Translate this page into:
Nasal dermoid sinus cyst with intracranial extension and atretic sinus tract in an adult patient
*Corresponding author: Ayse Gokce, Department of Radiology, Bursa Yuksek Ihtisas Training and Researching Hospital, Bursa, Turkey. draysegokce@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gokce A, Onbas O. Nasal dermoid sinus cyst with intracranial extension and atretic sinus tract in an adult patient. J Cutan Aesthet Surg. doi: 10.25259/jcas_60_21
Abstract
Nasal dermoid sinus cyst (NDSC) is a rare congenital lesion due to cephalic neural tube defect. It may also have been seen in other parts of the body. NDSC constitutes 1–3% of all dermoid cysts and 11–12% of those in the head and neck. A NDSC is located in the median line of the nasofrontal region from the glabella to the columella. The differential diagnosis based on location includes epidermal inclusion cyst, glioma, meningomyelocele, meningoencephalocele, teratoma, teratoid cyst, thyroglossal duct cyst, branchial cleft cyst, and benign lymphadenopathy. Intracranial extension causes serious complications such as meningitis, osteomyelitis, abscess formation, hydrocephalus, seizures, and personality changes. All patients with NDSC should be considered to have a potential intracranial extension and should, therefore, undergo pre-operative radiological evaluation. Herein, the authors report an unusual adult patient with NDSC with intracranial extension.
Keywords
Nasal dermoid
Nasal mass
Intracranial extension
INTRODUCTION
Nasal dermoid sinus cyst (NDSC) is a rare congenital anomaly caused by a cephalic neural tube defect that occurs in the early embryonic period.1 Dermoid was frequently written as “dermoid cyst” or “dermal cyst” in many reports, and most nasal dermoids were connected with fistula tracts. Therefore, he proposed the term “NDSCs” for all such lesions.2 While most lesions are detected in the 1st 3 years, some cases may not go unnoticed until adulthood. The oldest case described in the literature was 56 years old.3 A medical history and physical examination are required to evaluate these lesions. It may be asymptomatic or there may be signs of swelling in the nasal region pre-operative radiological evaluation. The study should include fine computed tomography (CT), and supplementary magnetic resonance imaging (MRI) should be considered if intracranial extension is a concern. In the case we presented, we wanted to mention that radiology plays a major role in the diagnosis of NDSC in asymptomatic patients and the evaluation of intracranial extension. In addition, we wanted to draw attention to the role of CT in determining the ossified intracranial component and sinus tract in our case, despite the MRI, which seems sufficient by some authors to evaluate the intracranial extension of NDSCs.
CASE REPORT
Brain MRI of a 46-year-old female patient revealed a millimeter nodular lesion with homogeneous fat density on the nasal dorsum and an extra-axial heterogeneous lesion measuring 2.5 × 2 × 2 cm in the left olfactory sulcus [Figures 1-2]. On fat-suppressed T2-weighted MR images, the lateral part of the lesion was observed as hyperintense, consistent with cystic features, while there was signal loss in the medial part [Figure 2]. Furthermore, rim-like enhancement was detected in the periphery of the lesion in the dense cyst intensity described in the lateral part. Complementary CT imaging revealed that most of the lesion in the left olfactory sulcus was an ossified lesion with a bony cortex. In addition, the atretic sinus tract extending through the frontal bone was observed more clearly [Figure 3]. A millimeter nodular lesion on the nasal dorsum line was observed with a homogeneous fat density [Figure 3]. The medical history of the patient was questioned, and it was learned that she had a nasal dermoid cyst operation when she was 1½ years old. It was learned that the patient’s sense of smell was not different. In addition, there was no visible finding around the nose. The patient only had a migraine-like headache. When the findings were evaluated together and due to the previous operation, it was evaluated in accordance with the NDSC with atretic sinus tract and extending intracranially.
