Translate this page into:
Autonomic denervation dermatitis – A post-operative enigma
*Corresponding author: Ranjana Beniwal, Department of Dermatology, Venereology and Leprology, Dr. Sampurnanand Medical College, Jodhpur, Rajasthan, India. ranjanabeniwal@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Beniwal R, Agrawal A, Singh D. Autonomic denervation dermatitis – A post-operative enigma. J Cutan Aesthet Surg. doi: 10.25259/jcas_215_23
Dear Editor,
Autonomic denervation dermatitis (ADD) is an underrecognized, cutaneous complication presenting in the post-operative period. Herein, we describe a case series of 4 patients with this entity. Three males and one female, belonging to the age group 25–50 years, presented to the dermatology outpatient with lesions that developed 6–12 months after undergoing surgery around the knee. The lesions were well-defined erythematous-to-hyperpigmented scaly plaques adjacent to the surgical incision site [Figure 1 and Table 1]. Two of the patients reported associated numbness. Diagnosis of ADD was made, and they were prescribed mid-potency topical steroids and emollients. The lesions resolved within the next few weeks, and emollients were continued for maintenance.
| Patient no. | Age/Gender | Type of intervention | Latency period | Site of eczema | Sensory loss | Treatment |
|---|---|---|---|---|---|---|
| 1 | 27/M | Surgery for proximal tibia fracture fixation | 9 months | Lateral to incision | Absent | Topical steroids Emollients |
| 2 | 32/M | Surgery for proximal tibia fracture fixation | 12 months | Lateral to incision | Absent | Topical steroids Emollients |
| 3 | 37/M | Surgery for distal femur fracture fixation | 6 months | Lateral to incision | Present | Topical steroids Emollients |
| 4 | 42/F | Surgery for distal femur fracture fixation | 11 months | Lateral to incision | Present | Topical steroids Emollients |
F: Female, M: Male
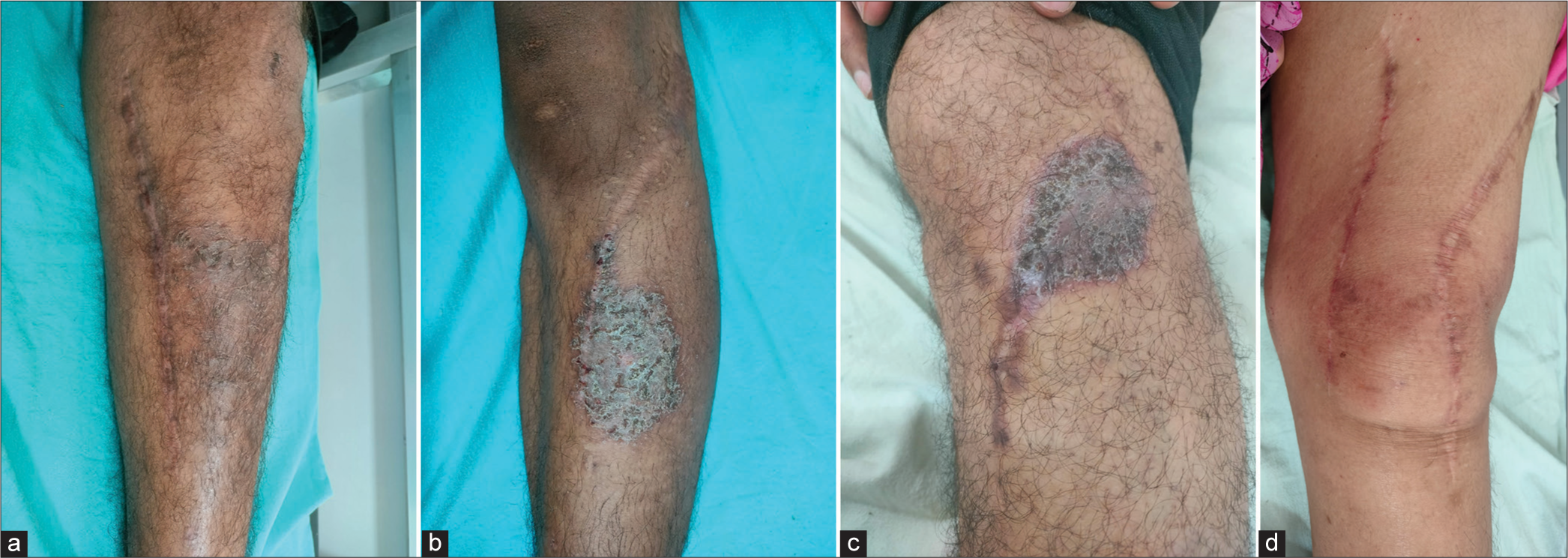
- Well-defined hyperpigmented eczematous plaques adjacent to the surgical incision site in (a) patient 1, (b) patient 2, (c) patient 3, and (d) patient 4.
