Translate this page into:
Optimizing management of secondary changes in port-wine stains: Navigating resource constraints with staged debulking surgery and radio frequency ablation
*Corresponding author: Guneet Awal, Department of Dermatology, Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, Punjab, India. guneetawal@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Awal G, Shubham, Singh A. Optimizing management of secondary changes in port-wine stains: Navigating resource constraints with staged debulking surgery and radio frequency ablation. J Cutan Aesthet Surg. doi: 10.25259/JCAS_15_2024
Abstract
Port-wine stains (PWSs) are low-flow congenital capillary malformations showing a progressive ectasia of superficial cutaneous vascular plexus in the skin. Congenital PWS has a 0.3% incidence rate and is most frequently observed on the face and neck, though it can also appear on other regions of the body. PWS does not involute over time, but rather, if untreated in the early years of life, they may later develop nodularity and hypertrophy, which respond poorly to existing treatment modalities and cause significant psychosocial distress to the patient. We present a case series of patients with PWS managed with staged surgical resections and radiofrequency ablation.
Keywords
Port-wine stains
Nodularity
Debulking
Radiofrequency ablation
INTRODUCTION
Port-wine stains (PWSs), congenital vascular malformations affecting 0.3–0.5% of newborns, result from a malfunction in the local sympathetic nervous system.1-4 Evolving into raised, red or purple patches, nodules, or plaques, PWS may develop hypertrophy, pyogenic granulomas, and, rarely, intralesional carcinoma.5-11 Despite various treatment modalities, effective treatments remain elusive.12 Long-standing cases with nodules and soft-tissue hypertrophy show minimal success with pulsed dye laser (PDL) laser, emphasizing the need for surgical interventions such as resections and flap repairs.13-15 This case series presents three PWS patients managed successfully through staged surgical resections and radiofrequency ablation.
CASE REPORT
Case 1
A 50-year-old male presented to the outpatient department (OPD) of dermatology of a tertiary care hospital with a complaint of asymptomatic reddish patches and nodules involving the left side of his face since birth. The patch started from a reddish discoloration over the left malar region, zygomatic region, and upper lip. The lesion was left untreated. At the age of 20 years, he started to have progressive thickening of the lesion along with the development of multiple nodularities in it, which also were progressive in size. These nodular lesions were disfiguring to overall facial symmetry, distorting the anatomy of the upper lip on the left side. This caused problems while consuming food and a reduction in the visual field in the inferior and lateral aspects of the left eye. There was a history of frequent erosions on the nodules. This caused significant physical and emotional distress to the patient, leading to social stigma and poor quality of life.
