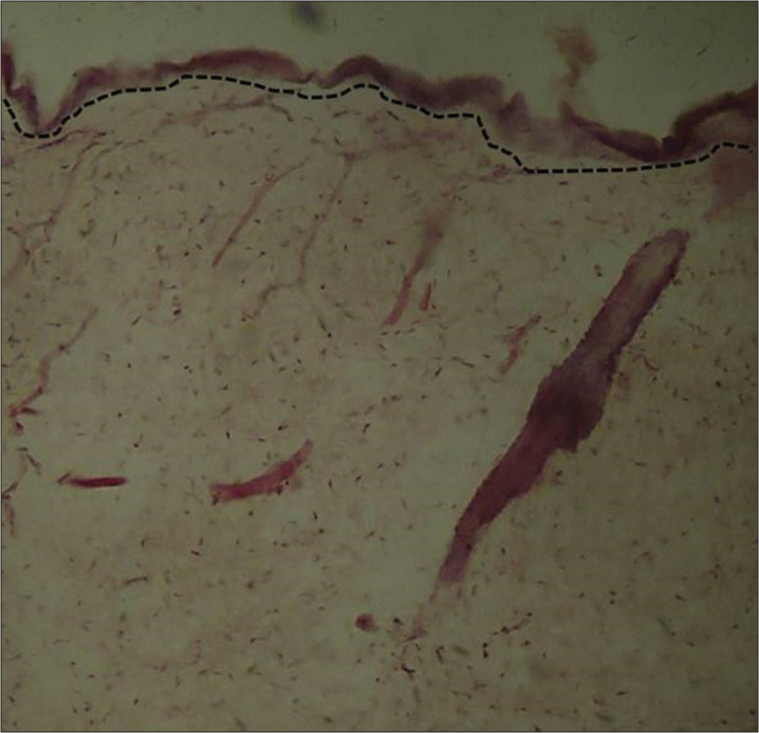
- Photomicrograph hematoxylin and eosin-stained histological section of skin (×10). The dotted black line borders the shape of the basement membrane that has been rectified by the thick epidermal thickness in the experimental group
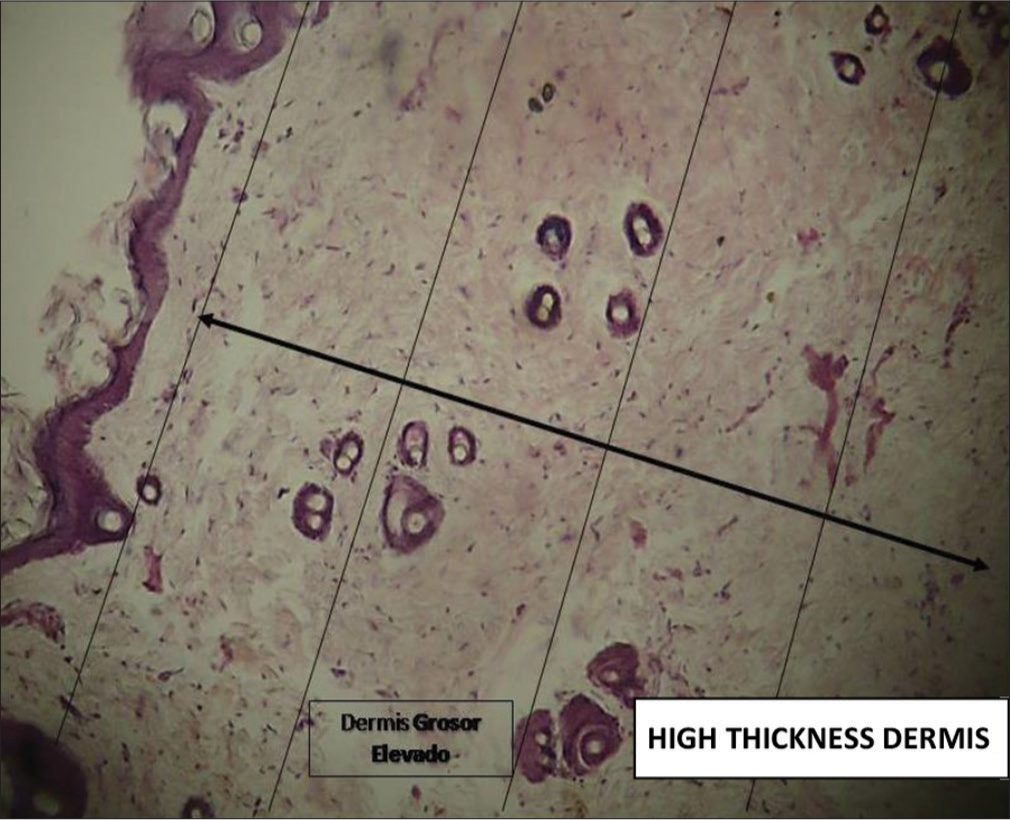
- Photomicrograph hematoxylin and eosin-stained histological section of skin (×40). The oblique black arrow crossing the histological preparation shows the size or thickness of the dermis in the experimental group (it occupies 4/4 of the field).