The term ADD has been coined to include all eczematous eruptions at or around surgical sites, regardless of the nature and site of the operative procedure. It has been proposed to include a subset terminology known as “SKINTED,” surgery of the knee, injury to the infrapatellar branch of the saphenous nerve (IPSN), and traumatic eczematous dermatitis.1 Clinically, ADD can range from a simple rash to an extensive eruption or even an excoriated zone of papules or macules. It can be asymptomatic or associated with numbness and can run a chronic and persistent course exhibiting frequent remission and relapse. The associated numbness resolves over time with reinnervation of the area by the surrounding neural structures. On histopathology, it is suggestive of chronic spongiotic dermatitis.2
ADD occurs secondary to iatrogenic insult. It has been postulated that the injury to the IPSN, which supplies the anterolateral aspect of the knee below the patella, increases the transepidermal water loss, leading to xerosis and also alters the behavior of keratinocytes by hampering the secretion of neuropeptides including substance P and acetylcholine. This leads to disruption of the epithelial barrier and increases the risk of dermatitis over the affected area.2 Another mechanism that has been proposed for the occurrence of eczema in hypoesthetic skin is a defect in forming inter-corneocyte lipids due to faulty release of ceramide from the lamellar bodies leading to an improper water barrier formation.3 It has also been proposed that skin incisions can cause transections of dermal nerves, leading to denervation and impairment of sudomotor and vasomotor responses. “Trophoneurosis” is used to describe the alteration in cutaneous architecture and physiology after injury to peripheral nerves.1 Injury to IPSN is common, but only a few develop ADD, which is explained by a probable theory of the extent of nerve damage, wherein a larger incision with some crushing component due to retraction may lead to more chances of developing ADD.4 Figure 2 shows the distribution and sensory area supplied by the infrapatellar nerve. It is important to distinguish ADD from hypersensitivity to iodine or dressing patches and metal hypersensitivity. Hypersensitivity reaction to iodine or dressing patches is localized to the application area only, could be anywhere around the knee, and is not associated with sensation loss. Metal hypersensitivity is more generalized, presents all around the knee, and could be associated with swelling and fluid formation.5 ADD is more location specific, with most cases localized at the inferolateral aspect of the knee along with numbness in IPSN distribution.6 Table 2 summarizes the recent studies regarding ADD.
| S. No. | Author | Study design | Number of patient | Type of intervention | Latency period | Site of eczema | Time for resolution | Treatment |
|---|---|---|---|---|---|---|---|---|
| 1. | Pathania and Singh7 | Case report | 1 | TKA | 3 months | Lateral to incision in both knees | 2 weeks | NR |
| 2. | Mathur and Sharda8 | Case Report |
2 | TKA | 11–16 months | NR | NR | NR |
| 3. | Nazeer et al4 | Prospective cohort study | 148 | TKA | 3–6 months | Lateral to surgical site | 4–10 weeks | Topical steroids |
| 4. | Mukartihal et al.6 | Retrospective cohort study | 3318 | TKA | 2–6 months | Lateral to surgical site | 6–12 weeks | Topical steroids |
| 5. | KavyaDeepu and Sekar9 | Case report | 1 | TKA | 3 months | Lateral to surgical site | 2 weeks | Topical steroids |
| 6. | Mahajan et al.10 | Case report | 1 | TKA | 3 months | Lateral to surgical site | 8 weeks | Topical steroids |
