Translate this page into:
Relatively uncommon presentations of the ubiquitous acrochordon – A brief review
*Corresponding author: Sujata R. Mehta-Ambalal, Department of Dermatology, Skin clinic @ Sumeru and Shilp Clinic; SHREI, Ahmedabad, Gujarat, India. sujata.ambalal@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mehta-Ambalal SR, Verma S, Arora S, Behera B, Ramamoorthy R, Janney M. Relatively uncommon presentations of the ubiquitous acrochordon – A brief review. J Cutan Aesthet Surg. doi: 10.25259/jcas_158_23
Abstract
Acrochordons are ubiquitous and rarely command our attention. In this review, we look at their usual as well as unusual presentations. We also attempt to refresh our understanding of and provide new insights on this oft taken for granted lesion.
Keywords
Acrochordons
Skin tags
Fibroepithelial polyp
INTRODUCTION
Acrochordons are one of the most common benign neoplasms of the skin. They are variably known as skin tags (ST), fibroepithelial polyps (FEP), and soft fibromas. We herein share a few not so commonly encountered presentations of this commonly seen entity. We take the liberty of elaborating on the pathogenesis and the histological aspects of STs.
Pathogenesis
The exact etiopathogenesis of acrochordons continues to remain obscure. They are often associated with obesity. The risk of occurrence and prevalence of metabolic syndrome or its components (abdominal obesity, high fasting glucose or type 2 diabetes mellitus, hypertension, high triglycerides, and low high-density lipoprotein) is higher in patients with STs.1-3 The relative risk of developing metabolic syndrome in those with STs is 11.13 times higher than in controls. Different studies have found significant associations with individual components of metabolic syndrome in various permutations and combinations. The presence of metabolic syndrome is independent of the number, color, and size of STs.4 Hormonal influence of progesterone and estrogen contributes to the female predilection in pregnancy.5 Hyperinsulinemia, as well as female hormone levels, have been found to be related to elevated levels of epidermal growth factor and transforming growth factor with an upregulation of their receptors. Mutations in fibroblast growth factor receptor, Ras, and thyroid nuclear receptor thyroid hormone receptor alpha gene predispose to skin tumorigenesis and acrochordon formation.6,7 Obesity leads to hyperinsulinemia, which in turn increases insulin-like growth factor (IGF) levels. There is a strong expression of IGF-1 in both epidermis and dermal elements, especially the endothelium of STs. IGF-1 is implicated in hyperproliferative hyperplastic skin conditions. By an autocrine effect, IGF-1 produced by dermal fibroblasts leads to the formation of loose and extra connective tissue. By a paracrine effect, it stimulates keratinocytes, causing hyperkeratosis and acanthosis with or without papillomatosis. Both subsequently lead to the formation of acrochordons.8
The role of skin irritation in the form of chronic friction and pressure has often been mentioned, considering the propensity of STs to develop in areas prone to friction, such as the neck, axillae, and groin. However, a plausible explanation has never been forthcoming in literature. Skin aging with resultant loss of elasticity has been proposed to be a contributory factor. STs arise in sites subjected to trauma. Mast cells are recruited to sites of skin trauma as a response to injury and increase their tumor necrosis factor-alpha (TNF-α) content. Increased mast cell infiltrate, elevated TNFα levels and increased TNF-related apoptosis-inducing ligand, another member of the TNFsuperfamily, were reported in STs compared to controls.9