Results of the clinical trial
None of the patients reported any secondary and/or adverse effects and no adverse events were observed in the follow-up reviews.
A panel of three expert observers performed the clinical and photographic assessment. The expert operator who performed the treatments did not participate, to avoid interpretation bias. Facial tightening is an indirect measure obtained by contrasting the distances between the facial thirds before and after the lift, considering that a good lifting effect is achieved when the tissues are repositioned to the point that the proportion is similar between the three-thirds of the face [Figures 21-27].

- Case 1. Facial firming was obtained with the Cartesian Technique™ and smart polydioxanone suture (Smart PDOs™).
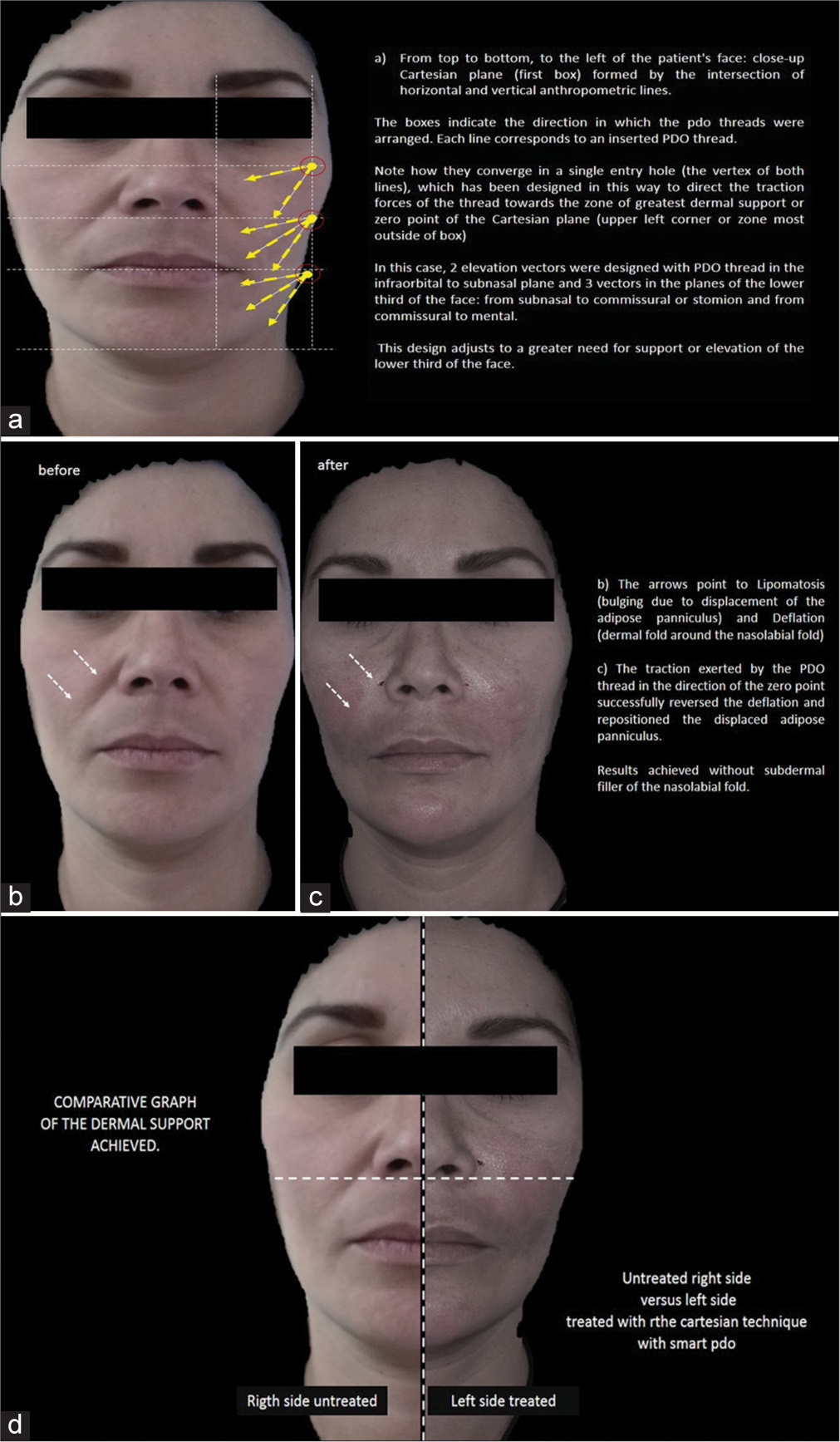
- Case 2 - (a) Diagram of design of the Cartesian Technique™ and smart polydioxanone suture (Smart PDOs™) over the patient. The yellow arrows indicate the direction of the Polydioxanone (PDO) thread (vector). As indicated by the 2 yellow arrows, 2 PDO sutures were inserted between the infraorbital and subnasal plane. Between the infraorbital and subnasal plane, 3 vectors or threads were inserted (yellow arrows) and 3 vectors (in the direction of the yellow arrows) or 3 threads were inserted between the planes of the lower third of the face: from subnasal to commissural or stomion and from commissural to mental. (b) Before and (c) after. (d) Results of the Cartesian Technique™ and Smart PDOs™.