Dermatological examination revealed a diffuse, partially blanchable erythema extending from the left zygomatic arch to the margins of the upper lip on the left side. There were also multiple discrete irregularly shaped reddish-purple nodules of size 0.5––2.5 cm [Figure 1a].
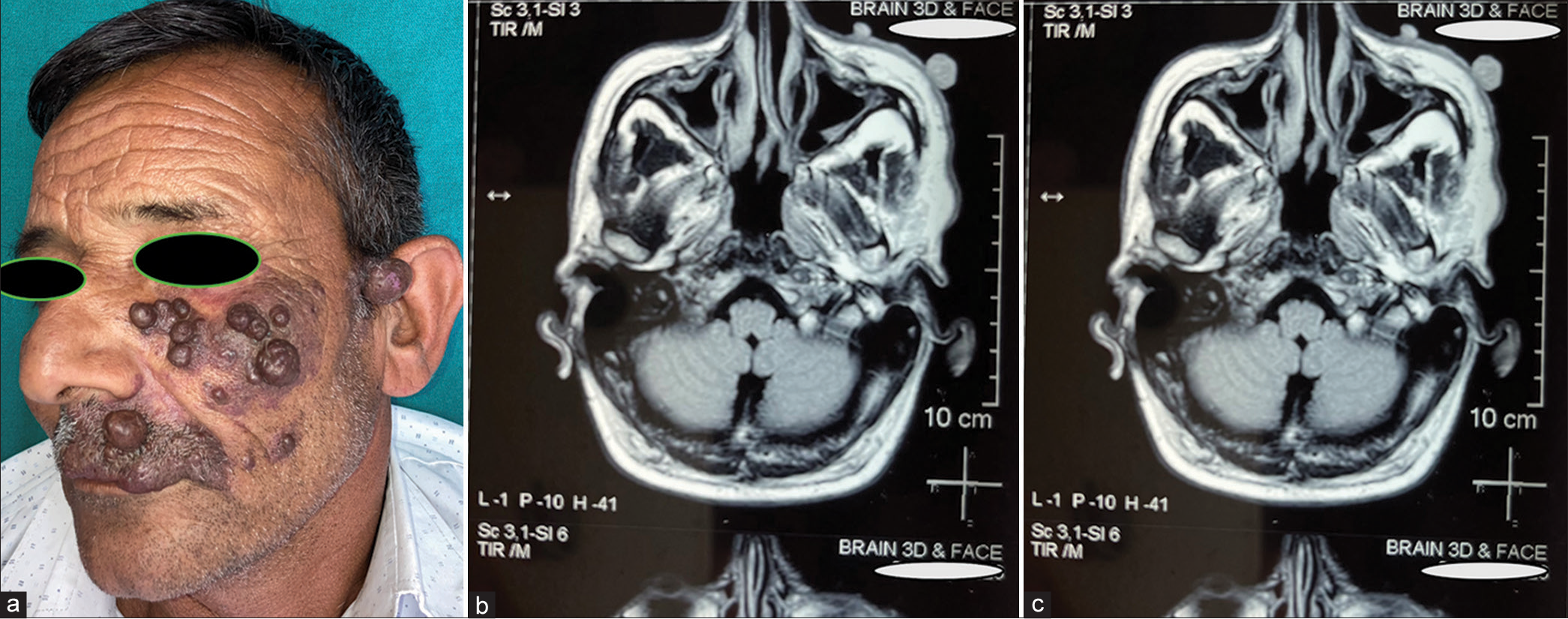
- (a) Multiple reddish-purple nodules occupying the left side of the face in a patient with port-wine stains (PWS). (b) High-power view of PWS showing dilated superficial dermal blood vessels and endothelial proliferation along with fibro-collagenous tissue with intervening adnexal structures (hematoxylin and eosin ×400). (c) Magnetic resonance imaging showing multiple skin-based nodular lesions with exophytic components (T1 weighted).
On the basis of the clinical examination, a provisional diagnosis of PWS was made, and the patient was investigated. The histopathological examination revealed scattered dilated blood vessels with blood elements and endothelial proliferation in the dermis and fibro-collagenous tissue with adnexal structures in the intervening, suggestive of cavernous hemangioma [Figure 1b]. There was neither an inflammatory infiltrate nor any atypical cells. This helped to confirm our diagnosis and ruled out malignancy. Magnetic resonance imaging revealed multiple skin-based nodular lesions with exophytic components [Figure 1c].
Laser therapy was discussed with the patient, but he declined this treatment option for the lesion due to inaccessibility and high cost.
In consultation with the plastic surgery department, the patient was taken up for serial debulking under general anesthesia using a two-stage approach. In the first stage, large nodular lesions from zygomatic, infra-orbital, and supra-labial regions were resected, followed by subcutaneous closure with buried non-absorbable sutures and cutaneous closure with interrupted Prolene sutures [Figure 2a]. The sutures were removed at a follow-up after 7 days. After this, monthly follow-up was done. A second stage resection was done at 2 months in which smaller nodules, mainly from the zygomatic, labial, and supra-labial region, were resected and closed in a single layer with non-absorbable (Prolene) sutures.

- (a) Intraoperative picture during first stage surgical resection after removal of nodular lesions from the molar and zygomatic region. (b) At 1 month follow-up, showing improvement in facial symmetry and visual field. At this stage, radiofrequency ablation was deployed to remove smaller lesions. (c) At the 6-month follow-up showing improved facial symmetry and topography with no evidence or recurrence of nodules/hypertrophy.
After 1 month, there was a significant improvement in the facial symmetry and visual field of the patient [Figure 2b]. At 1 month follow–up, after, radiofrequency ablation (RFA) was deployed for removal of the remaining nodules and hypertrophic lesions. This led to cosmetic improvement through improved topography of the lesions [Figure 2c]. The final results were acceptable to the patient, and treatment was considered satisfactory at this stage. There was no recurrence at 6 months follow-up.