Human papillomavirus (HPV) deoxyribonucleic acid (DNA) has been detected in some samples of STs analyzed despite their non-contagious nature, suggesting it is a cofactor in the pathogenesis. Various genotypes, including the high-risk types 16 and 18, have been detected. However, the lack of viral transcripts indicates a latent infection.10 Therefore, the causal role of HPV in acrochordons is not clear.
Clinical features
Acrochordons most frequently present as small, pedunculated lesions anywhere on the skin. Although considered trivial, some may occasionally become mentally as well as physically bothersome because of an unusual appearance or associated symptoms such as itching pain or rubbing against clothes.2
Sex
Although some studies have found a female predilection, others have failed to observe a particular gender predominance.3 Acrochordons occurring during pregnancy have been called fibroma molluscum gravidarum.11 Their onset is during the 4th–6th months of pregnancy, and they usually disappear after parturition. They have been found to persist and undergo a continued increase in size during subsequent pregnancies.12
Age
Once an ST has developed, it may increase in size or number with advancing age. The risk of getting STs increases with age. After age 40, the frequency of STs is ~37%.13 By the fifth to sixth decade, close to two-thirds of individuals may develop acrochordons, which usually remain until the end of life. The age of 50, however, seems to be a turning point at which a stagnation of the increase is observed.14 However, the size of previously unnoticed lesions may increase, which then makes acrochordons noticeable and provokes anxiety in many individuals.
Presentation
Acrochordons are usually pedunculated with a thin stalk measuring 0.5–2.5 mm in diameter. They often appear round and soft, and most are diagnosed simply by naked eye examination. They may be skin colored or hyperpigmented.
STs are mostly found in areas of friction: the axilla, followed by the neck and groin. They are known to develop over sites of acanthosis nigricans, including on facial acanthosis nigricans. Other localizations are the face, especially eyelids, inframammary region, abdomen, and back.14
Acrochordons have the following general descriptions:
Small STs: Furrowed papules of approximately 1–2 mm in width and height, most frequently appearing on the neck and the axillae
Mid-sized STs: Solo or multiple filiform STs that are roughly 5 mm long and 2 mm wide, occurring at other sites on the body
Large-sized STs: Pedunculated lesions that may demonstrate a nevoid, bag-like appearance or soft fibromas usually located on the lower part of the body groin.
They occasionally grow more than 5 cm in size, and these are called giant FEP. Acrochordons larger than 15 cm have been reported over the vulva, axilla, and thigh.15
Rare reports exist of acrochordons occurring over unusual locations against the backdrop of specific clinical circumstances, like the location of a giant FEP near ventriculoperitoneal shunt on pre-sternal site,16 or penis associated with condom catheter,17 or under prolonged influence of hormones in the genital tract.18
A sudden change in its shape and size or development of symptoms such as pain and bleeding is accompanied by a sense of urgency leading to an emergency consultation, extreme concern about the nature of the change, anxiety related to a possible malignancy, and quick remedial action.
We share some examples of varied presentations collected over the past 5 years in a private clinic (SV) [Figures 1-20].19,20

