Translate this page into:
Home cryolipolysis – A burning issue
*Corresponding author: Tiffanie-Marie Borg, Department of Plastic and Reconstructive Surgery, Northern Regional Burn Centre, Royal Victoria Infirmary, Newcastle, United Kingdom. tiffanie.borg@nhs.net
-
Received: ,
Accepted: ,
How to cite this article: Borg T, Campbell K, Zhao JC, Varma S, Lewis C. Home cryolipolysis – A burning issue. J Cutan Aesthet Surg. doi: 10.25259/jcas_57_24
Abstract
Cryolipolysis is a non-surgical technique for fat reduction whereby adipose tissue is exposed to low temperatures to induce apoptosis. This leads to a slow reabsorption of the excess tissue. The aim of this report is to increase awareness of the burns-related risks associated with home cryolipolysis treatments, with the goal of improving regulations around such treatments and preventing similar injuries from occurring in the future. This case report highlights the potential complications associated with cryolipolysis. We present the case of a 25-year-old female with a background history of bulimia nervosa who sustained mixed-depth burns to the abdomen and upper arms following a cryolipolysis treatment. She self-delivered using an online-bought machine. Although cryolipolysis is considered a safe method for the reduction of local adiposity, it is not without risk. Burns secondary to cryolipolysis treatments have occurred, though typically by unregulated providers, not self-use as in this case. There is a need for improved regulation of the administration of cryolipolysis treatments. Health-care professionals and patients should be aware of the possible complications that can arise. Improved regulation of cryolipolysis machine purchase and use is vital to prevent machine misuse by unregulated providers and members of the public.
Keywords
Cryolipolysis
Fat freezing
Burns
Cool sculpting
INTRODUCTION
Cryolipolysis involves the use of cold to stimulate lipolysis. Typically, skin is not damaged because the threshold for skin injury exceeds that for lipolysis.1 Cryolipolysis devices have been approved for flank and abdominal fat reduction by the Food and Drug Administration in patients with a body mass index <30 since 2010.2 Under the trademark “CoolSculpting,” millions of procedures have been performed worldwide.3 With increasing popularity, devices of variable quality have entered the marketplace. Risk is greater if practitioners purchase machines from non-reputable sources who have not offered training.
Complications of cryolipolysis include minor transient outcomes such as erythema, swelling, bruising, and pain and more severe complications such as paradoxical fat hypertrophy, contour irregularity, and nerve palsy.4 Thermal injury is an under-recognized and poorly appreciated complication of cryolipolysis.4
We report the presentation and management of a case of thermal injury secondary to cryolipolysis. The patient was managed in our burn center and followed up for 8 weeks.
CASE REPORT
This 25-year-old female presented with mixed-depth burns to the abdomen and upper arms following self-administered cryolipolysis using an online-bought machine. She did not follow the manufacturer’s recommendations. No barrier membrane was used, and the patient used the machine in colder settings than recommended. Cryolipolysis was performed at –8° for 45 min to the abdomen and –5° to the upper arms despite recommended temperatures of −3 to −4°. Although immediately post-treatment, her skin appeared normal, over the subsequent hours, she developed swelling, erythema, and blistering. No first aid was performed. She attended the Emergency Department the following morning, where the burns were wrapped in cling film, and the patient was referred to our care.
The patient has a background of bulimia nervosa. She did not intend to self-harm, rather reporting high stress following a binge-eating episode, for which she was attempting a quick fix. Although overweight, she has no other history.