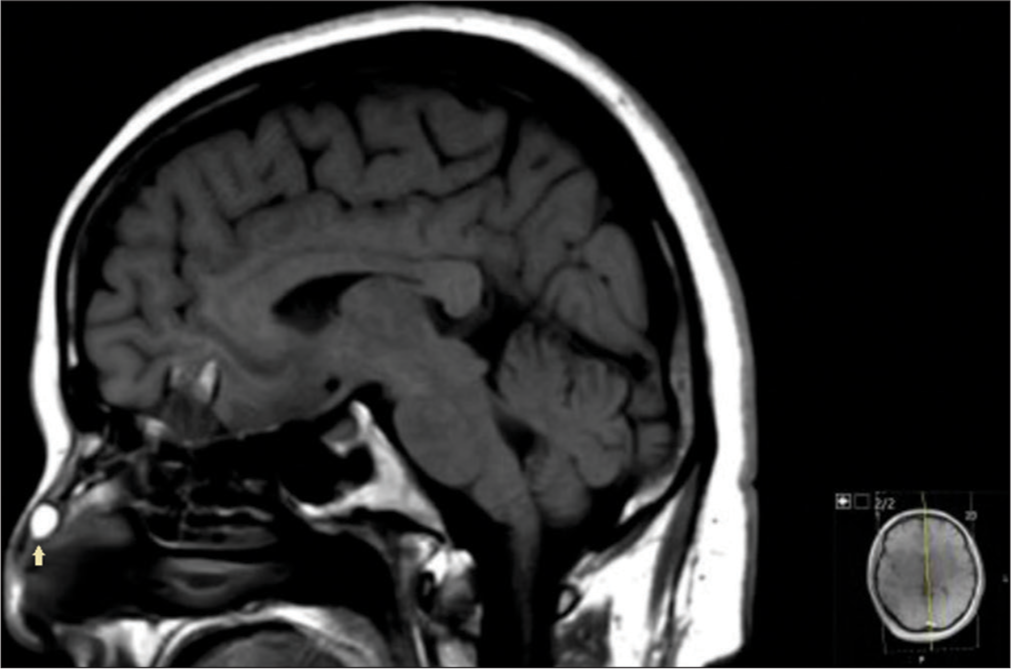
- Sagittal T1-weighted magnetic resonance imaging (MRI) showing hyperintense nodular lesion in the nasal dorsum (yellow arrow).
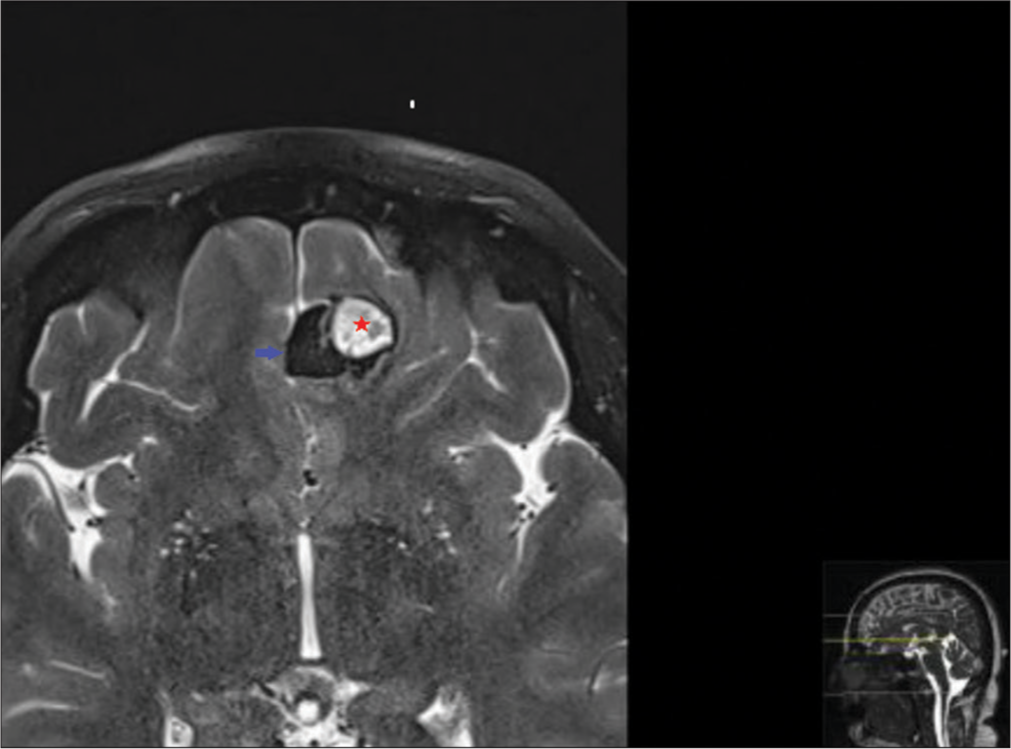
- Axial fat suppressed T2-weighted magnetic resonance imaging (MRI) showing lesion located in the left olfactory sulcus with hypointensity corresponding to the ossified area in the medial (blue arrow) and cystic hyperintensity in the lateral (red star).

- Sagittal reformatted computed tomography (CT) showing intracranial ossified area (red arrow), the canal of the atretic sinus tract extending within the frontal bone (yellow star) and nodular fat density in the nasal dorsum (black arrow).
