Translate this page into:
Dermoscopy as a novel tool to examine and assess treatment response of acne scars: A pilot study in an Indian population
*Corresponding author: Shreya Poddar, Department of Dermatology, Asansol District Hospital, Asansol, West Bengal, India. shreyapods@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma R, Khunger N, Poddar S. Dermoscopy as a novel tool to examine and assess treatment response of acne scars: A pilot study in an Indian population. J Cutan Aesthet Surg. doi: 10.25259/jcas_43_23
Abstract
Objectives:
Acne scars are common and have limited methods of evaluation. They occur due to decreased collagen (atrophic, rolling, icepick, boxcar, and linear) or increased collagen (hypertrophic and keloidal). There are very few studies concerning the evaluation and treatment methodology of acne scars by dermoscopy. The primary aim of the study was to observe the dermoscopic features of different types of acne scars. The secondary aim was to evaluate the role of dermoscopy in the assessment of response to treatment.
Material and Methods:
Thirty consenting patients with post-acne scars were enrolled for the study in a tertiary care dermatology center. Detailed history and clinical examination data were recorded followed by dermoscopic evaluation at presentation. Consequently, the standard treatment modality was chosen depending on the type of acne scars, and the procedure was done at monthly intervals. Dermoscopy was repeated at a frequency of 6 months. Concurrently, histopathological evaluation for collagen and elastin was performed in a case of deep atrophic scar.
Result:
Initial dermoscopy showed a poorly defined pseudo reticular network on the face and diffuse pigmentation interrupted by adnexal openings. Ice pick scars appeared as comedo-like openings along with an accentuated perifollicular pigmented network and vascular structures. Rolling scars showed valley-like areas with sloping edges and a marginal rim of pigmentation. Boxcar scars had characteristic cup-shaped depressions with a hyperpigmented rim and dilution of central pigmentation. On sequential dermoscopy following treatment, a decrease in perifollicular pigmentation, and a granular pigment network was seen. There was considerable curtailment of size and depth of acne scars. Further, an increase in the hair follicle density was observed following treatment. Scars of shorter duration showed better response compared to scars of longer duration. In histopathology, increased collagen deposition and early elastogenesis were observed.
Conclusion:
Treatment is more effective in cases of acne scars of shorter duration. Dermoscopy may be a valuable tool in the assessment of acne scars and their response to treatment.
Keywords
Acne scars
Dermoscopy
Histopathology
INTRODUCTION
Acne is a common, chronic inflammatory condition of the pilosebaceous unit. Scarring is a common sequela with prevalence ranging from 1% to 28% in different ethnic groups.1 Acne scars cause profound psychological impact and go well beyond the actual manifestation of the condition as it predominantly involves the face.2 It adversely affects the psychological well-being and emotional quotient, thereby influencing the quality of life. Hence, the earliest treatment of this condition is of paramount importance. Acne scars are common and have limited methods of evaluation. Acne scars occur due to decreased collagen (atrophic, rolling, icepick, boxcar, and linear) or increased collagen (hypertrophic and keloidal). In most cases, the acne scars heal with loss of collagen and in limited cases with accumulation of collagen. There is limited data on dermoscopy of acne scars and very few studies concerning the evaluation and treatment methodology of acne scars by dermoscopy.
There are multiple options for treatment depending on the type of acne scars. Besides, energy-based devices such as non-ablative, ablative laser, and microneedling radiofrequency, there are other treatment modalities available such as subcision, punch excision, and chemical reconstruction of skin scars (CROSSs) with trichloroacetic acid (TCA) technique.3-6 The primary aim of this pilot study was to observe the dermoscopic features in different types of acne scars. The secondary aim was to evaluate the role of dermoscopy in the assessment of response to treatment.
