Translate this page into:
Efficacy and safety of Q-switched neodymium-doped yttrium aluminum garnet (532 nm) in freckles in skin of color patients
*Corresponding author: Rashmi Sarkar, Department of Dermatology, Lady Hardinge Medical College and Associated Hospitals, New Delhi, India. rashmisarkar@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sarkar R, Mendiratta V, Sonker S, Dua A, Verma B. Efficacy and safety of Q-switched neodymium-doped yttrium aluminum garnet (532 nm) in freckles in skin of color patients. J Cutan Aesthet Surg. doi: 10.25259/JCAS_29_2024
Abstract
Objectives
The study aims to determine the efficacy of Q-switched neodymium-doped yttrium aluminum garnet (Nd:YAG) laser using physician and patient self-assessment and study the safety profile of Q-switched Nd:YAG for treatment of freckles in patients of the skin of color.
Material and Methods
A hospital-based prospective interventional study was conducted at a tertiary care center. A total of 40 subjects above 18 years of age with a minimum of 5 lesions on each side of the face were recruited and divided into two groups. All of them had IV and V Fitzpatrick skin types. In group A, only sunscreen was used as a control and in group B, a 532 nm Q-switched Nd:YAG laser was done along with the sunscreen (group B) application. The effectiveness was assessed using a photographic record by physician global assessment scale and by patient self-assessment. Side effects were classified as mild, moderate, and severe. Statistical analysis included Wilcoxon–Mann–Whitney test.
Results
Physician and patient assessment results concluded that statistically significant improvement (P < 0.05) was reported in group B as compared to group A. In group B, 6 cases (30%) had mild side effects such as erythema, burning, and stinging that resolved within 3 days post-procedure. Three (15%) cases developed post-inflammatory hyperpigmentation. No patient developed scarring.
Conclusion
We hereby conclude that Q-switched Nd:YAG laser is an efficacious and safe modality in the treatment of freckles, along with the judicious use of sunscreen.
Keywords
Q-switched Nd:YAG laser
Freckles
Ephelides
INTRODUCTION
Freckles or ephelides are commonly encountered in benign melanocytic proliferation. They are an early sign of photoaging, which imparts substantial esthetic morbidity and also creates psychosocial concern among the patients.
Freckles clinically manifest as small (up to 5 mm), poorly marginated pale brown macules present on sun-exposed skin areas.1 They usually appear in childhood and increase with age. Sun exposure results in aggravation, and their color and density increase in the summer months and fade away in winter.1 Genetic predisposition is often seen.2
Photoprotection is crucial in the treatment and prevention of freckles. Several therapeutic lines exist for freckles with varied response rates and complications. Recent advancements in treatment with lasers have become increasingly popular. Continuous lasers or quasi-continuous lasers have an increased risk of scar formation, hypo, and hyperpigmentation.3 To overcome these problems, a dual-frequency (532/1064 nm) Q-switched neodymium-doped yttrium aluminum garnet (Nd:YAG) laser was developed, which induces both photothermal and photomechanical reactions.4
Melanosomes have a broad absorption spectrum (400–1100); thus, lasers with these wavelengths can be effectively used to treat pigmentary lesions.5 The various lasers tried in the treatment of freckles include 532 nm Q-switched Nd:YAG,2,5 Q-switched alexandrite,6 755 nm long pulse (LP) alexandrite,7 532 nm LP potassium titanyl phosphate (KTP) laser,7 595 nm LP pulsed dye laser,7 and fractional CO2 laser8 with variable efficacy and side effects in Indian skin.
Several studies have been conducted assessing the efficacy and safety of different lasers in the treatment of freckles. To the best of our knowledge, there are no comparative studies done so far evaluating the efficacy, safety, and long-term maintenance of treatment response of Q-switched Nd:YAG laser with topical sunscreen versus only topical sunscreen in the patients of freckles. Hence, our study aims to investigate the therapeutic response of Q-switched Nd:YAG laser and topical sunscreen in patients with freckles of skin color.