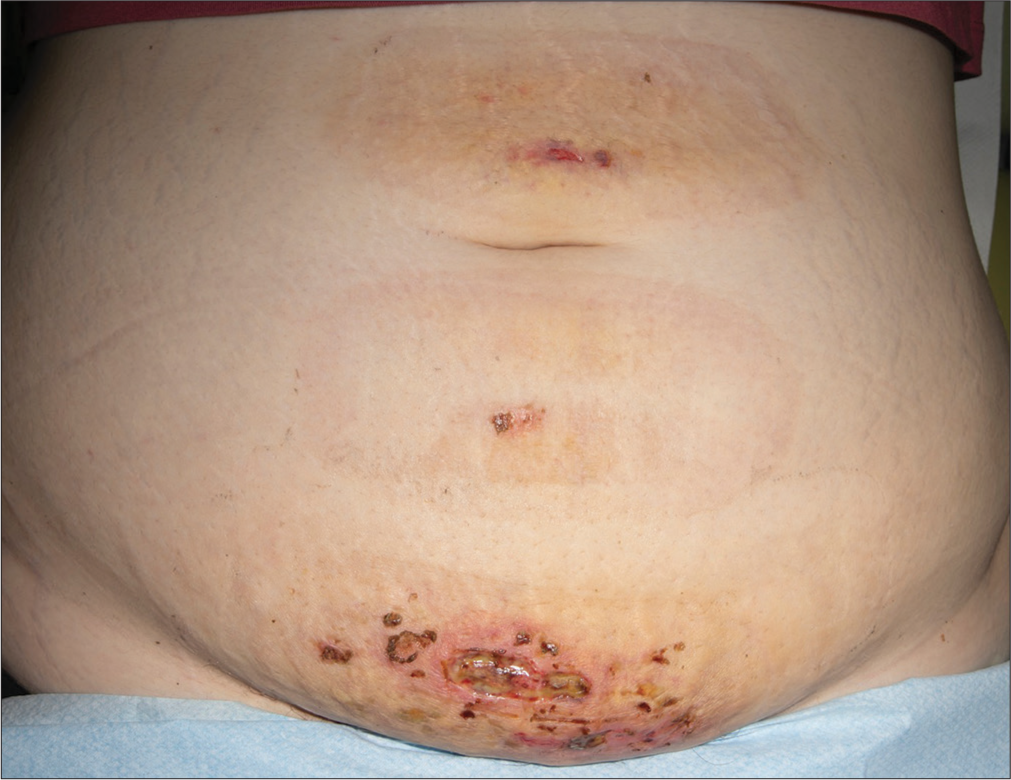
On examination, the patient had mixed depth burns to the lower abdomen and upper inner arms, amounting to 2% of total body surface area (TBSA) [Figure 1]. The shape appeared in keeping with the contact area of the machine. Most of the burns were superficial partial thickness, with the lower abdomen being mid-dermal.
The patient was managed conservatively. The epidermal burns of the arms were not dressed and fully healed within a week. Figure 2 demonstrates the abdominal burns at 1-week post-injury. Abdominal blisters were deroofed, then twice-weekly dressing changes were performed until fully healed at 8 weeks, when advice regarding scar massage for a hypertrophic scar at the lower abdomen was provided before discharge.
DISCUSSION
Cryolipolysis is a non-invasive technique designed to achieve localized fat reduction by targeted cold exposure to adipose tissue. Variation between machine providers includes size, ease of use, applicators, cooling capabilities, and the inclusion/ exclusion of built-in safety features such as automatic shutoff systems to minimize risk during treatments.5 In general, a similar approach is taken when providing treatments with all cryolipolysis machines. The machine is first set up according to the recommended temperature and treatment time for that machine and the target treatment area. A protective membrane is placed on the skin of the target area then the cooling plates are placed for treatment onset. This includes vacuum-type suction to the machine plates with localized temperature decrease. On completion of the treatment, the machine releases the area, facilitating the removal of the plates and membrane. Patient risk is minimized by (i) the use of high-quality cryolipolysis machines with built-in safety features, (ii) application of the protective membrane, (iii) treatment delivery using the machine according to its specifications and recommendations, and (iv) treatment delivery by an appropriately trained professional who, in the event of a complication, can promptly recognize and address this.
Literature generally supports the safety of cryolipolysis, with over 96% of patients reporting minimal pain1 or transient erythema, bruising, edema, and paraesthesia.4 However, complications have occurred in “do-it-yourself” attempts and when performed at beauty salons.6 Nseir et al., report the case of a 55-year-old female with 4% TBSA mixed-depth burns following an attempt of cryolipolysis at home.6 This patient applied dry ice wrapped in a paper bag and saran wrap to her abdomen, having sourced the do-it-yourself information from a YouTube video.
Choong et al.,7 reports the case of a 53-year-old female with two full-thickness 5 × 7 cm burns to the left lateral flanks following cryolipolysis at a beauty salon. Hours later, she developed painful blisters and erythema. However, the salon owner did not advise medical attention. This patient was not referred to plastic surgery until seen by her general practitioner due to increasing pain and exudate days later. Benoit and Modarressi,8 similarly report a female patient with full-thickness burns following cryolipolysis at a non-medical “clinic,” where, again, the beautician did not recommend medical input. The patient presented to the Emergency Department 2 days later with a 15 × 12 cm abdominal burn of full-thickness depth centrally with surrounding superficial-thickness burns.