MATERIAL AND METHODS
This was a prospective and two-independent observer-blinded study. We evaluated the dermoscopic characteristics of acne scars. This study was undertaken at a tertiary care hospital, after approval by the Medical Ethics Committee and was conducted between March and August 2018. This study included 30 adult consenting patients; 22 males and 8 females who had not undergone any previous treatment for acne scars. Patients with an age <18 years, a history of active infection on the face, keloidal tendency, bleeding disorders, patients on anticoagulants, or any regional dermatosis were excluded from the study. Due consideration was given to include all types of acne scars in the study. A questionnaire was prepared to collect the data needed for the objectives of the study. Every patient gave consent to participate in the study after being informed about the nature of the treatment and the research. A detailed history of the onset, duration, and previous treatment if taken along with a thorough clinical examination was conducted. Detailed dermoscopic evaluation with Ultracam triple light source (TLS) dermoscope and clinical imaging was done in a representative area, before and after the treatment at intervals of 6 months, in all the patients. Dermoscopic pictures were taken by one of the authors. Two other authors, who were unaware of the type of acne scar independently, evaluated the dermoscopic images for the dermoscopic characteristics of these acne scars. There are a variety of treatments for acne scars. Individual acne scars can vary in type and depth; hence, treatment was chosen depending on the type of individual scar. Different treatment modalities are better suited for a particular acne scar depending on its mode of action. The standard treatment as per the protocol of the study was carried out. Briefly, subcision was done for all atrophic scars.7 This was combined with the CROSS technique using 100% TCA for icepick scars, microneedling using the dermaroller of 1.5 mm size for rolling scars, and punch techniques for boxcar scars.5-8 Fat grafting was done post-excision for boxcar scars. Patients underwent monthly treatment. Assessment of the representative area with dermoscopy was done at presentation and interval of 6 months from the same site. Response to treatment was graded by the quartile grading and Goodman and Baron Qualitative scale.9 Histopathological study was also performed at intervals of 6 months in one case of deep atrophic scarring.
The Statistical Package for the Social Sciences version 21.0 was employed for statistical analysis. Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean ± standard deviation. The number of hair follicles before and after the treatment was compared using a paired t-test. Qualitative variables were compared using the Chi-square test. P < 0.05 was considered statistically significant.
RESULTS