Case 2
A 23-year-old male presenting to the OPD had a 15-year history of an erythematous patch on the right side of his face. The lesion was asymptomatic with a history of progressive thickening for the past 6 years and the formation of a few dome-shaped lesions on top of these lesions and a few embedded papules. This was a reason for concern for him. There was no h/o trauma, seizures, or family history of similar lesions. On examination, there was a single well-defined dull erythematous patch of size 15 cm × 10 cm with many pinhead-sized embedded papules on the cheek area along with three discrete subcentimetric, soft, and compressible nodularities [Figure 3a]. A clinical diagnosis of PWS was made, and a biopsy taken from one of the nodularities showed few dilated capillaries and endothelial proliferation in the dermis. A Dermaindia MEGASURG Gold monopolar RF device was used to deploy RFA energy at intensities ranging from 2–5 until the nodularities got removed and underlying tissue exhibited whitish discoloration. There was bleeding with the initial stroke of the probe, but it quickly stopped in the deeper layers of the lesion. Complete hemostasis was achieved without the need for any sutures [Figure 3b]. At a follow-up after 1 week, good cosmetic results were noted after a single session of RFA, and the concerns of the patient with regard to nodularities could be addressed effectively.

- (a) Single erythematous patch of size 15 cm × 10 cm with multiple embedded papules along with three discrete subcentimetric nodularities (arrows). (b) After radio frequency ablation deployment at the three nodular lesions, showing achievement of hemostasis (arrows).
Case 3
A 40-year-old male presenting to the OPD had a history of a reddish patch on the left upper arm region since birth with a pedunculate polypoidal growth over it for the past 2 years, which often bled on manipulation. On examination, there was a bright red patch measuring 12 cm × 8 cm on the posterolateral aspect of his upper left arm with a solitary, erythematous, moist, and inflamed pedunculated polyp of 2 cm diameter [Figure 4a]. A Dermaindia MEGASURG Gold monopolar RF device was used to deploy RFA energy to smoothly excise the lesion through its stalk. Complete hemostasis was achieved by local pressure and gauze soaked with adrenaline. The histopathological examination has consisted of pyogenic granuloma showing polypoid mass with overlying atrophic epidermis showing erosions, multiple capillaries arranged in lobules within the upper dermis with a mixed inflammatory infiltrate within the stroma. On follow-up at 1 month, the lesion had healed with good cosmesis and no sign of recurrence [Figure 4b].
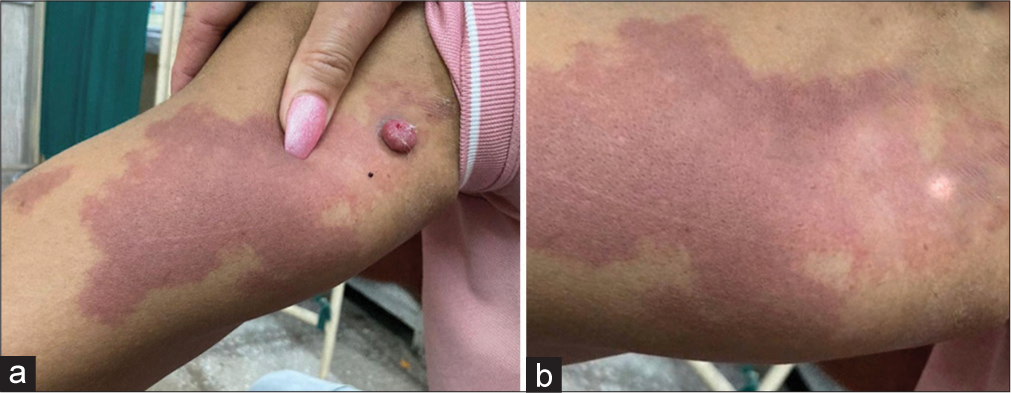
- (a) A bright red patch measuring 12 cm × 8 cm on the posterolateral aspect of the upper left arm with an inflamed pedunculated polyp of 2 cm diameter. (b) At 1 month follow-up, showing no sign of recurrence.
DISCUSSION
Soft-tissue and bone hypertrophy in PWS represents a therapeutic challenge because three-dimensional tissue deformities cannot be corrected with vascular-specific lasers, and thus, surgery becomes the only option.16 Nodular changes in PWS signify pyogenic granuloma and/or arteriovenous malformations within the skin’s vascular structures.17
In the past, surgical management of PWSs was not considered a preferred modality of treatment due to anticipation of excessive hemorrhage. Over the past few years, studies have shed new light on the pathology of PWS. Although hypertrophy involves all the tissue layers, the pathological vessels are located in the superficial part of the dermis. Due to this, there is an increased risk of bleeding only during the initial skin incision. Moreover, these are low-flow malformations consisting of small-diameter vessels, and hence, any bleeding can be easily managed. Therefore, patients with PWS are now considered operable with a manageable risk of bleeding.