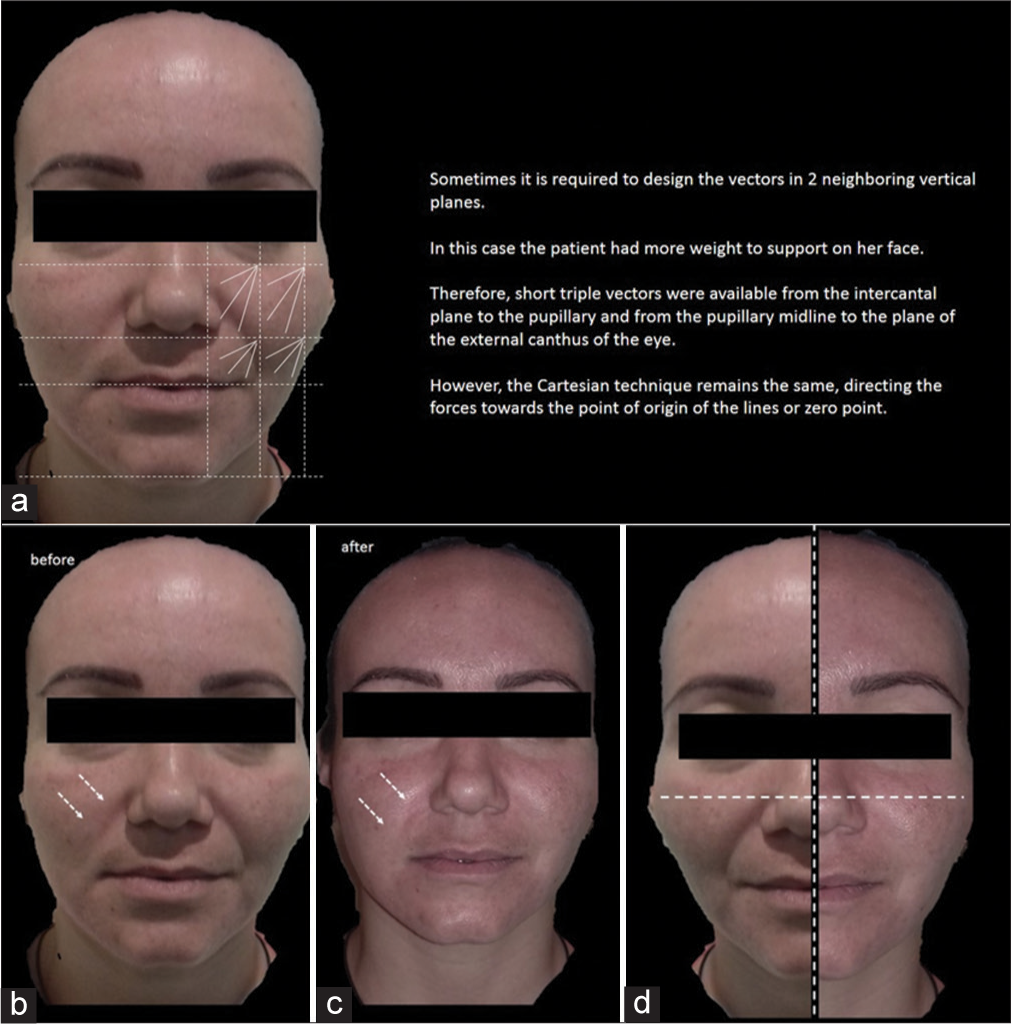
- Case 3 – (a) Diagram of design of the Cartesian Technique™ and smart polydioxanone suture (Smart PDOs™) over the patient. (b) Before and (c) after. The white arrows in (a), (b), and (c) indicate how by elevating the most superior and external tissues of the face with this system, the nasolabial fold, nasojugal fold, mentolabial folds, and primary and secondary wrinkles are reversed. The Jowls is also softened, demarcating the mandibular contour. (d) Results of the Cartesian Technique™ and Smart PDOs™. The horizontal and vertical dotted line represents the transverse plane of the face or X axis and the Y axis of the face. The dotted dividing line shows the untreated sagging tissues on the left side of the face, whereas, the tissues on the right side of the face (treated with the Cartesian technique and Smart PDOs) are observed to be much higher.