Out of the sample size of 30, a total of 26 patients participated for the entire duration of treatment (6 months), for whom the post-treatment dermoscopy was performed. There were 22 males and 8 females who belonged to the age group of 18–46 years. The most common predominant type of acne scars was ice pick scars (76.92% of the participants), followed by rolling scars (69.23% of the participants) and boxcar scars (61.53% of the participants) [Table 1]. The dermoscopic findings of atrophic scars are summarized in Table 2. The most frequent dermoscopic features of icepick scars were a crater-like depression with accentuation of central hyperpigmentation. Rolling scars showed valley-like areas with sloping edges and a marginal rim of pigmentation, while, in boxcar scars, there were characteristic cup-shaped depressions with a hyperpigmented rim and dilution of central pigmentation [Figure 1a-c]. The clinical and dermoscopic examination of the representative area was marked and performed. The clinical and dermoscopic evaluation of the representative area was performed again after treatment at 6 months [Figure 2].
| Type of scars | Procedure | Number of patients |
|---|---|---|
| Icepick | Subcision+TCA | 20 |
| Rolling | Subcision+CO2 laser/subcision+microneedling | 18 |
| Boxcar | Subcision+Punch Elevation | 16 |
| Hyperpigmented | Salicylic acid+Yellow peel | 6 |
| Linear | Subcision+CROSS | 1 |
| Lipoatrophic | Subcision+Autologous Fat Transplant | 3 |
| Hypertrophic | Intralesional Triamcinolone Injection | 1 |
TCA: Trichloroacetic acid, CROSS: Chemical reconstruction of skin scars, CO2: Carbon dioxide
| Global features | Diminution of a normal pseudo reticular network. Linear hyperpigmented streaks with interrupted hypopigmented areas. Diffuse light brown pigmentation Crinkled appearance in the affected areas. Areas of whitish-to-yellow bands present in between. Cup, valley or crater-like pigmented areas Decrease in hair follicles and opening of sweat glands Few comedones with light to dark brown homogenous areas of pigmentation. Linear blood vessels with few dots. Dots and globules with few regression structures seen. |
| Icepick scars | Crater like depression present with accentuation of central hyperpigmentation (in comparison to periphery) |
| Rolling scars | Valley like pigmented areas with marginal rim of pigmentation present |
| Boxcar scars | Cup shaped depression with hyperpigmented rim and central dilution in pigmentation |
| Linear scars | Light brown homogenous areas of diffuse pigmentation and areas of white to yellow band present |
| Lipoatrophic scars | Linear hyperpigmented streaks with interrupted hypopigmented areas Crinkled appearance in the affected area |
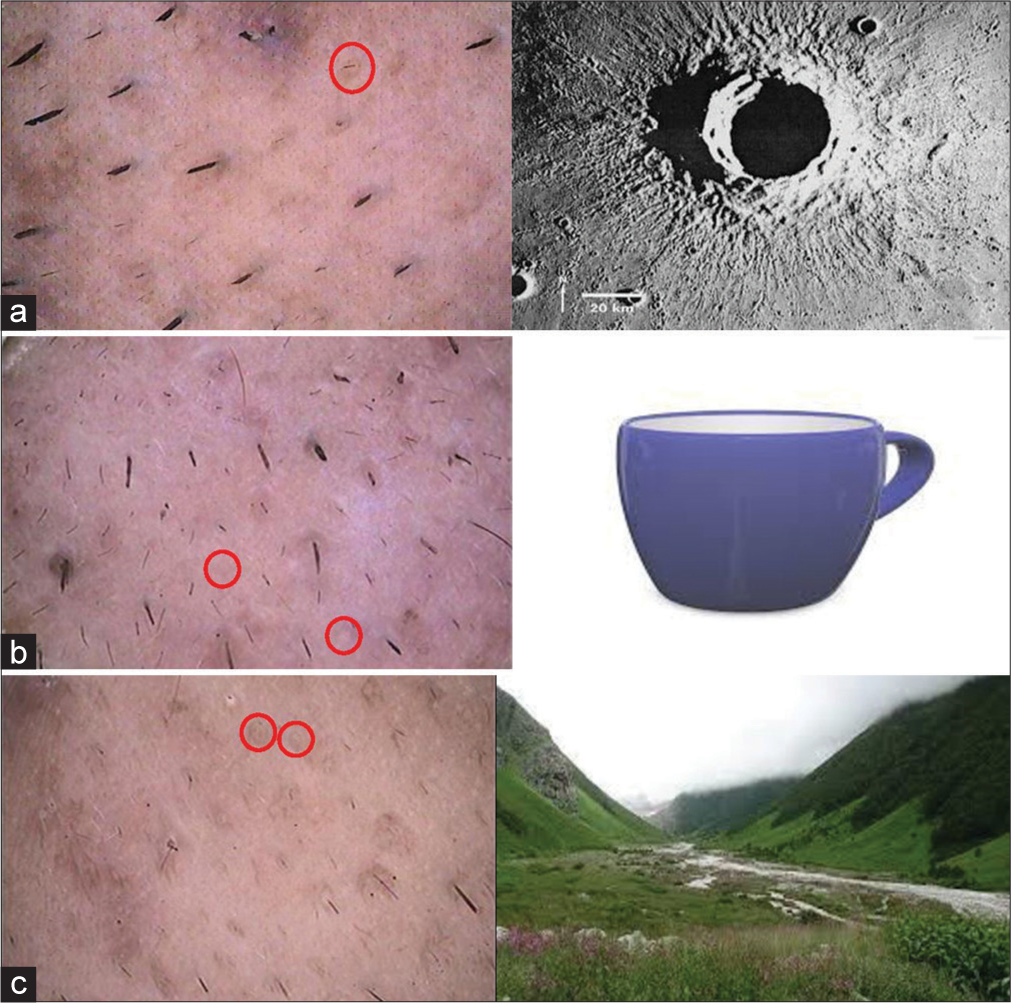
- Dermoscopic assessment of acne scars (Ultracam TLS dermoscope). (a) Ice pick scars: Comedo-like openings with accentuated perifollicular pigmented network and vascular structures (red circle). (b) Boxcar scars: Cup-shaped depressions with a hyperpigmented rim and dilution of central pigmentation (red circle). (c) Rolling scars: Valley-like areas with sloping edges and a marginal rim of pigmentation (red circle).