- Multiple small, occasionally pigmented acrochordons that can be mistaken for dermatosis papulosa nigra.

- Various morphologies and sizes of acrochordons on the neck. Small pigmented, round acrochordons, with smooth and rough surfaces coexisting with a filiform pigmented one in the lower right corner and a larger, non-pigmented tumid one in the center of the image.

- Axilla showing elongated, pedunculated, and convoluted acrochordons superimposed on acanthosis nigricans, a common finding in obese patients.

- Small skin tags under 2 mm in size seen through a dermatoscope.
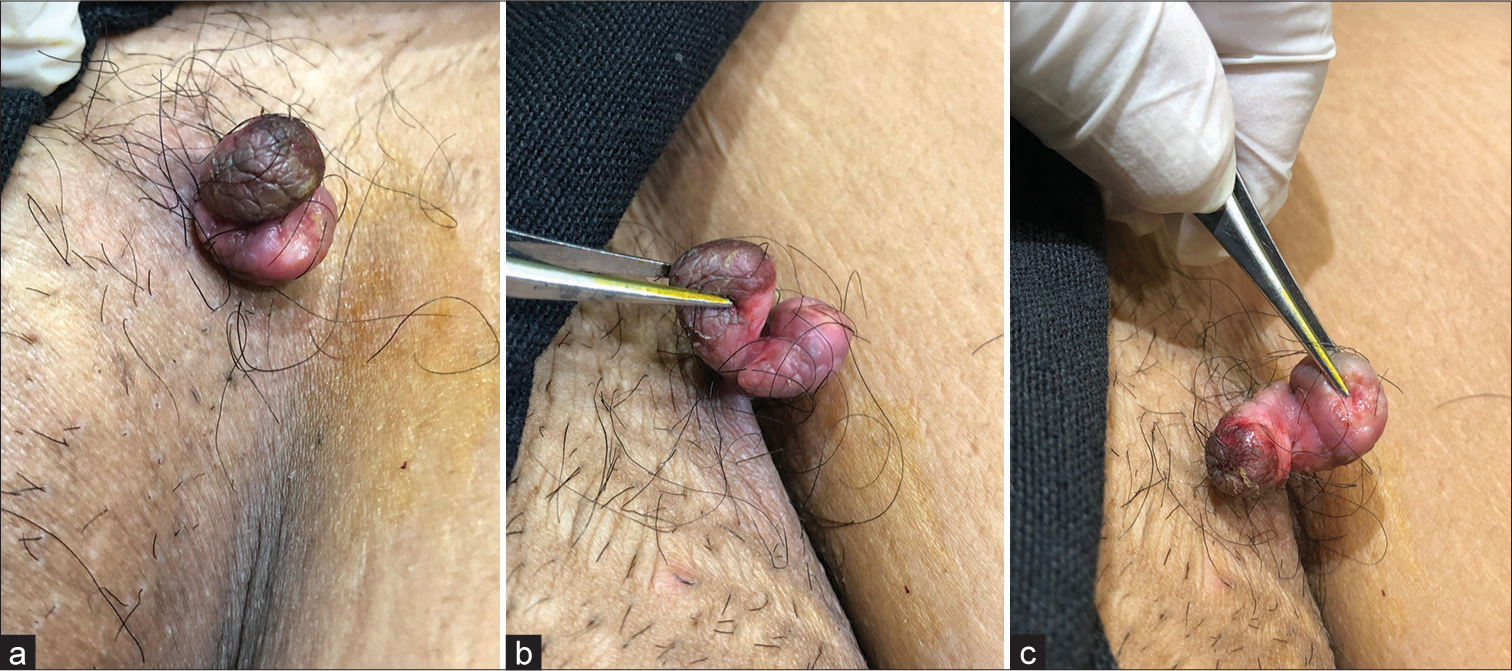
- (a) Bilobed acrochordon in groin arising from a single stalk. (b) One lobe is pigmented and rugose, while the other is skin colored and swollen. (c) Adjacent surfaces show inflammatory changes.