DISCUSSION
While all midline nasal masses are seen in 40,000 living creatures every 20,000, NDSCs represent more than half, followed by hemangiomas and, less frequently, gliomas and encephaloceles.3 The pathogenesis of NDSCs is not fully understood, but several theories have been proposed. The predominant theory is the “prenasal theory,” which was first described by Grunwald in 1910 and later theorized by Pratt in 1965.4 Pratt suggested that nasal gliomas, encephaloceles and NDSCs share a common embryological pathway. The Dura passes into the nose through the unfused bones of the cranial floor in the 2nd month of pregnancy and is located near the nasal tip dermis. If ossified bones fail to separate the dura from the nasal dermis, it may occur in one out of three congenital malformations.2 This theory may explain the location of the pit of an NDSC located in the median line of the nasofrontal region from the glabella to the columella. The differential diagnosis based on location includes epidermal inclusion cyst, glioma, meningomyelocele, meningoencephalocele, teratoma, teratoid cyst, thyroglossal duct cyst, branchial cleft cyst, and benign lymphadenopathy. A medical history and physical examination are required to evaluate these lesions.5 The existence of nasal dermoid operation history in our case supports the diagnosis.
The epidermoid is usually found at the tip of the nose or in the perinasal region. Unlike other facial dermoids, an NDSC can extend into deeper structures and sometimes extend intracranially.3 Pathological signs show NDSC walls lined with keratinized squamous epithelial and skin extensions containing hair follicles, sebaceous glands, sweat glands, and fibroadipose tissue.5 Intracranial extension causes serious complications such as meningitis, osteomyelitis, abscess formation, hydrocephalus, seizures, and personality changes. All patients with NDSC should be considered to have a potential intracranial extension and should, therefore, undergo pre-operative radiological evaluation.6 Radiological techniques include simple X-rays, fistulography, CT, and MRI. The study should include fine CT, and supplementary MRI should be considered if intracranial extension is a concern. Some authors considered MRI alone to be the most cost-effective and accurate way of evaluating nasal dermoids and necessary for pre-operative planning.6 However, in our case, the superiority of CT to MRI in the evaluation of the ossified area, which has some bone cortex belonging to the intracranial component, stands out. Definitive treatment of nasal dermoid cysts is surgery, and if there is an intracranial extension, excision should be done with craniotomy. Nasal dermoid recurrence rate is low, but can occur several years after the first surgery. Therefore, long-term follow-up of all patients with a history of nasal dermoid is important.7
Although NDSCs are rare in adults, the possibility should be considered in the differential diagnosis of mass in or around the nose. Furthermore, in our case, the ossified intracranial component mimics a calcified meningioma on MRI. Therefore, the nasal area should be carefully investigated in terms of possible nasal dermoid extension in extra-axially located atypical frontal masses. The clinical presentation of NDSC in an adult is similar to that seen in a child. Most patients present with a midline mass in the nasal region and cutaneous sinus. In our case, although there was no inspection finding in the nasal region, there was a non-specific headache that was present in the last decade and may be due to intracranial extension. In our case, it is understood how valuable radiology, together with medical history, is in the diagnosis of an asymptomatic patient.
CONCLUSION
MRI imaging plays an important role in the diagnosis of NDSCs that have no examination findings in the nasal region and appear as an intracranial mass, as in our case.
Authors’ contributions
Gokce A. and Onbas O.: Acquisition, analysis, and interpretation of data: Gokce A.: Drafting of the manuscript.: Onbas O.: Critical revision of the manuscript.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of ınterest.
Artificial intelligence declaration statement
The authors confirm that there was no use of artificial ıntelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Nasal dermoid sinus cyst in a young girl: A case report. J Dermatol. 2018;45:e132-3.
- [CrossRef] [Google Scholar]
- Adult nasal dermoid sinus cyst. Am J Otolaryngol. 2005;26:403-5.
- [CrossRef] [PubMed] [Google Scholar]
- Intracranial extension of a nasal dermoid sinus cyst in a 56-year-old man. Head Neck. 1994;16:366-71.
- [CrossRef] [PubMed] [Google Scholar]
- Midline cysts of the nasal dorsum: Embryologic origin and treatment. Laryngoscope. 1965;75:968-80.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric dermoid cysts of the head and neck. Otolaryngol Head Neck Surg. 2005;132:938-42.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging and surgical approach of nasal dermoids. Int J Pediatr Otorhinolaryngol. 2002;62:111-22.
- [CrossRef] [PubMed] [Google Scholar]
- Endonasal endoscopic approach for intracranial nasal dermoid sinus cysts in children. Int J Pediatr Otorhinolaryngol. 2012;76:1217-22.
- [CrossRef] [PubMed] [Google Scholar]