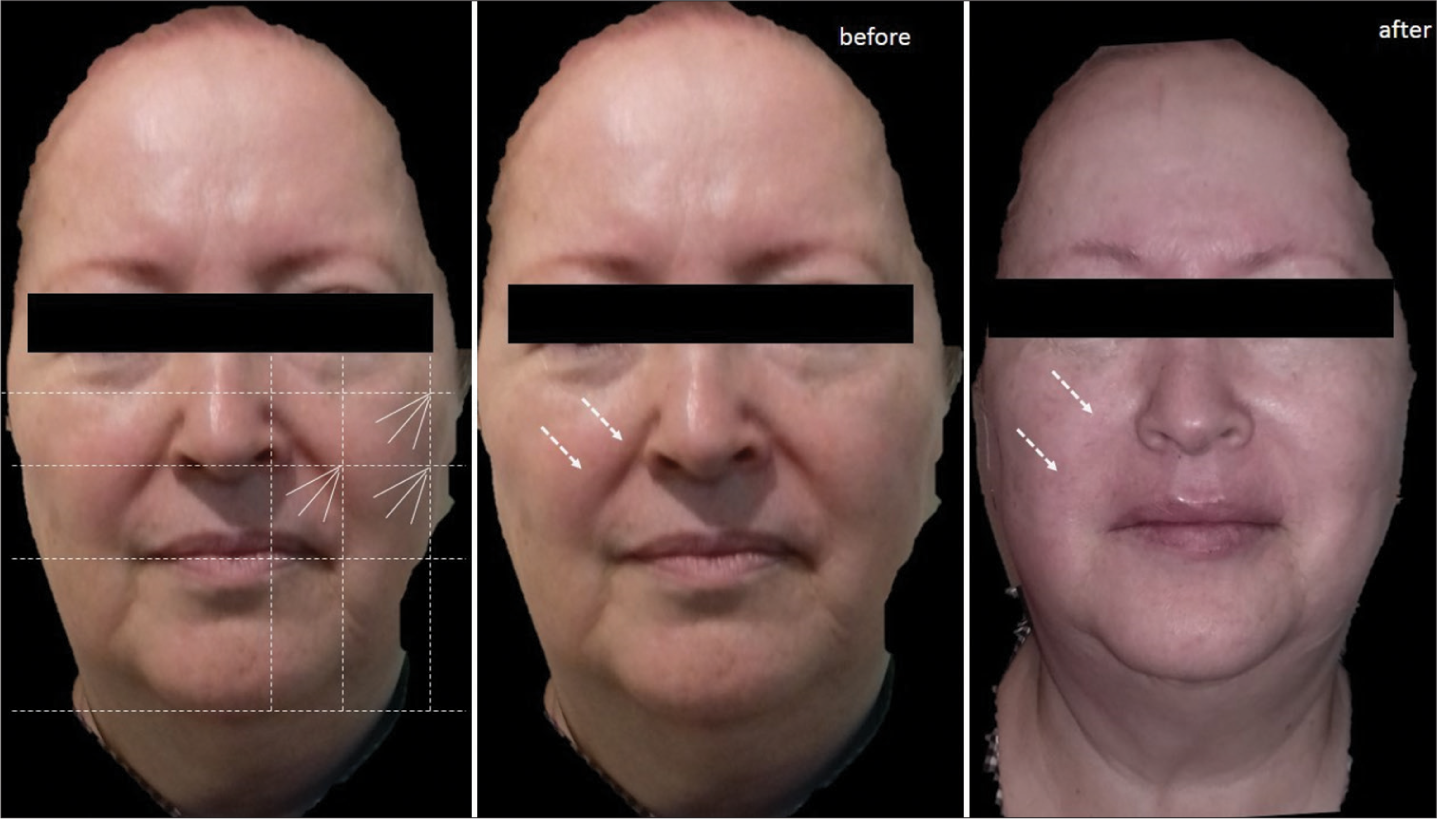
- Case 4: Diagram of design of the Cartesian Technique™ and smart polydioxanone suture (Smart PDOs™) over the patient and its results. The white arrows indicate how by elevating the most superior and external tissues of the face with this system, the nasolabial fold, nasojugal fold, mentolabial folds, and primary and secondary wrinkles are reversed. The Jowls are also softened, demarcating the mandibular contour.