According to Yamaguchi et al., another issue is that some of these individuals have syndromic associations that carry a higher anesthetic risk. According to them, utilizing a multidisciplinary team and precise pre-operative preparation could lower this risk.18
Small lesions are amenable to primary closure and resection or RFA with controlled homeostatic measures. Large soft-tissue defects are typically covered with flaps as there is a risk of development of skin contracture, thereby resulting in lip malposition, ectropion, and nostril deformity, among other issues. Split-thickness skin grafting is favored for larger lesions due to superior cosmetic results and reduced risk of complications.14
Bone hypertrophy in PWSs appears to be caused by local hypervascularity surrounding the periosteum; as a result, radical surgery is not a viable option.
Zhou et al., in their study, concluded that whenever dentofacial abnormalities carry a significant negative impact on the patient’s quality of life, undergoing a multi-step surgery for skeletal deformity and soft-tissue correction is advisable.19
In our first patient, the results after two staged resections followed by RFA were satisfactory, and further, treatments were not required.
In the second and third patients, the secondary changes were amenable to RFA and did not require a more invasive surgical approach.
CONCLUSION
Treatment of PWS with soft-tissue hypertrophy through PDL, potassium titanyl phosphate (KTP) 532 laser, photodynamic therapy, and even plastic surgery are not easily accessible, more so in developing parts of the world. As a result, the patient ends up with chronic cosmetic disfigurement, which leads to psychosocial embarrassment to the patient, which hampers their quality of life. Here, staged resection and RFA can be offered with good results and cosmesis.
Authors’ contributions
All the authors contributed equally for study conception and design, data analysis and manuscript preparation.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Clinical study on hemoporfin PDT for infant facial port-wine stains. Photodiagnosis Photodyn Ther. 2019;25:106-10.
- [CrossRef] [PubMed] [Google Scholar]
- Port-wine stains. A disease of altered neural modulation of blood vessels? Arch Dermatol 1986. ;. ;122:177-9.
- [CrossRef] [PubMed] [Google Scholar]
- Reduced vasoactive responses in port wine stains. Br J Dermatol. 1990;122:615-22.
- [CrossRef] [PubMed] [Google Scholar]
- Capillary malformations (portwine stains) of the head and neck: Natural history, investigations, laser, and surgical management. Otolaryngol Clin N Am. 2018;51:197-211.
- [CrossRef] [PubMed] [Google Scholar]
- The Vanishing Port-Wine stain birthmark-consideration for a rare type of congenital vascular anomaly. Eur J Plast Surg. 2022;45:997-1013.
- [CrossRef] [Google Scholar]
- Reconstruction of head and neck capillary malformations with free perforator flaps for aesthetic purposes. Ann Plast Surg. 2016;77:13-6.
- [CrossRef] [PubMed] [Google Scholar]
- The pathogenesis of Port wine stain and Sturge weber syndrome: Complex interactions between genetic alterations and aberrant MAPK and PI3K activation. Int J Mol Sci. 2019;20:2243.
- [CrossRef] [PubMed] [Google Scholar]
- Basal cell carcinoma arising in port wine stains: Coincidence or correlation? Adv Dermatol Allergol. 2020;37:272-3.
- [CrossRef] [PubMed] [Google Scholar]
- Squamous cell carcinoma on a port wine stain. Actas Dermosifiliogr. 2019;110:e1-2.
- [CrossRef] [Google Scholar]
- Port wine stain treatment outcomes have not improved over the past three decades. J Eur Acad Dermatol Venereol. 2019;33:1369-77.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatment of head and neck port-wine stains by means of a staged zonal approach. Plast Reconstr Surg. 2014;134:1003-12.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatment of dermatomal capillary malformations in the adult face. Arch Plast Surg. 2012;39:126-9.
- [CrossRef] [PubMed] [Google Scholar]
- Prognosis and response to laser treatment of early-onset hypertrophic port-wine stains (PWS) J Am Acad Dermatol. 2016;75:64-8.
- [CrossRef] [PubMed] [Google Scholar]
- Vascular lip enlargement: Part II. Port-wine macrocheilia-tenets of therapy based on normative values. Plast Reconstr Surg. 1997;100:1674-81.
- [CrossRef] [PubMed] [Google Scholar]
- Nodules arising within port-wine stains: A clinicopathologic study of 31 cases. Am J Dermatopathol. 2011;33:144-51.
- [CrossRef] [PubMed] [Google Scholar]
- Correction of facial deformity in Sturge-Weber syndrome. Plast Reconstr Surg Glob Open. 2016;4:e843.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical correction for patients with port-wine stains and facial asymmetry. J Cosmet Dermatol. 2020;19:3307-14.
- [CrossRef] [PubMed] [Google Scholar]