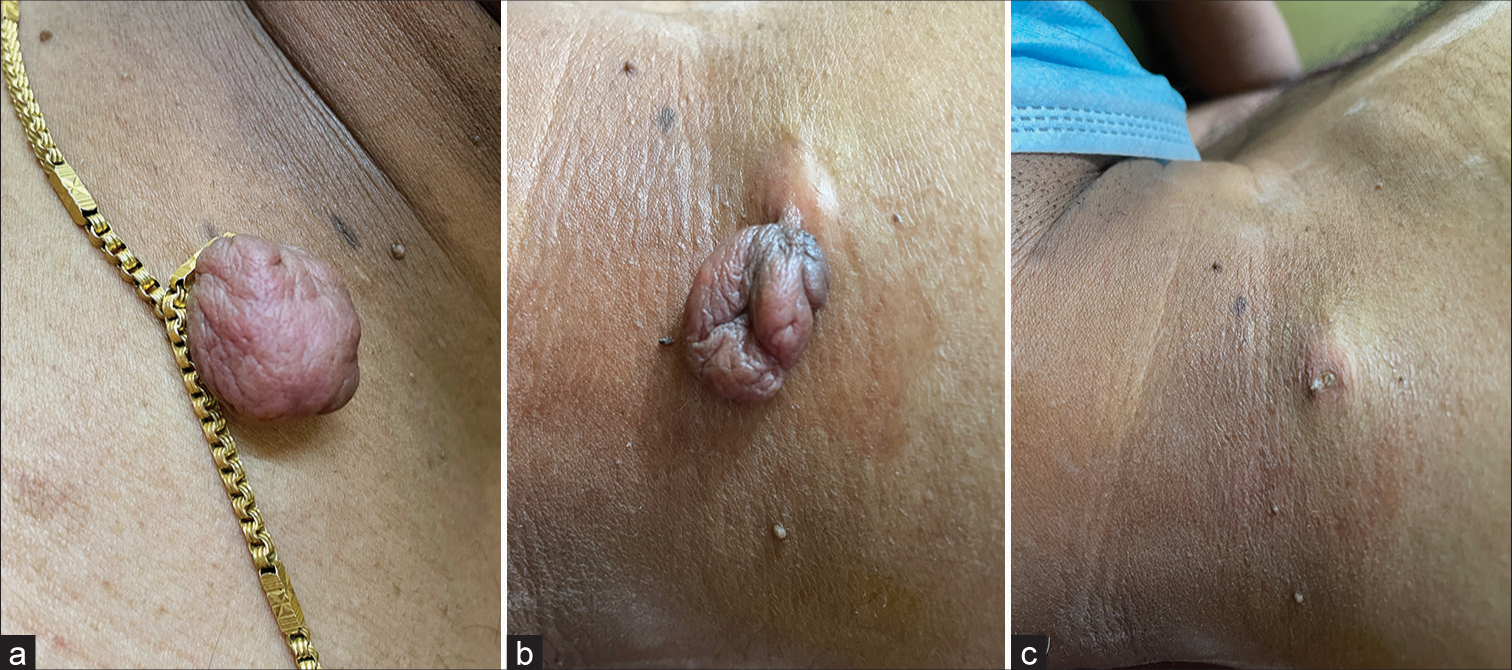
- (a and b) Areolar skin tag with an eroded undersurface. (c) Base after removal by radiofrequency cautery.
- (a) Skin tag (ST) engorged due to neck chain strangulating the stalk. (b,c) Swollen base of ST before and after radiofrequency cautery.

- (a and b) Skin tag on the lower eyelid, strangulated by a blue and white thread that was visualized by dermoscopy. (c) Post-cautery image.

- Flattened pancake-like cerebriform skin tag with a small stalk.

- Skin tag with dark black coal-like surface.

- Linear arrangement of skin tags overlying acanthosis nigricans.

- Skin tag over labia majora, (a) Before and (b) After radiofrequency ablation.

- Skin tag on labia minora.
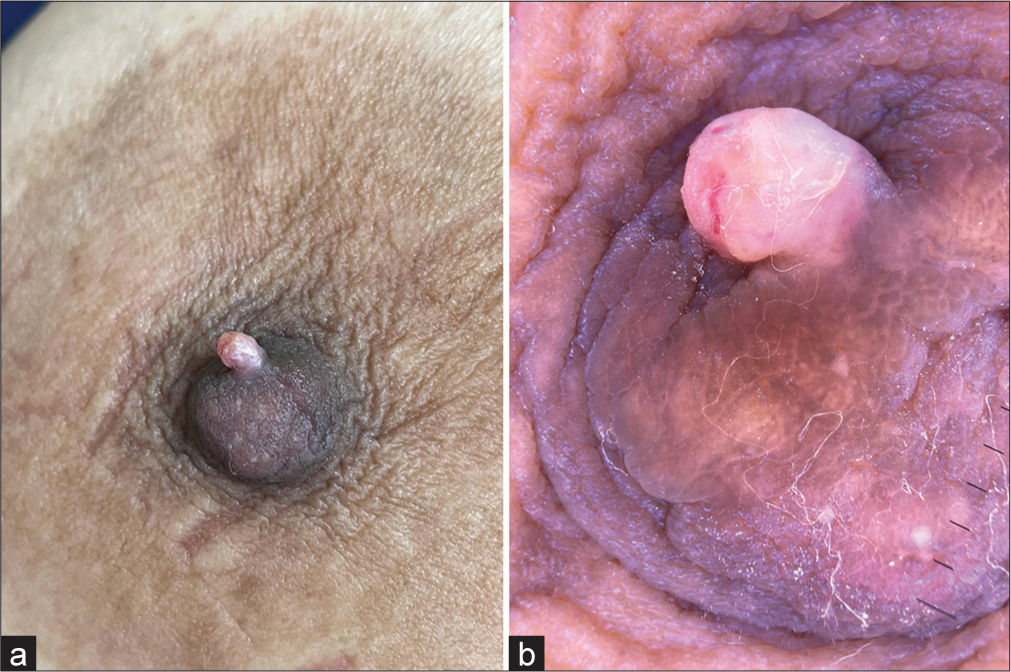
- (a) Flesh-colored skin tag over the nipple. (b) The same lesion was visualized on the dermatoscope.