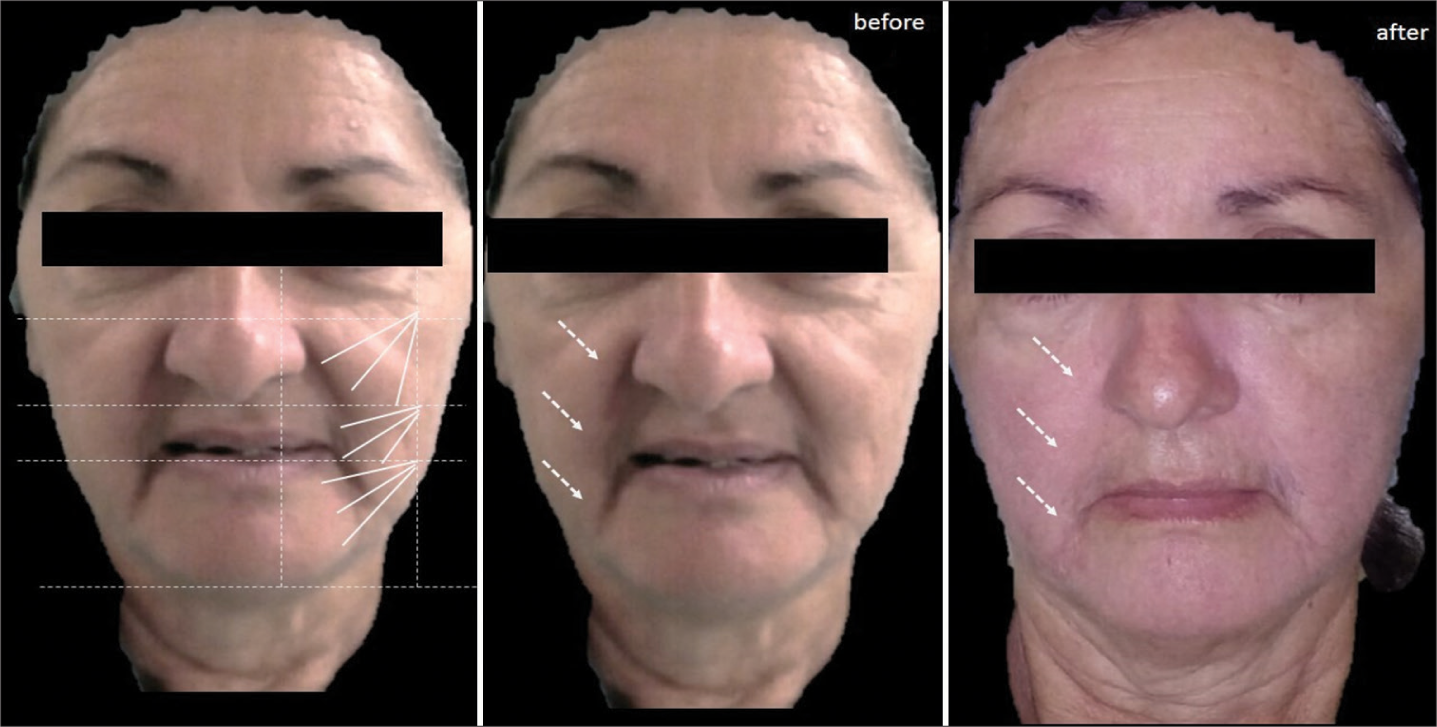
- Case 5: Diagram of design of the Cartesian Technique™ and smart polydioxanone suture (Smart PDOs™) and its results. The white arrows indicate how by elevating the most superior and external tissues of the face with this system, grooves such as the nasolabial groove are reversed.
- Case 6: Diagram of design of the Cartesian Technique™ and smart polydioxanone suture (Smart PDOs™) and its results. The white arrows indicate how by elevating the most superior and external tissues of the face with this system, furrows such as the nasolabial groove are reversed.