MATERIAL AND METHODS
A hospital-based prospective interventional study was conducted from October 2021 to October 2022 in the Department of Dermatology and Sexually Transmitted Disease at Lady Hardinge Medical College and Smt. Sucheta Kriplani Hospital. The Institutional Ethics Committee approved the study.
A total of 40 subjects above 18 years of age with a clinical diagnosis of freckles with a minimum of 5 lesions on each side of the face were recruited. To differentiate the freckles from lentigines, the following points were considered:8
A family history of similar lesions is seen in freckles
Onset of lesions – usually freckles appear early in life compared to lentigines
Freckles usually lighten in winter; on the other hand, lentigines remain the same irrespective of weather
Borders – irregular borders in the case of freckles and lentigines have regular borders.
Half of the patients (i.e., 20) were recruited for sunscreen application (group A), and half of the patients (i.e., 20) for Q-switched Nd:YAG laser (group B) with sunscreens. Patients with a history of keloid scarring, photosensitivity or taking photosensitizing medication, connective tissue disease, history of concurrent vitiligo, active dermatitis at the site of treatment, systemic use of skin lightening agent like tranexamic acid, isotretinoin, photosensitizing medications, or corticosteroids in the past 6 months, topical use of skin lightening agents and corticosteroids in the past 1 month, pregnant or lactating females, and previous history or concurrent skin cancers were excluded from the study. Written informed consent was obtained from the subjects before enrollment. Detailed history and clinical examination were done and recorded on a pre-designed clinical pro forma. Pre and post-treatment photographs were recorded at each visit.
Subjects in both groups were asked to apply 3 mL broad spectrum sunscreen sun protecting factor [(SPF) 30+] to the whole face daily thrice a day at 3 hourly intervals during the day-time. Sunscreen helps both in limiting the progression and preventing new lesions from appearing.
Subjects in group B were treated with 2 sessions of Q-switched Nd:YAG laser (Model [1064QCCL] at a monthly interval, manufactured by M/S Beijing Honkon Tech Co., Ltd, China) with the setting of 532 nm wavelength, at energy 0.10 J, fluence of 1.41 J/cm2, spot size 3 mm, and frequency 4 Hz at a 4-week interval. The area to be treated was marked, topical anesthesia (prilocaine 2.5% + lidocaine 2.5%) was applied under occlusion for 1 h before treatment, and degreasing of the skin with 75% alcohol was done. All individuals in the treatment room used protective eye gear. The endpoint of laser treatment was the development of an immediate ash white color. Post laser ice pack was applied for 20–30 min on the treated area to reduce erythema. Post-laser session patients were advised to apply a combination of 2% fusidic acid + 1% hydrocortisone till the eschar drops off spontaneously. Regular use of sunscreen with SPF 30 + was advised after treatment and to avoid excess sun exposure for 1 week following treatment.
For assessing efficacy, pre-treatment photographs of subjects in group A were compared with photographs after 3 months of treatment, and in group B, they were compared at 1-month post-second treatment session. Photographs were reviewed by 2 independent dermatologists who were blinded to the study and were using the physician global assessment scale independently and rated the clinical improvement (% disappearance of pigments) as grade 0 – no improvement, grade 1 (1–25%), grade 2 (26–50%), grade 3 (51–75%), and grade 4 (76–100%).8 Subjective patient’s assessment was done depending on similar grading. More than 50% improvement (grade 3 and grade 4) was considered a significant improvement.9
Side effects were classified as mild, moderate, and severe: Mild – erythema, burning, stinging; moderate – post-inflammatory hypo/hyperpigmentation; severe – scarring. All subjects of both groups were reviewed after 2 months for recurrence of lesions. Any patient developing immediate or late side effects was managed according to the standard institutional treatment protocol.