| 7. | Das et al.11 | Case report | 1 | Amputation of great toe of right foot | 2 years | Dorsum of right foot | NR | Topical steroids |
| 8. | Baxi et al.12 | Case series | 3 | TKA | 3–5 months | Over, lateral and medial to surgical site | NR | Topical steroids |
| 9. | Ray et al.13 | Case report | 1 | Coronary artery bypass Graft surgery |
2 years | Medial aspect of the left lower limb | NR | Topical steroids |
| 10. | Vivekanandh, et al.14 | Case series | 6 | 1-Coronary artery bypass graft surgery 2,3,4-Split-thickness skin graft 5,6-Surgery for left Tibial fracture |
4 months–3 years | 1,2,3,4-ver graft site 5,6-Over trauma site |
NR | 3-topical steroids Rest-NR |
NR: Not reported, TKA: Total knee arthroplasty
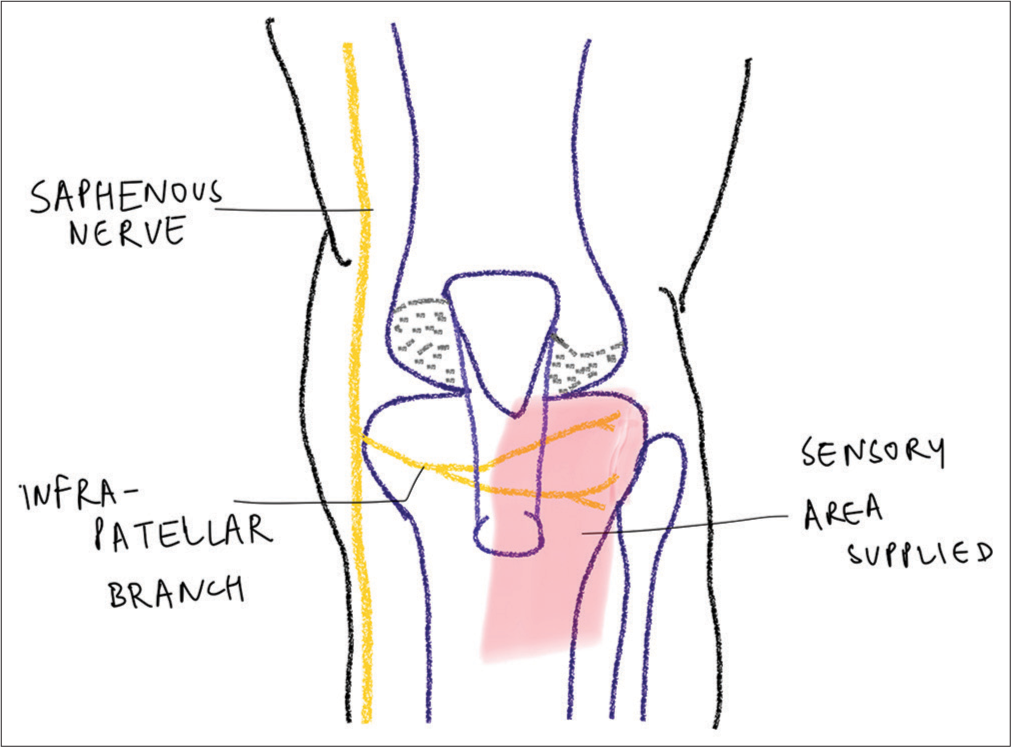
- Diagram showing the sensory area supplied by the infrapatellar nerve.
Treatment of ADD includes maintaining the skin barrier through the use of emollients and occlusive moisturizers and short-term use of topical steroids.1 Dermatologists and surgeons should be aware of this underreported entity to permit early diagnosis, management, and allay unnecessary anxiety in the post-operative period.
Authors’ contributions
Ranjana Beniwal: Conceptualization, Data Curation, Formal Analysis, Investigation, Methodology, Project Administration, Supervision, Visualization, Writing (Original Draft), Writing - Review and Editing. Akriti Agrawal: Conceptualization, Data Curation, Formal Analysis, Methodology, Project Administration, Visualization, Writing (Original Draft), Writing -Review and Editing. Devendra Singh: Conceptualization, Formal Analysis, Investigation, Methodology, Project Administration, Supervision, Visualization, Writing - Review and Editing.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Autonomic denervation dermatitis: A new type of eczematous dermatitis. Clin Dermatol Rev. 2017;1:61-4.
- [CrossRef] [Google Scholar]
- Explaining a hitherto nameless condition: 'SKINTED' Clin Exp Dermatol. 2009;34:e465-6.
- [CrossRef] [Google Scholar]
- Asteatotic eczema in hypoesthetic skin: A case series. JAMA Dermatol. 2014;150:1088-90.
- [CrossRef] [Google Scholar]
- SKINTED: A rare complication after total knee arthroplasty. Arthroplast Today. 2020;6:1028-32.
- [CrossRef] [Google Scholar]
- Dermatitis on the knee following knee replacement: A minority of cases show contact allergy to chromate, cobalt, or nickel, but a causal association is unproven. Contact Dermatitis. 2006;54:228-9.
- [CrossRef] [Google Scholar]
- Neuropathy dermatitis: An underdocumented complication following total knee arthroplasty. Indian J Orthop. 2023;57:445-52.
- [CrossRef] [Google Scholar]
- SKINTED: An autonomic denervation dermatitis. Int J Dermatol. 2020;59:613-4.
- [CrossRef] [Google Scholar]
- Autonomic denervation dermatitis in two patients. Indian J Clin Dermatol. 2019;2:96-7.
- [Google Scholar]
- Arriving at SKINTED (Surgery of the knee, injury to the infrapatellar branch of the saphenous nerve, traumatic eczematous dermatitis): A case report. Cureus. 2024;16:e54307.
- [Google Scholar]
- SKINTED: An uncommon cutaneous complication of total knee replacement. Am J Neurodegener Dis. 2023;12:16-22.
- [Google Scholar]
- Autonomic denervation dermatitis. Indian J Dermatol Venereol Leprol 2024 [Article in Press]
- [CrossRef] [Google Scholar]
- What is in a name?-demystifying “SKINTED”-a review of literature from dermatological perspective. Turk J Dermatol. 2023;17:1-5.
- [CrossRef] [Google Scholar]
- Autonomic denervation dermatitis: A case series of six patients. Med J Dr DY Patil Vidyapeeth. 2024;17:231-3.
- [CrossRef] [Google Scholar]