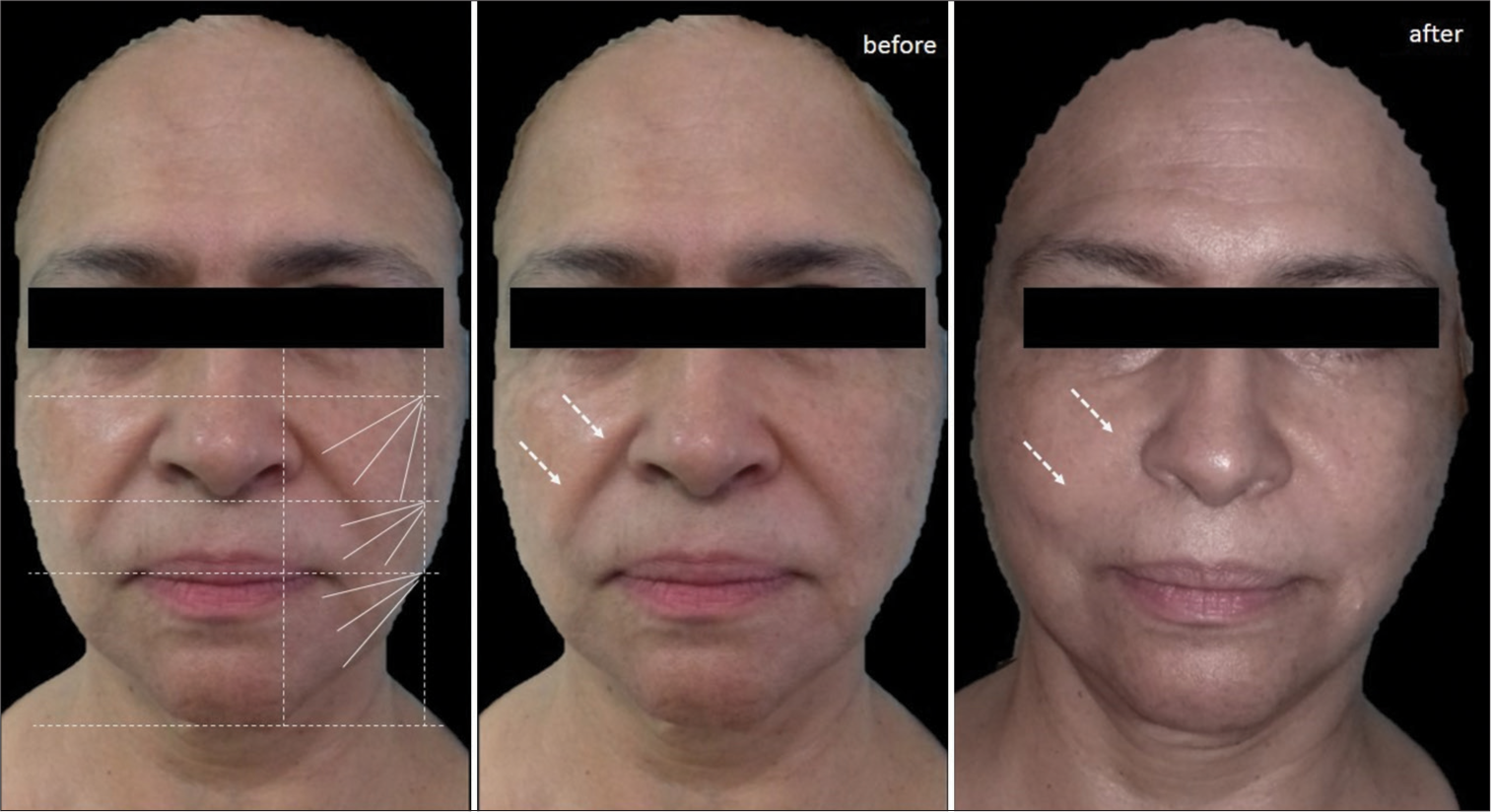
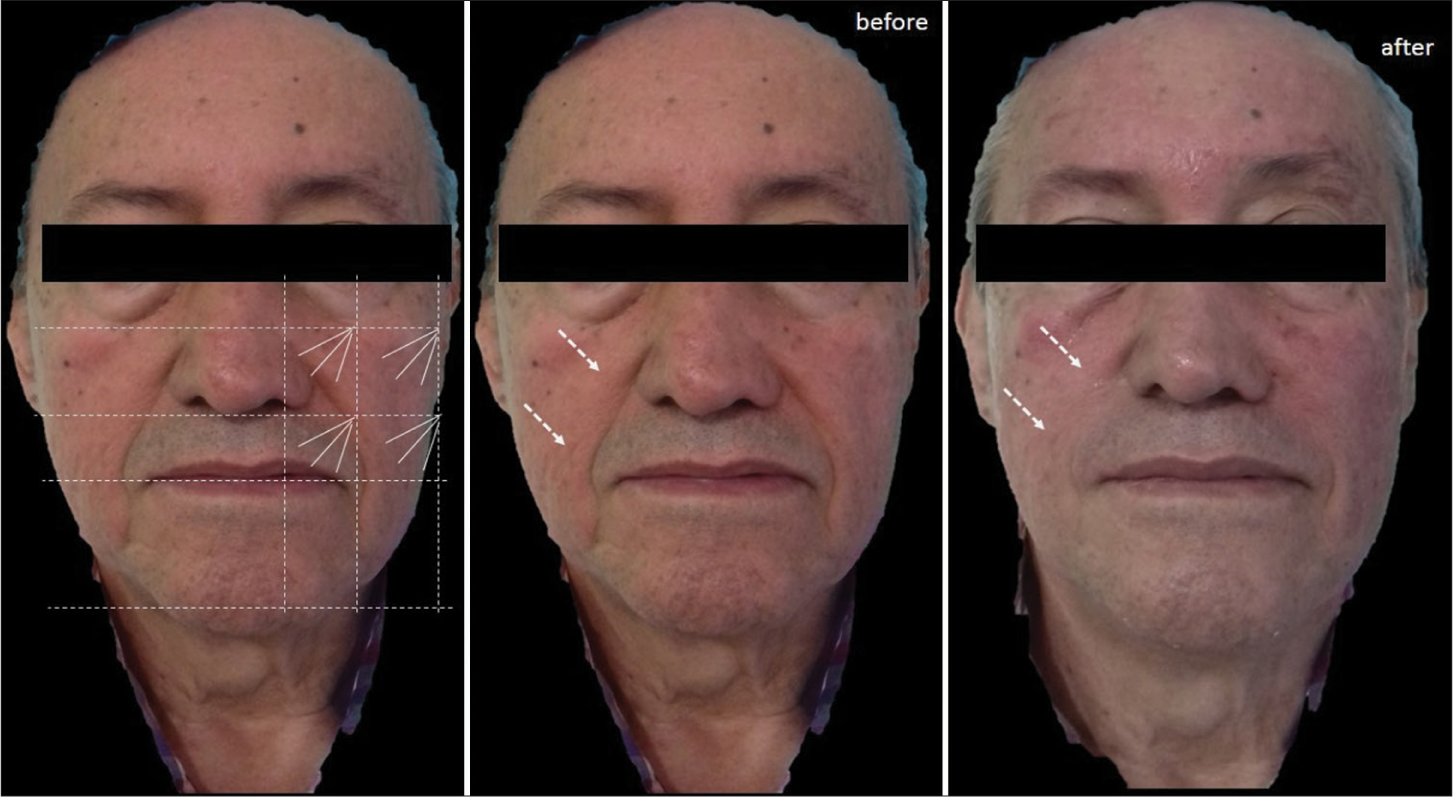
- Case 7: Diagram of design of the Cartesian Technique™ and smart polydioxanone suture (Smart PDOs™) and its results. The white arrows indicate how by elevating the most superior and external tissues of the face with this system, furrows such as the nasolabial groove are reversed.
The Cartesian scaffold managed to reverse deep grooves, even in problematic areas such as the malar festoon and nasojugal groove.
It softened the Nasogenian Groove and mentolabial folds and the primary and secondary rhytides.
It opens the ocular expression and densifies the skin of the entire face, but the tension achieved in the frontal and superciliary area counteracted the upper blepharochalasis. Dermo sustentation also manages to demarcate the Mandibular contour, hiding the Jowls.
Side effects
None of the patients reported any secondary and/or adverse effects and no adverse events were observed in the follow-up reviews.
Follow-up period
Long-term follow-up was performed at 2 and 4 months after the placement of the threads [Figure 28]. No follow-up was carried out at 6 months, since, at 180 days, the PDO has already been completely reabsorbed according to the indications of the manufacturers and preclinical studies.

- Results of the follow-up period. The white arrows indicate how tissue elevation is maintained with this system up to 4 months later.
DISCUSSION
In facial harmonization, one of the most desired objectives is to hold flaccid tissues in their original position and shape. Said facial tightening can be achieved if the dermal tissue is stimulated until its internal reorganization is achieved.9 In this sense, the strategy of using enriched PDO threads, as bioactive regenerative scaffolds, following the Smart PDOs™ technique, could be very successful, as has been detected in our research.