RESULTS
Mean age of cases in both the groups was almost similar, i.e., 30.35 years and 28.45 years, respectively, and the most commonly affected site was cheeks in both groups [Table 1]. Out of all patients, 36 (90%) cases had a positive family history of freckles. Based on physician assessment done using the physician global assessment scale [Table 2], in group B, out of 20 cases, 12 patients (60%) showed significant improvement (51–100%) and only 1 case (5%) showed no improvement (grade 0) [Figures 1 and 2]. Whereas in group A, the majority of cases (10 [50%]) showed no improvement (grade 0) and only 2 (10%) patients showed significant improvement [Figures 3 and 4]. Based on subjective patient assessment [Table 2], in group B, 11 (55%) cases showed more than 50% improvement, while only 2 cases (10%) showed no improvement (grade 0). In group A, 35% of the cases showed grade 0 (no improvement) and only 3 (15%) cases showed more than 50% improvement. Physician and patient assessment results concluded that statistically significant improvement (P < 0.05) was reported in group B as compared to group A. Pre and post-treatment photographs of both subjects of Group A and Group B are shown in Figures 1 and 2, respectively.
| Demographic characteristics | Sunscreen (n=20) (%) | Laser (n=20) (%) | P-value |
|---|---|---|---|
| Age (years) | 30.35±9.42 | 28.45±4.1 | 0.416† |
| Duration (months) | 6 (4–15) | 12 (2–39) | 0.531‡ |
| Gender | |||
| Female | 18 (90) | 19 (95) | 1* |
| Male | 2 (10) | 1 (5) | |
| Forehead | 1 (5) | 2 (10) | 1* |
| Cheeks | 20 (100) | 20 (100) | NA |
| Chin | 3 (15) | 5 (25) | 0.695* |
| Systemic disease | 4 (20) | 0 (0) | 0.106* |
| Keloidal tendency | 0 (0) | 1 (5) | 1* |
| No dermatology disease | 13 (65) | 18 (90) | 0.127* |
| Acne | 4 (20) | 1 (5) | 0.342* |
| Melasma | 3 (15) | 1 (5) | 0.605* |
| Scars | 1 (5) | 0 (0) | 1* |
| History of previous treatment (topical/systemic/hormonal/surgical/laser) | 0 (0) | 0 (0) | NA |
| Family history | 1 (5) | 4 (20) | 0.342* |
| History of photosensitivity | 0 (0) | 0 (0) | NA |
| History of CTD | 0 (0) | 0 (0) | NA |
| History of isotretinoin intake | 0 (0) | 1 (5) | 1* |
| Skin resurfacing procedures | 1 (5) | 0 (0) | 1* |
| Filler injection | 0 (0) | 0 (0) | NA |
| Efficacy | Sunscreen (n=20) (%) | Laser (n=20) (%) | P-value |
|---|---|---|---|
| Physician assessment | |||
| Grade 0 (No improvement) | 10 (50) | 1 (5) | 0.0009* |
| Grade 1 (1–25%) | 6 (30) | 3 (15) | |
| Grade 2 (26–50%) | 2 (10) | 4 (20) | |
| Grade 3 (51–75%) | 2 (10) | 6 (30) | |
| Grade 4 (76–100%) | 0 (0) | 6 (30) | |
| Subjective patient assessment | |||
| Grade 0 (No improvement) | 7 (35) | 2 (10) | 0.019* |
| Grade 1 (1–25%) | 7 (35) | 2 (10) | |
| Grade 2 (26–50%) | 3 (15) | 5 (25) | |
| Grade 3 (51–75%) | 3 (15) | 7 (35) | |
| Grade 4 (76–100%) | 0 (0) | 4 (20) | |

- (a) Global photographs of patient 1 at baseline in group B, (b) global photographs of patient 1 at 2 months in group B.