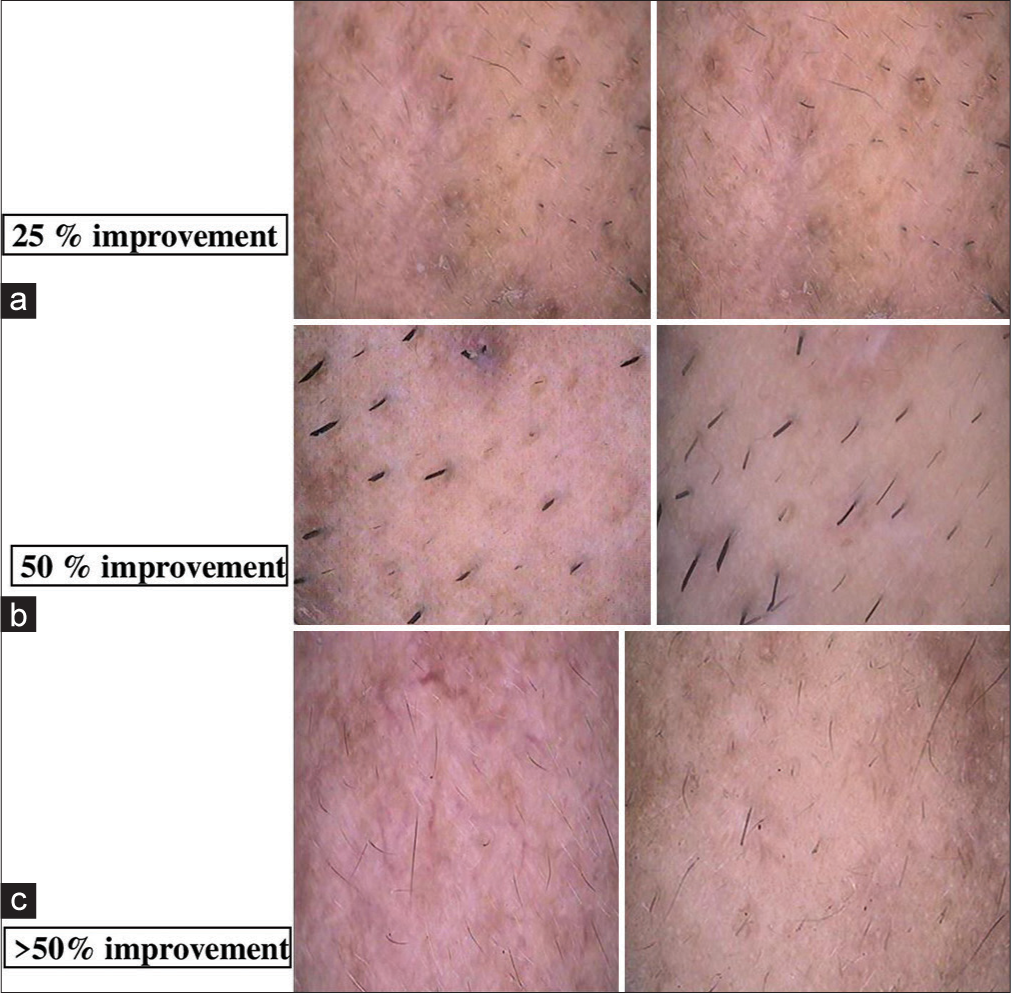
- Independent observer-based evaluation after intervention: (a) 25% improvement, (b) 50% improvement, and (c) >50% improvement.
The clinical and dermoscopic improvement in the study was graded on the following improvement scale:
Grade 1: <25% improvement
Grade 2: 25–50% improvement
Grade 3: >50% improvement.
The evaluation of the improvement was assessed by two independent observers depending on:
Diffuse pigmentation
Perifollicular pigmentation
Size, depth, and margin of the scars
Number of hair follicles.
Any one of the four subclassified criteria mentioned above was considered positive [Figure 2].