- Pigmented, cerebriform skin tag on the base of penile shaft mimicking a seborrheic keratosis.

- Large skin tag on the scrotum adjacent to the penis.

- Tiny, depigmented skin tags on the eyelid margin of a vitiligo patient.

- Relatively sessile acrochordon with a pendulous distal end.

- Peniform acrochordon next to said appendage.

- Peniform acrochordon with a warty surface.
Differential diagnosis
Acrochordons may resemble or mimic nevi, papillomas, verrucae, molluscum contagiosum, neurofibromas, seborrheic keratoses, dermatosis papulosa nigra, milia, cutaneous malignancies, and many more entities.
Investigations
Diagnosis is clinical. Excisional biopsy is considered prudent in case of doubt, especially in case of unusual appearance, rapid growth, and bleeding. The importance of documentation of the diagnosis in such cases cannot be overemphasized. While there may be no merit in subjecting common variants of skin tags routinely for histopathological examination, any unusual appearance merits a biopsy for the purpose of documentation.
Histopathology
The histopathology of the skin tag will reveal an attenuated epidermis, a flattened basal cell layer, and often increased pigmentation [Figure 21]. The furrowed papules show epidermal hyperplasia and sometimes horn cyst formation. These lesions have surface changes like those seen in seborrheic keratosis and are most common on the neck and eyelids. The filiform lesions have an epidermis with only mild acanthosis. Pagetoid dyskeratosis is sometimes an incidental finding in the overlying epidermis. The extra mass is composed of loose fibrous tissue. Histology of the pedunculated skin lesion will reveal the presence of mild hyperkeratotic epidermis, containing blood vessels of various sizes in the dermal stroma. Acrochordons are usually identified by their flattened, acanthotic, presentation, or “flowery” pattern-like epithelium.
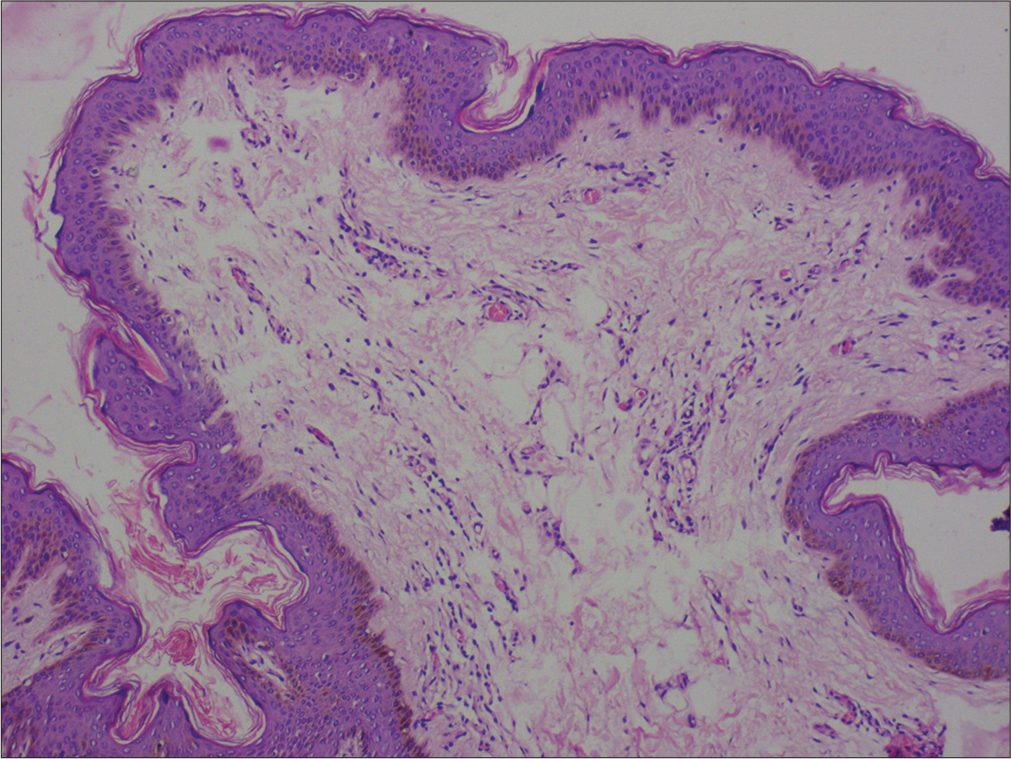
- Histopathology of a skin tag. Normal to the minimally atrophic epidermis, increased basal layer pigmentation, loosely-arranged thin collagen fibers in the dermis, and increased blood vessels (Hematoxylin and eosin, ×100).
The dermal layer usually has loosely arranged collagen fibers along with lymphatic vessels and dilated capillaries. Elastic fibers are present in normal amounts. A few fat cells and, sometimes, nevus cells may be present. The larger, bag-like lesions (fibrolipomas) usually have a stroma composed of loosely arranged collagen and a central core of adipose tissue. Appendages are generally not seen in the classic lesion.3 The mass is connected to the skin by a narrow and thin pedicle composed of well-vascularized and loosely arranged collagen.