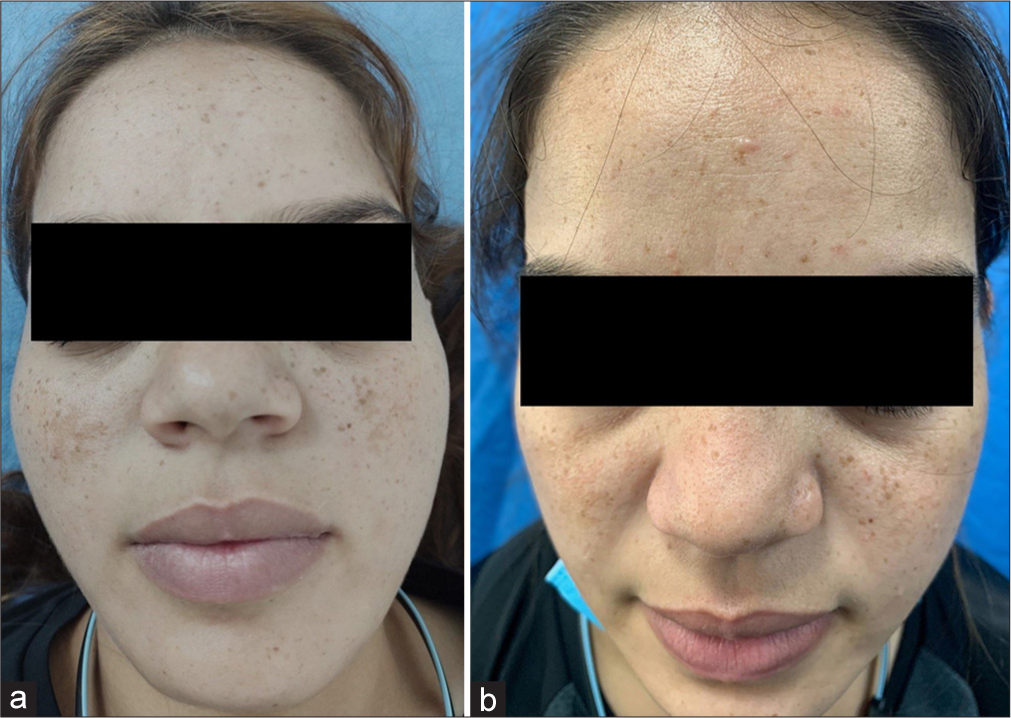
- (a) Global photographs of patient 2 at baseline in group B, (b) global photographs of patient 2 at 2 months in group B.
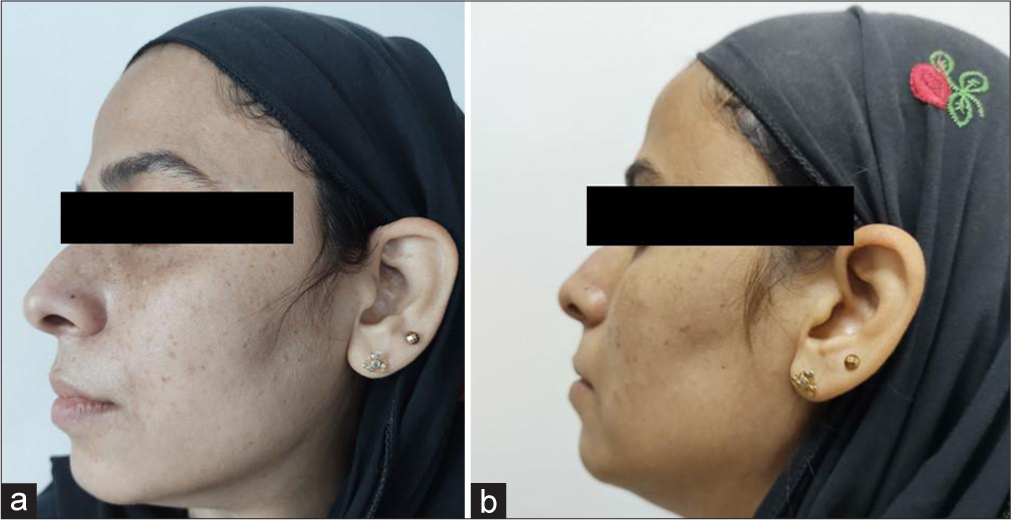
- (a) Global photographs of patient 3 at baseline in group A, (b) global photographs of patient 3 at 2 months in group A.