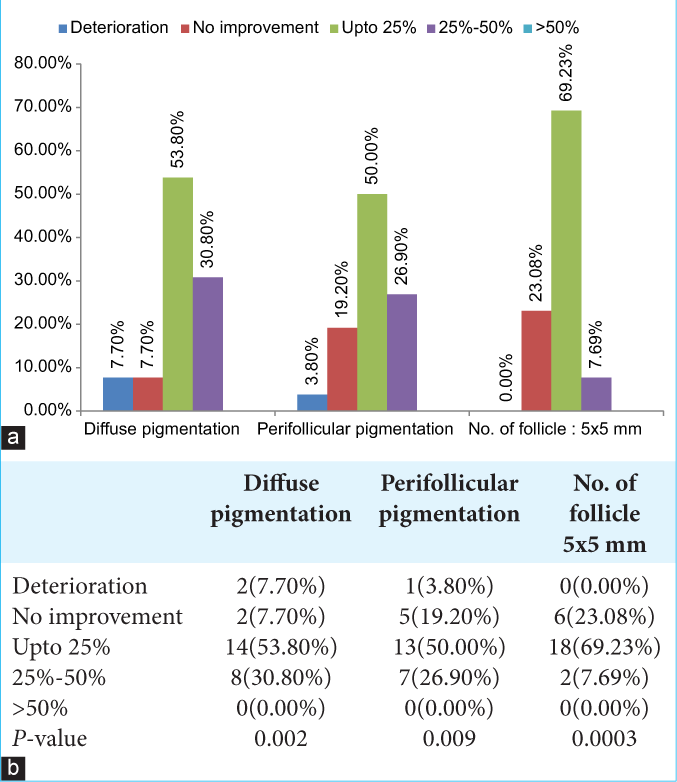
The histopathological evaluation manifested increased collagen deposit and early elastogenesis [Figure 3]. The duration of acne scars ranged from 1 to 10 years. A significant association between improvement and duration of acne scars was found. Patients with acne scars of duration ranging from 2 to 5 years manifested grade 3 improvement, <10 years manifested grade 2 improvement, and more than 10 years duration showed grade 1 improvement. The patient with a lesser duration of acne scar showed more significant improvement, P = 0.019 [Table 3]. There was a considerable decrease in diffuse and perifollicular pigmentation and an increase in hair follicles was observed dermoscopically [Figure 2], following the treatment [Table 4 a and b]. The grade 1 improvement of diffuse pigmentation was noted in 53.8% of the cases, perifollicular pigmentation was improved in 50% of the cases, and an increase in the hair follicles was noted in 69.23% of the cases. The treatment was well tolerated with transient side effects such as mild erythema and post-inflammatory hyperpigmentation.
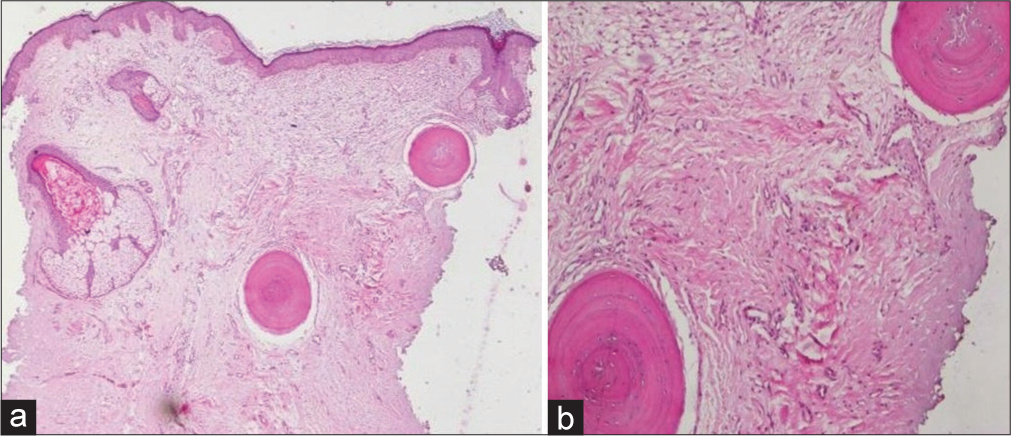
- Histopathological evaluation done at interval of 6 months a)Increased collagen deposition (H&E, X40) b)Early elastogenesis noted (H&E, X100). H&E: Hematoxylin and Eosin.