Scientific evidence indicates that PDO sutures manufactured with drugs or loaded with active substances have been used for other purposes such as preventing wound infections and promoting regeneration;10 our research is the 1st time that their use with biostimulatory substances for skin rejuvenation has been proposed.
In known drug-eluting sutures, the drug is added to the suture during the manufacturing process or by coating after a suture has been manufactured, by emulsion, dispersion, electrospinning, extrusion, and coating.11 However, so far all these procedures involve expensive and sophisticated manufacturing techniques.
Furthermore, no previous study has used drug-enriched absorbable PDO sutures in the subcutaneous tissue for rejuvenation purposes as we have proposed in the present investigation. In this sense, our method is innovative, since the use of smart PDO sutures is a technique.
This pioneering study shows that the PDO suture absorbs the drug by capillarity and is capable of slowly releasing it. In addition to the simplicity of the Smart PDOs™ preparation method, its effect on skin firming or facial lifting is successful, improving the clinical performance of sutures, as could be seen in the follow-up of patients in the phase I clinical trial.
There are few studies similar to ours that have performed an instrumental analysis of sutures for controlled release purposes. The most similar used polylactic acid and polycaprolactone sutures coated with ciprofloxacin and analyzed by electron microscopy and UV-vis spectroscopy, validating that these are the usual and reliable techniques to analyze this type of modified sutures for drug release.12
On the other hand, the success of facial tightening with Smart PDOs™ not only depends on its ability to release drugs but also on its correct anchoring in key points of the face. This is what the Cartesian Technique™ proposes, a clinical protocol that organizes the distribution of the traction forces of the PDO threads on the face for a successful and lasting reverse deflation.