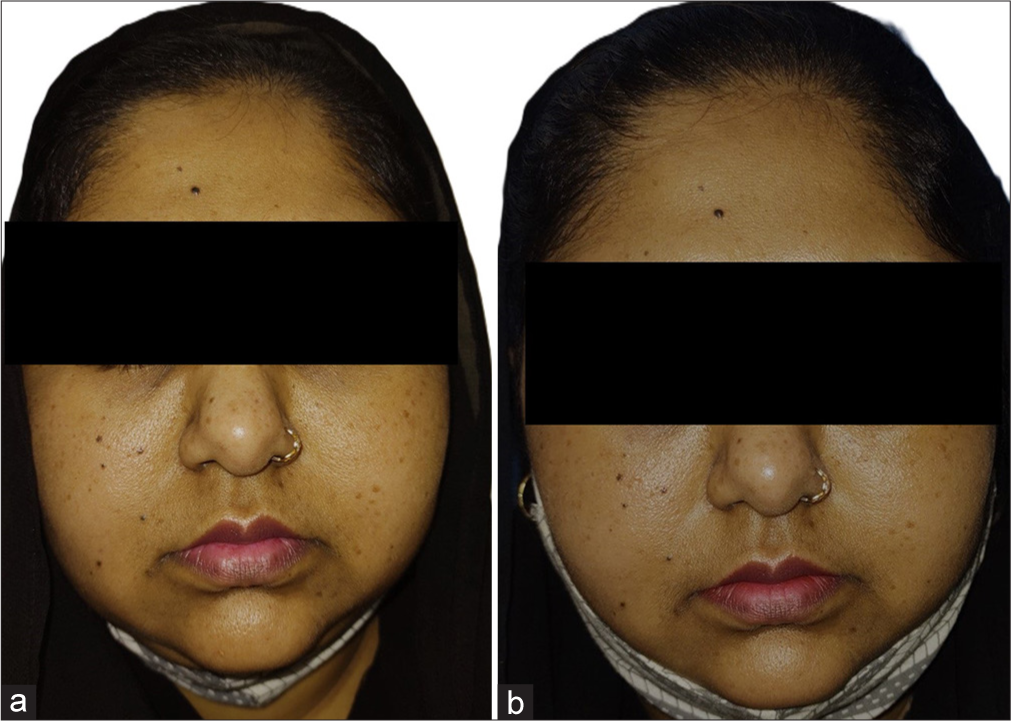
- (a) Global photographs of patient 4 at baseline in group A, (b) global photographs of patient 4 at 2 months in group A.
The majority of cases (11 [55%]) in group B experienced no adverse effects, while 6 cases (30%) had mild side effects such as erythema, burning, and stinging that resolved within 3 days post-procedure [Table 3]. Three (15%) cases developed post-inflammatory hyperpigmentation that improved with the regular use of sunscreen and skin-lightening creams. None developed severe side effects such as scarring, which suggests that Q-switched Nd:YAG is reasonably safe. However, in group A, the majority of cases (19 [95%]) had no side effects, and 5 % of cases had mild side effects.