On scanning view, the acrochordon has a polypoid configuration. The tumor comprises a central loose fibrocollagenous tissue and blood vessels surrounded by a hyperplastic and papillomatous epidermis. It is usually devoid of adnexal structures. The epidermal findings may vary based on the clinical morphology; a furrowed papule may have epidermal hyperplasia with horn cyst formation, and the filiform and polypoid papules may show mild acanthosis. Based on epidermal proliferation patterns, they can be confused with seborrheic keratosis, verruca vulgaris, and acquired digital fibrokeratoma, among others. Features suggestive of trauma, such as epidermal necrosis, ulceration, pagetoid dyskeratosis, lichen simplex chronicus-like, and lichen sclerosus-like changes may be observed. The changes should be interpreted keeping in line with the clinical morphology. The presence of pagetoid dyskeratosis mandates ruling out Paget’s disease, melanoma, clear cell papulosis, and koilocytes.21,22 A varying number of adipocytes can be noted in relatively larger acrochordons, named lipofibroma. The adipocytes with the acrochordon are not an independent indicator of underlying diabetes or metabolic syndrome.23 Lymphedematous FEPs of the glans penis and prepuce demonstrate prominent dermal edema, increased cellularity, dilated vessels, and inflammatory infiltrate, including mast cells and scattered multinucleated giant cells. In addition, the vaginal lesion can be found to have myxoid changes.17 A variant, called cutaneous pseudosarcomatous polyp, displays markedly pleomorphic sarcomatoid cells; however, clinically, these have a benign course. They may contain widely separated pleomorphic stellate stromal cells and multinucleated cells in a myxoid to collagenous stroma. The pleomorphic cells stain diffusely positive for vimentin and negative for desmin and smooth muscle actin. In addition, a variable positive for CD 34 and factor XIIIa can be noticed. These can be confused with pleomorphic fibroma, dermatofibroma with monster cells, and pleomorphic lipoma.24
Clinical and laboratory evaluation
Any patient with new onset or enlarging acrochordons should be thoroughly evaluated for signs of insulin resistance-like acanthosis nigricans. Waist circumference, blood pressure, blood sugar, and lipids should be checked. Hormonal disturbances such as polycystic ovary syndrome and thyroid disease should also be ruled out.25,26
Treatment
Acrochordons, especially over the face and neck, are of significant cosmetic concern and patients seek treatment despite the reassurance regarding its benign course. In some instances, unusually large/atypical acrochordons not only cause discomfort but also adversely affect a patient’s quality of life.
The topical or local injectable anesthetic can be used before removal. Small, sessile acrochordons are ablated with radiofrequency/electrocautery or LASERs (nanosecond Q-switched Nd:Yag or CO2 laser), whereas large, pedunculated acrochordons can either be cut at the base of the stalk with an iris scissor (snip excision) or ablated by above-mentioned methods while gently pulling the acrochordon for adequate visualization of base. This is popularly known as the “pull and cut” approach.27 Giant acrochordons with a broader base leave behind bigger defects and hence are excised and sutured for better outcomes.