The Cartesian Technique™ proposes to draw Cartesian planes on the face, to guide the direction and sense of each suture, which should be inserted from a diagonal and ascending zero point, generating traction forces or vectors with a natural sense of subjection. Together, this generates a subdermal mesh that provides greater biomechanical support, prolonging the lifting effect. This response was verified with the histopathological findings, which reveal that silicon synergistically potentiated the tissue effect of the PDO suture, generating greater biostimulation of fibroblasts with better quality of collagen fibers, greater restructuring and redensification of the skin, and avoiding the late inflammatory response.
Until now, a technique similar to the Cartesian Technique™ with Smart PDOs™ based on the use of drug-eluting sutures following a vector logic from facial anthropometric points has not been found. This technique is successful because it applies principles of physics, geometry, and engineering to subcutaneous facial support to distribute traction forces.
CONCLUSION
Preliminary clinical results indicate that the Cartesian Technique™ with Smart PDOs™ is an effective protocol for skin replenishment that enhances cell biostimulation through the release of bioactive drugs. It represents a very useful technique in facial harmonization, whose results indicate that it improves skin turgor, reverses rhytides, and counteracts deflation or flaccidity.
In addition, it is also a simple technique to apply, which allows the recipient tissue to be enriched with other bioactive substances such as the growth factors contained in injectable platelet-rich fibrin (i-PRF). It recommends expanding the sample and generating comparisons with PDO sutures without drugs, to establish statistical measures of association.
Authors’ contributions
Gladys J Velazco De Maldonado: Concepts, design, definition of intellectual content, literature search, clinical studies, experimental studies, data analysis, manuscript preparation, manuscript editing, manuscript review. Dubraska V Suárez-Vega: Design, definition of intellectual content, literature search, clinical studies, experimental studies, data acquisition, data analysis, statistical analysis, manuscript preparation, manuscript editing, manuscript review, guarantor. Blanca Miller-Kobisher: Literature search, clinical studies, experimental studies, manuscript preparation, manuscript editing, manuscript review. Victor García-Guevara: Literature search, clinical studies, experimental studies, manuscript preparation, manuscript editing, manuscript review.
Ethical approval
The research/study approved by the Institutional Review Board at CEBIOULA (Bioethics Committee of the University of the Andes, Mérida-Venezuela), number -CEBIOULA/123, dated -June 22, 2019.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Evaluation of biocompatibility of different membrane surfaces using unrestricted somatic stem cells. In Vivo. 2019;33:1447-54.
- [CrossRef] [Google Scholar]
- Polydioxanone-based bio-materials for tissue engineering and drug/gene delivery applications. Eur J Pharm Biopharm. 2015;97:371-91.
- [CrossRef] [Google Scholar]
- Medical grade polylactide, copolyesters and polydioxanone: Rheological properties and melt stability. Polym Test. 2018;72:214-22.
- [CrossRef] [Google Scholar]
- Novel polydioxanone multifilament scaffold device for tissue regeneration. Dermatol Surg. 2016;42:63-7.
- [CrossRef] [Google Scholar]
- Multipolydioxanone scaffold improves upper lip and forehead wrinkles: A 12-month outcome. J Cosmet Dermatol. 2019;18:879-84.
- [CrossRef] [Google Scholar]
- Editorial: Biomimetic materials for tissue regenerations. Front Cell Dev Biol. 2022;10:825455.
- [CrossRef] [Google Scholar]
- Innovative paradigm in aesthetics medicine: Proposal for diagnostic morphological geometric by thirds, semiology in clinical applied to aging facial. J Cutan Aesthet Surg. 2020;13:112-23.
- [CrossRef] [Google Scholar]
- Poly(ester-ether)s: II. Properties of electrospun nanofibres from polydioxanone and poly (methyl dioxanone) blends and human fibroblast cellular proliferation. Biomater Sci. 2014;2:339-51.
- [CrossRef] [Google Scholar]
- Electrospun medical sutures for wound healing: A review. Polymers. 2022;14:1637.
- [CrossRef] [Google Scholar]
- Engineering and polymeric composition of drug-eluting suture: A review. J Biomed Mater Res A. 2021;109:2065-81.
- [CrossRef] [Google Scholar]
- Controllable drug release behavior of polylactic acid (PLA) surgical suture coating with ciprofloxacin (CPFX)-polycaprolactone (PCL)/polyglycolide (PGA) Polymers. 2020;12:288.
- [CrossRef] [Google Scholar]