| Side effects | Sunscreen (n=20) (%) | Laser (n=20) (%) | P-value |
|---|---|---|---|
| No | 19 (95) | 11 (55) | 0.014* |
| Mild | 1 (5) | 6 (30) | |
| Moderate | 0 (0) | 3 (15) | |
| Total | 20 (100) | 20 (100) |
DISCUSSION
Freckles are hyperpigmented lesions induced by sun exposure and present mostly over photo-exposed sites. These are of profound cosmetic concern and lower self-esteem among patients. Photoprotection remains the mainstay of treatment and also prevents the development of new lesions. Several therapeutic lines exist for freckles with varied response rates and complications, including physical therapies such as cryotherapy, laser therapy, chemical peels trichloroacetic acid [(TCA) peels,10 glycolic acid,11 and Jessner’s solution4], and dermabrasion. Topical therapies include hydroquinone, tretinoin, adapalene, and their combinations or camouflage.4
The absorption spectrum of melanin is very broad, i.e., 400– 1100 nm.5 Since many laser systems function in this visible and infrared range, all these lasers would have some effect on melanin. Green, red, and infrared wavelength bands are most useful for treating pigmented lesions.12 In the past decade, Q-switched lasers have been developed (Q-switched ruby, Q-switched alexandrite, Q-switched Nd:YAG) to minimize damage to surrounding skin by continuous wave lasers.5 Continuous lasers or quasi-continuous lasers have an increased risk of scar formation, hypo, and hyperpigmentation.3 To overcome these problems, a dual-frequency (532/1064 nm) Q-switched Nd:YAG laser was developed, which induces both photothermal and photomechanical reactions.5 It causes selective photothermolysis of melanosomes and melanin by producing higher temperature (1000°C) with short pulse duration (3–7 ns), resulting in evaporation of melanin within the skin and vacuolization. Between the target and surrounding tissue, a collapse of the temperature gradient is created, which leads to photomechanical damage resulting in fragmentation of the target.4 It can remove the pigmented lesion without damaging the surrounding tissue, with the scab falling off by the 7th day of treatment.2
Green laser light (532 nm Q-switched Nd:YAG) is particularly effective on freckles as shorter wavelengths are more strongly picked up by the melanin in the freckles.2
Pai and Pai2 recruited 43 patients with freckles with skin type V and they underwent Q-switched Nd:YAG (532 nm) laser treatment. Out of 43 patients, 23 (53.48%) patients showed significant improvement after laser treatment, comparable to our study in which 55% of patients showed improvement. They had reported adverse effects in 20 patients, 7 (16.27%) patients developed hyperpigmentation, and 13 (30.23%) patients developed prolonged hypopigmentation at the treated site.2 While in our study, 6 (30%) patients developed mild erythema, burning, and stinging post-procedure and 3 (15%) patients developed post-inflammatory hyperpigmentation.
In a 24-month follow-up study performed by Rashid et al.,13 Nd:YAG (532 nm) laser therapy was used for treating freckles and lentigines. It was seen that 80% of patients manifested more than 50% improvement. At follow-up, 40% of patients with freckles showed partial recurrence and no patients with lentigines showed recurrence. However, in our study, no patient with significant improvement showed recurrence of freckles within a 2-month long follow-up period post-treatment.
Similar to our study, Q-switched Nd:YAG laser (532 nm) was used in the treatment of various superficial pigmented lesions in Korean patients in a study conducted by Suh et al.14 All four patients treated for freckles showed excellent or good response with one or two sessions of Q-switched Nd:YAG treatment.
In a retrospective analysis of the management of freckles and lentigines, the effectiveness and safety of four different pigment lasers – 595 nm long pulsed dye laser (LPDL), 755 nm LP alexandrite laser, 532 nm Q-switched Nd:YAG, and 532 nm LP KTP laser – were determined.7 Statistically significant improvement was found after treatment with LPDL, Q-switched Nd:YAG, and LP KTP, while no significant improvement was found after LP alexandrite laser. Post inflammatory hyper-pigmentation (PIH) was seen in 20% with LP alexandrite, 10% with Q-switched Nd:YAG, and absent after LPDL and LP KTP.