| Duration of acne scar | Grade 1 improvement | Grade 2 improvement | Grade 3 improvement | No improvement | Deterioration | Total |
|---|---|---|---|---|---|---|
| 1–2 years | 0 | 2 | 0 | 0 | 0 | 2 |
| 2–5 years | 10 | 7 | 1 | 0 | 0 | 18 |
| 5–10 years | 0 | 1 | 0 | 2 | 1 | 4 |
| More than others | 2 | 0 | 0 | 0 | 0 | 2 |
| Total | 12 | 10 | 1 | 2 | 1 | 26 |
 |
DISCUSSION
Acne scars are classified into two types – atrophic and hypertrophic. Atrophic scars comprise icepicks, boxcars, and rolling scars.8 Hypertrophied scars are classified as keloidal and hypertrophic scars.9
Traditionally, evaluation of an acne scar has been carried out by physical examination, examining the presence of erythema, depth of scarring, and baseline skin phototypes.10 Dermoscopy is a unique technique of magnification commonly employed for the visualization of sub-surface structures.11
There is a paucity of data on dermoscopic findings in acne scars. Various clinical and dermoscopic features of atrophic acne scars noted in our study were noted [Table 2]. The post-treatment clinical findings and various dermoscopic features accounted as improvement were as follows: Diffuse pigmentation, perifollicular pigmentation, detailed findings around the margins of the acne scar, and number of hair follicles [Figure 2]. The improvement in our study was graded in the improvement scale as grade 1–grade 3 depending on the percentage of improvement. We observed a significant reduction in the pigmentation of acne scars and an increase in the hair follicle following the treatment, based on clinical and dermoscopy findings [Figure 2]. In our study, the shorter duration of acne scars exhibited a better response to treatment.
The histopathological study of the acne scar showed a remarkable increase in collagen post-treatment. There is very scarce data for dermoscopic evaluation of acne scars and it is assessment post-treatment. A Korean study did a dermoscopic assessed of atrophic acne scar patients. They depicted the role of dermoscopy in acne scars with a significant increase in the density of hair follicles post-treatment which was quite similar to our study.7 Dermoscopic findings in their study showed no obvious differences according to clinical acne scar type.
CONCLUSION
Dermoscope is an important handheld tool to assess treatment response in acne scars. Multiple treatment combinations are preferred in acne scars and show better response clinically and dermoscopically. A dermoscope can be used as an added important evaluation tool to assess and monitor treatment response in acne scars. It also aids in patient counseling. The important dermoscopic features were noted at the interval of 6 months which showed a decrease in perifollicular pigmentation, granular pigment network with substantial diminution of depth and margin of acne scars, and an increase in the hair follicle density. None of the treatment methodologies currently in vogue may cure the acne scar in total. The best way remains prevention and early initiation of treatment as better treatment outcome was noticed in acne scars of shorter duration.
Further studies are required to establish the role of dermoscopy in acne scars with a bigger sample size.
Authors’ contributions
All the authors have contributed to concepts, design, definition of intellectual content, literature search, clinical studies, data acquisition, data analysis, statistical analysis, manuscript preparation, manuscript editing and manuscript review.
Ethical approval
The study complies with the Helsinki Declaration of 1964.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Niti Khunger is on the Editorial Board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Comparison of the epidemiology of acne vulgaris among Caucasian, Asian, Continental Indian and African American women. J Eur Acad Dermatol Venereol. 2011;25:1054-60.
- [CrossRef] [PubMed] [Google Scholar]
- A clinical evaluation of acne scarring and its incidence. Clin Exp Dermatol. 1994;19:303-8.
- [CrossRef] [PubMed] [Google Scholar]
- Subcutaneous incisionless (subcision) surgery for the correction of depressed scars and wrinkles. Dermatol Surg. 1995;21:543-9.
- [CrossRef] [PubMed] [Google Scholar]
- Dermabrasion and microdermabrasion. Facial Plast Surg. 2009;25:301-10.
- [CrossRef] [PubMed] [Google Scholar]
- The consideration of dermoscopic findings during atrophic acne scar treatment: A pilot study. Korean J Dermatol. 2015;53:23-9.
- [Google Scholar]
- Acne scarring: A classification system and review of treatment options. J Am Acad Dermatol. 2001;45:109-17.
- [CrossRef] [PubMed] [Google Scholar]
- Acne scars: Pathogenesis, classification and treatment. Dermatol Res Pract. 2010;2010:893080.
- [CrossRef] [PubMed] [Google Scholar]
- Acne scarring-pathogenesis, evaluation, and treatment options. J Clin Aesthet Dermatol. 2017;10:12-23.
- [Google Scholar]