- Burns to the abdomen with clearly delineated margins where the skin was in contact with cryolipolysis machine. Images taken 24 hours post-injury.
- Burns to abdomen demonstrating the healing process. Image taken 1-week post-injury.
A retrospective 8-year analysis of the New South Wales State-wide Burn Injury Service registry identified 10 patients with burns directly following cryolipolysis. The abdomen was most commonly affected, with a mean TBSA of 1% and depth of injury ranging from partial to full thickness.9
Our patient believed that her cryolipolysis device was medical grade and safe for use, having purchased it directly from a salon through eBay. It is unclear if this device is faulty. The risk was exacerbated by the patient’s deliberate failure to use a membrane between her skin and the machine, as well as use at lower temperatures for longer than recommended. Her rationale stemmed from a desire to increase fat loss achieved per treatment. The patient had not received any counseling or support for her bulimia nervosa before this. This presentation highlights several pitfalls regarding cryolipolysis: (i) Device reliability, (ii) user awareness of treatment administration and risks, and (iii) device misuse in patients with a history of eating disorders.
The Medicines and Healthcare Products Regulatory Agency expanded the scope of devices under regulation by Medical Devices Regulations to include cryolipolysis devices in November 2021.10 However, full implementation of these regulations is only expected by July 2025.10 Up-classification paves the way for improving patient safety through device testing and certification. However, regulations are needed regarding who can purchase and utilize such machines. Un-qualified practitioners performing cosmetic procedures remain a wider problem within the cosmetic sector in general.11 More stringent regulation of providers, device retailers, and devices are required to ensure patient safety. Robust systems for monitoring and reporting adverse events associated with these devices are required.
CONCLUSION
Thermal injury is an under-appreciated complication of cryolipolysis. Although “do-it-yourself ” YouTube has as many as 70,000 online views, it usually contains no information regarding the risks of thermal injuries. While some patients may seek treatment in a beauty salon or clinic setting, cryolipolysis-associated burns may not be entirely avoided due to defective devices and poor technician experience. Greater patient and practitioner understanding of cryolipolysis complications, with improved regulation of devices, is required. In the event of a thermal injury, first aid with prompt referral to burns should be considered.
Authors’ contributions
All authors have been involved in the care of the patient reported and in the production of this manuscript. The lead author is also responsible for manuscript inception, project design and write-up.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Selective cryolipolysis: A novel method of noninvasive fat removal. Lasers Surg Med. 2008;40:595-604.
- [CrossRef] [Google Scholar]
- Cryolipolysis for safe and effective inner thigh fat reduction. Lasers Surg Med. 2015;47:120-7.
- [CrossRef] [Google Scholar]
- The skinny on freezing fat. 2020. Available from: https://www.health.harvard.edu/blog/the-skinny-on-freezing-fat-2020031218990 [Last accessed on 2023 Jun 19]
- [Google Scholar]
- Adverse events associated with cryolipolysis: A systematic review of the literature. Dermatol Surg. 2020;46(supple 1):S8-13.
- [CrossRef] [Google Scholar]
- What is the best professional fat-freezing machine. Available from: https://www.vennhealthcare.com/whats-the-best-professional-fat-freezing-machine [Last accessed on 2024 Jun 25]
- [Google Scholar]
- Skin necrosis of the thigh after a cryolipolysis session: A case report. Aesthet Surg J. 2018;38:NP73-5.
- [CrossRef] [Google Scholar]
- Frostbite following cryolipolysis treatment in a beauty salon. J Wound Care. 2017;26:188-90.
- [CrossRef] [Google Scholar]
- Severe frostbite complication after cryolipolysis: A case report. JPRAS Open. 2020;24:499-515.
- [CrossRef] [Google Scholar]
- Cold burns as a result of cosmetic cryolipolysis: An emerging concern from the NSW statewide burn injury service. J Plast Reconstr Aesthet Surg. 2023;76:289-91.
- [CrossRef] [Google Scholar]
- Regulating medical devices in the UK. 2023. Available from: https://www.gov.uk/guidance/regulating-medical-devices-inthe-uk#overview [Last accessed on 2023 Jun 19]
- [Google Scholar]
- JCCP 10-point plan for safer regulation in the aesthetic sector. 2021. Available from: https://www.jccp.org.uk/NewsEvent/jccp-10-point-plan-for-safer-regulation-in-the-aesthetic-sector [Last accessed on 2024 May 02]
- [Google Scholar]