In an Egyptian study,15 Q-switched Nd:YAG laser was used in the treatment of pigmentary disorders. A total of 25 patients with epidermal lesions were recruited, out of which 10 patients had freckles. They were treated with 532 nm Q-switched Nd:YAG laser and all the patients with freckles showed excellent response. Post-treatment erythema was the most common complication noted in 5 patients (14.71%), followed by post-inflammatory hyperpigmentation in two patients (5.88%). The results were similar to our study, where 6 (30%) patients developed mild erythema, burning, and stinging and 3 patients (15%) developed post-inflammatory hyperpigmentation post-laser treatment.
CONCLUSION
Q-switched Nd:YAG (532) laser is an efficacious and safe modality for the treatment of freckles, along with the rigorous use of sunscreen. Although photoprotection plays an important role in the prevention of freckles, it alone is not sufficient for treatment purposes.
Authors’ contributions
All authors Rashmi Sarkar, Vibhu Mendiratta, Sneha Sonker, Aishwarya Dua, Bharati Verma have contributed substantially in concept, methods, writing and critically approving manuscript.
Ethical approval
The research/study was approved by the Institutional Review Board at Lady Hardinge Medical College and Associated Hospitals, number LHMC/IEC/2022/03/45, dated April 22, 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Novel Preventive and Therapeutic strategies for ephelides (freckles) from a persian medicine perspective: A narrative review. J Skin Stem Cell. 2022;9:e123335.
- [CrossRef] [Google Scholar]
- Q-switched laser treatment for freckles in individuals with skin type V. Aesthet Dermatol Surg. 2017;1:2-7.
- [CrossRef] [Google Scholar]
- Laser treatment of pigmented lesions--2000: How far have we gone? Arch Dermatol. 2000;136:915-21.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of solar lentigines. J Am Acad Dermatol. 2006;54:S262-71.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical applications of Q-switched NdYAG laser. Indian J Dermatol Venereol Leprol. 2008;74:682-6.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of Q-switched and long-pulsed alexandrite laser for the treatment of freckles and lentigines in oriental patients. Lasers Surg Med. 2011;43:108-13.
- [CrossRef] [PubMed] [Google Scholar]
- A retrospective analysis of the management of freckles and lentigines using four different pigment lasers on Asian skin. J Cosmet Laser Ther. 2012;14:74-80.
- [CrossRef] [PubMed] [Google Scholar]
- Sun-induced freckling: Ephelides and solar lentigines. Pigment Cell Melanoma Res. 2014;27:339-0.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of fractional carbon dioxide laser for treatment of unwanted facial freckles in phototypes II-IV: A pilot study. Lasers Med Sci. 2014;29:1937-42.
- [CrossRef] [PubMed] [Google Scholar]
- Trichloroacetic acid peels revisited. J Dermatol Surg Oncol. 1989;15:933-40.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical improvement of photoaged skin with 50% glycolic acid. A double-blind vehicle-controlled study. Dermatol Surg. 1996;22:455-60.
- [CrossRef] [PubMed] [Google Scholar]
- Laser treatment of pigmented lesions. Dermatol Clin. 1997;15:397-407.
- [CrossRef] [PubMed] [Google Scholar]
- Laser therapy of freckles and lentigines with quasi-continuous, frequency-doubled, Nd:YAG (532 nm) laser in Fitzpatrick skin type IV: A 24-month follow-up. J Cosmet Laser Ther. 2002;4:81-5.
- [CrossRef] [PubMed] [Google Scholar]
- The use of Q-switched Nd:YAG laser in the treatment of superficial pigmented lesions in Koreans. J Dermatolog Treat. 2001;12:91-6.
- [CrossRef] [PubMed] [Google Scholar]
- Use of the Q-switched Nd:YAG laser for the treatment of pigmentary disorders in Egyptians. J Cosmet Laser Ther. 2010;12:92-100.
- [CrossRef] [PubMed] [Google Scholar]