Cryotherapy has been increasingly used in recent times to treat acrochordons. In the open spraying technique, liquid nitrogen is sprayed over skin tags from 1 to 1.5 cm for about 20–30 s to produce a small ice ball. Alternatively, earbuds or forceps dipped in liquid nitrogen can be used as applicators. Cotton-tipped applicators are used to treat smaller acrochordons and are placed directly over them. Pedunculated acrochordons are best treated by pinching their base with forceps.28 Two to three freeze-thaw cycles might be required based on the size of the acrochordon. It is important to protect the adjacent areas and be precise in application to avoid complications. Handheld cryotherapy pens with refillable cartridges of nitrous oxide dimethyl ether achieve −80°C–−90°C in tissues and are the latest addition to our armamentarium.29 These procedures are mostly safe, and complications such as bleeding, infection, delayed wound healing, and post-inflammatory dyspigmentation are rarely encountered.
Other treatment methods include ligation of acrochordons with suture, copper wire, or dental floss to occlude blood supply and cause ischemic necrosis. These techniques are painful and slow and are rarely followed by medical practitioners.
Given the risk of development of metabolic syndrome, patients should be encouraged to modify their lifestyle, including dietary calorie restriction and increased physical activity.30
CONCLUSION
Skin tags are extremely common in middle aged, obese patients. Apart from reassuring patients and offering them the choice of removal, the clinician must keep an eye open for underlying systemic associations.
Authors’ contributions
First draft, final draft and correspondence: Sujata R. MehtaAmbalal, conceptualization, periodic review of manuscript and photographs: Shyam Verma, histopathology photograph: Biswanath Behera. Text: All authors.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Cutaneous stigmata associated with insulin resistance and increased cardiovascular risk. Int J Dermatol. 2014;53:1062-9.
- [CrossRef] [PubMed] [Google Scholar]
- Association of skin tag with metabolic syndrome and its components: A case-control study from Eastern India. Indian Dermatol Online J. 2019;10:284-7.
- [CrossRef] [PubMed] [Google Scholar]
- A clinical study of skin changes in pregnancy. Indian J Dermatol Venereol Leprol. 2007;73:141.
- [CrossRef] [PubMed] [Google Scholar]
- Frequent FGFR3 and ras gene mutations in skin tags or acrochordons. J Invest Dermatol. 2021;141:2756-60.e8.
- [CrossRef] [PubMed] [Google Scholar]
- Germ line mutations in the thyroid hormone receptor alpha gene predispose to cutaneous tags and melanocytic nevi. Thyroid. 2021;31:1114-26.
- [CrossRef] [PubMed] [Google Scholar]
- Role of insulin-like growth factor-1 in skin tags: A clinical, genetic and immunohistochemical study in a sample of Egyptian patients. Clin Cosmet Investig Dermatol. 2019;12:255-66.
- [CrossRef] [PubMed] [Google Scholar]
- The possible role of trauma in skin tags through the release of mast cell mediators. Indian J Dermatol. 2011;56:641-6.
