Translate this page into:
Familial multiple glomuvenous malformations: The role of 1064-nm neodymium-doped yttrium aluminum garnet laser
*Corresponding author: Cláudia Brazão, Department of Dermatology, Unidade Local de Saúde Santa Maria, Avenida Professor Egas Moniz, Lisbon-1649-035, Portugal. claudiabrazaomd@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Brazão C, Sun L, de Sousa D, Correia-Fonseca I, Filipe P. Familial multiple glomuvenous malformations: The role of 1064-nm neodymium-doped yttrium aluminum garnet laser. J Cutan Aesthet Surg. doi: 10.25259/JCAS_54_2024
Dear Editor,
Glomuvenous malformations (GVMs) are cutaneous hamartomas of venous vessels and glomus cells with autosomal dominant inheritance.1 GVM does not pose a health risk and has no malignant transformation. However, they can be painful or disfiguring, and treatment may be necessary.2,3 We present a case of successful treatment of GVM with a 1064-nm neodymium-doped yttrium aluminum garnet (Nd:YAG) laser.
A 12-year-old boy, Fitzpatrick’s phototype III, was referred to dermatologic evaluation due to numerous cutaneous bluish papules that progressively appeared after birth. He was the firstborn of non-consanguineous parents, and the family history was relevant for one similar lesion on his father’s arm. Physical examination revealed bluish-to-violaceous, non-tender papules and nodules on the scapular [Figure 1a], axillary regions, and both legs. The skin biopsy demonstrated vascular channels surrounded by glomus cells in the dermis and hypodermis, compatible with GVM [Figure 1b]. Genetic analyses identified the Glomulin gene heterozygous variant (c.1319G>A)-p. (Trp440*) (Protein change) [p. refers to the change at the protein level; Trp is the one-letter code for tryptophan (W), which is the amino acid originally at position 440 of the protein.;* indicates a stop codon] on the patient and his father, establishing the diagnosis of familial multiple GVM. On discussion of the therapeutic options, we decided on laser treatment. We started to treat the scapular GVM using 1064-nm Nd:YAG laser with continuous forced-air-cooling (Cynergy-Multiplex®/Cynosure®) under topical anesthesia (lidocaine/prilocaine 25 mg/g). The laser parameters were chosen according to the literature and the manufacturer’s recommendations.3-5 Accordingly, we used a 3-mm spot size and 40-ms intervals, but a lower fluence of 120 J/cm2, later increased to 180 J/cm2. After five sessions with 2-month intervals, complete resolution was achieved [Figure 2]. As side effects, the patient reported moderate pain during the procedure. There were no complications or recurrences after 1 year of follow-up. After confirming the efficacy and safety of this treatment, we proceeded to treat the remaining GVM.
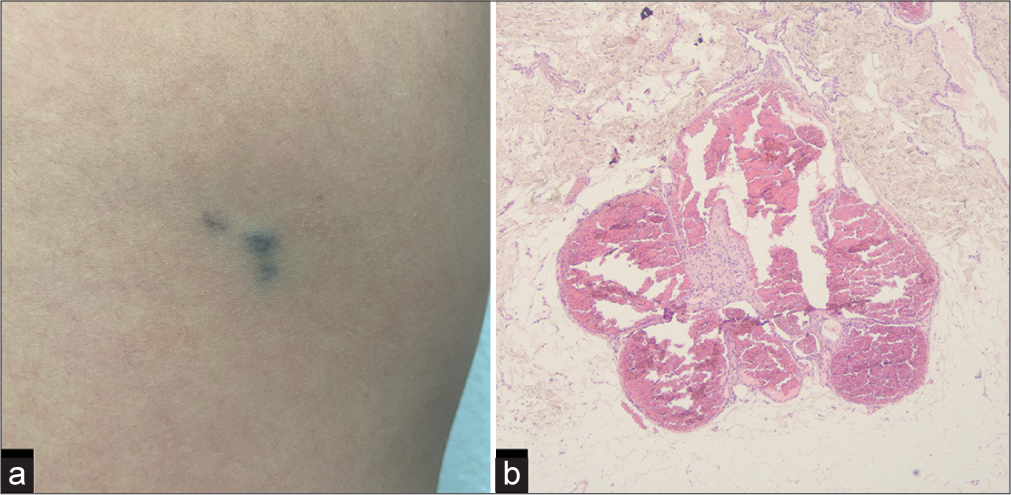
- Glomuvenous malformation. (a) Clinical image: Cluster of bluish-to-violaceous, firm, non-compressible, non-tender papules, and nodules, located on the patient’s right scapular region. (b) Histopathologic findings: Large, dilated, blood-filled vascular channels located in the transition between the dermis and hypodermis (dermo-hypodermal junction), which are lined by endothelial cells and layers of cuboidal cells with uniform round to ovoid nuclei (glomus cells) in a hyalinized stroma (hematoxylin and eosin, ×40).

- Clinical image after treatment: Complete resolution of the glomuvenous malformation on the right scapular region, after 5 sessions of 1064-nm neodymium-doped yttrium aluminum garnet laser treatment.
The treatment of GVM is challenging and must be evaluated on a case-by-case basis.2,5 Different therapeutic modalities are available: Surgery, sclerotherapy, and laser therapy.2 Although surgical resection has been the primary treatment, it is often impractical due to the size and number of lesions. Sclerotherapy and carbon dioxide laser are effective, but necrosis and ulceration are frequent adverse effects. Pulsed-dye laser has limited effect.3,4 Previous reports demonstrate the higher efficacy of 1064-nm Nd:YAG laser.3-5 As GVM is located within the lower dermis and superficial hypodermis, this laser is more effective in reaching the chromophores and delivering thermal ablation.5 The laser parameters and number of treatment sessions depend on the lesion type, body site, patient’s age, and laser surgeon’s experience.5 The reported parameters include spot sizes of 3–10 mm, intervals of 10–50 ms, and fluences of 50–240 J/cm2. Unlike shorter-wavelength lasers, small upward adjustments influence this laser can result in ulceration, scarring, and dyspigmentation. Therefore, some authors recommend starting with lower fluences, especially in children, which can be escalated depending on response until optimal parameters are identified.5 The narrow therapeutic window of Nd:YAG laser warrants careful parameter optimization, but when correctly performed, it has demonstrated substantial efficacy with minimal complications.3-5
Although guidelines are warranted to establish protocols for managing these patients, our case corroborates the efficacy and safety of the 1064-nm Nd:YAG laser for multiple GVM, and, taking into account the existing literature, we propose its consideration as a first-line treatment.
Authors’ contributions
All authors contributed to the manuscript conception and design, material preparation, literature research, and analysis. All authors contributed to preparing, drafting and writing this manuscript, and to its critical appraisal, and have seen and approved the final version for submission and publication.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Surgical and non-surgical treatment modalities for glomuvenous malformations. Dermatol Online J. 2021;27
- [CrossRef] [Google Scholar]
- Successful treatment of hereditary multiple glomangiomas with Nd:YAG laser. J Eur Acad Dermatol Venereol. 2014;28:1123-5.
- [CrossRef] [PubMed] [Google Scholar]
- Nd:YAG laser treatment for multiple cutaneous glomangiomas: Report of 3 cases. Arch Dermatol. 2011;147:255-6.
- [CrossRef] [PubMed] [Google Scholar]
- Utility and tolerability of the long-pulsed 1064-nm neodymium: yttrium-aluminum-garnet (LP Nd:YAG) laser for treatment of symptomatic or disfiguring vascular malformations in children and adolescents. J Am Acad Dermatol. 2017;77:473-9.
- [CrossRef] [PubMed] [Google Scholar]