- [CrossRef] [PubMed] [Google Scholar]
- Human papillomavirus in skin tags: A case series. Dermatol Pract Concept. 2018;8:295-6.
- [CrossRef] [PubMed] [Google Scholar]
- Fibroma molluscum gravidarum: A new clinical entity. Am J Obstet Gynecol. 1906;53:191-9.
- [Google Scholar]
- Connective tissue physiologic changes during pregnancy In: Obstetric dermatology: A practical guide. Germany: Springer; 2008. p. :25-31.
- [Google Scholar]
- Association of acanthosis Nigricans and skin tags with insulin resistance. An Bras Dermatol. 2012;87:97-104.
- [CrossRef] [PubMed] [Google Scholar]
- Skin tags: Localization and frequencies according to sex and age. Dermatologica. 1987;174:180-3.
- [CrossRef] [PubMed] [Google Scholar]
- Giant acrochordon arising from the thigh. J Coll Physicians Surg Pak. 2015;25:839-40.
- [Google Scholar]
- Giant fibroepithelial polyps: Why do they grow excessively? Sisli Etfal Hastan Tip Bul. 2020;54:257-60.
- [Google Scholar]
- Lymphedematous fibroepithelial polyps of the glans penis and prepuce: A clinicopathologic study of 7 cases demonstrating a strong association with chronic condom catheter use. Hum Pathol. 2004;35:190-5.
- [CrossRef] [PubMed] [Google Scholar]
- Giant acrochordon of vulva: A rare occurence. Nepal J Dermatol Venereol Leprol. 2015;13:70-2.
- [CrossRef] [Google Scholar]
- Obese male with linear skin tags: Looking beyond the role of obesity and insulin resistance. Indian J Dermatol Venereol Leprol. 2024;90:356-7.
- [CrossRef] [PubMed] [Google Scholar]
- Verruca plus acrochordon: An “over the top” skin tag. Clin Exp Dermatol. 2009;34:e432-3.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative study of pagetoid dyskeratosis between acrochordons and soft fibromas. Am J Dermatopathol. 2006;28:478-81.
- [CrossRef] [PubMed] [Google Scholar]
- Acrochordon with histological features of lichen sclerosus. Am J Dermatopathol. 2019;41:e64-5.
- [CrossRef] [PubMed] [Google Scholar]
- Adipocytes in fibroepithelial polyps are not related to diabetes mellitus or obesity. J Am Acad Dermatol. 2018;79:1154-5.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous pseudosarcomatous polyp: A recently described lesion. Ann Diagn Pathol. 2008;12:440-4.
- [CrossRef] [PubMed] [Google Scholar]
- A study of androgen and estrogen receptors alpha, beta in skin tags. Indian J Dermatol. 2010;55:20-4.
- [CrossRef] [PubMed] [Google Scholar]
- The association of various metabolic parameters with multiple skin tags. J Clin Aesthet Dermatol. 2018;11:40-3.
- [Google Scholar]
- Just a pinch: Technique for skin tag removal in sensitive areas. Can Fam Physician. 2016;62:998-9.
- [Google Scholar]
- Efficacy evaluation of the pixie(®) skin tag cryogenic device on skin tags in a prospective, single-blinded, randomized, comparative clinical trial. Dermatol Ther (Heidelb). 2021;11:995-1007.
- [CrossRef] [PubMed] [Google Scholar]
- Metabolic syndrome and skin: Interactions and implications. Indian J Dermatol. 2022;67:138-45.
- [CrossRef] [PubMed] [Google Scholar]







