Translate this page into:
Comparison of efficacy and safety of low-fluence neodymium-doped yttrium aluminium garnet laser versus glycolic acid peeling in patients of melasma: A split-face study
*Corresponding author: Sharang Gupta, Department of Dermatology, Government Medical College, Patiala, Punjab, India. drsharanggupta97@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Arora R, Malhan S, Kaur R, Chopra D, Kaur M, Gupta S. Comparison of efficacy and safety of low-fluence neodymium-doped yttrium aluminium garnet laser versus glycolic acid peeling in patients of melasma: A split-face study. J Cutan Aesthet Surg. doi: 10.25259/jcas_43_24
Abstract
Objectives
To compare the efficacy and safety of low-fluence neodymium-doped yttrium aluminium (Nd:YAG) laser and glycolic acid peeling in Melasma
Material and Methods
80 patients of clinically diagnosed melasma were treated with 3 sessions of low-fluence Nd: YAG laser on the right side of the face. For the left side, initial 2 sessions of GA 35% and later 3 sessions of GA 70% were done. Outcome was measured as percentage reduction in melasma area and severity index (MASI) score.
Results
Statistically significant reduction in mean MASI score was recorded with both the modalities, though the total reduction with Nd: YAG laser was found to be significantly more compared to the reduction with GA peeling (P = 0.003). Erythema was the most common side effect observed with both treatments. Delayed side effects were not seen with GA peeling but one patient developed hyperpigmentation after Nd: YAG laser treatment.
Conclusion
Laser sessions have the added advantage over GA peeling requiring comparatively fewer sessions while being equally or more efficacious. Immediate side effects are more common with GA peeling, while delayed side effects are more common with laser therapy.
Keywords
Glycolic acid
Melasma
Q-switched Nd: YAG laser
INTRODUCTION
Melasma is an acquired hyperpigmentary disorder characterized by light to dark brown poorly circumscribed symmetrically distributed macules predominantly on sun-exposed parts of the face.1 Factors such as sun exposure, pregnancy, hormonal imbalance, genetic susceptibility, thyroid disorders, stress, and certain drugs could act as a triggering factor for this disease.2,3 The treatment of melasma is challenging due to its multifactorial pathogenesis leading to chronic and relapsing lesions and thus a multimodal approach is required for effective management.4 Conventionally, hydroquinone and non-hydroquinone-based depigmenting agents such as arbutin and tretinoin have been used for medical management, though now with increased awareness and affordability chemical peeling and lasers are increasingly becoming popular.5,6 Chemical peeling acts by accelerating the turnover of epidermal keratinocytes and thus helps in the removal of melanin. Peels can be broadly classified as superficial, medium, and deep according to the depth of action.7
The risk of complications from chemical peels increases proportionately with the concentration of peeling agent used.5
Lasers are sources of high-intensity monochromatic coherent light.8 The low-fluence Q-switched neodymium-doped yttrium aluminium garnet (Nd: YAG) laser is commonly used to treat cutaneous pigmentary lesions. A wavelength of 1064 nm is used for dermal lesions and a shorter wavelength of 532 nm for epidermal melanin.8,9
MATERIAL AND METHODS
This hospital-based, non-randomized split-face interventional study was undertaken on 80 clinically diagnosed patients of facial melasma presenting to the outpatient department of dermatology of a tertiary care center in north India from January 2021 to June 2022.
Inclusion criteria
Patients aged more than 18 years
Patients who gave written informed consent to participate in the study.
Exclusion criteria
History of pre-existing photodermatosis or patients on photosensitizing drugs
History of contact dermatitis to glycolic acid (GA) products
History of keloid formation
Pregnant and lactating patients
Patients on isotretinoin and/or tranexamic acid therapy in the past 3 months.
Patients using topical depigmenting agents in the past 3 months.
Complete history including age, sex, possible risk factors, and clinical examination for the type of melasma was documented and the melasma area and severity index (MASI) were calculated. Wood’s lamp examination was performed in every case to know the depth of pigment deposition.
Procedure
The face was primed with GA 6% cream for minimum of 2 weeks.
Left side of face
After cleansing the face was degreased with spirit followed by normal saline gauze. Postauricular sensitivity test was performed in every case before the peeling session. GA 35% (BRM chemicals) was applied for 2 and 3 min for the first and second sessions, respectively, which were spaced 2 weeks apart. The subsequent three sessions were spaced 4 weeks apart and the concentration was increased to 70% GA for 2, 3, and 3 min, respectively. Peel was neutralized with sodium bicarbonate solution in water after the desired contact time or till erythema appeared, whichever was earlier. Thus, a total of 5 sessions were performed.
Right side of face
After degreasing the face with spirit followed by normal saline gauze, topical anesthesia with a eutectic mixture of lignocaine and prilocaine was applied under occlusion for 1 h. Low-fluence Q-switched Nd: YAG laser (Derma India, Chennai) 1064 nm, 4 mm spot size, fluence of 0.3 J/cm2 was used. A total of three sessions were performed spaced 4 weeks apart and fluence was increased by 0.2 J/cm2 in every subsequent session. The last three glycolic acid (GA) peel sessions on the left side of the face were performed with concomitant laser sessions on the right side of the face.
Post-procedure care
An ice pack was applied for 1 min immediately after the procedure. This was followed by emollient which was topped by a broad-spectrum sunscreen (sun protection factor [SPF] > 30).
MASI score and any adverse event, whether immediate (occurring on the same day of therapy) or delayed (occurring after 24 h of procedure) following treatment, were separately noted for each side of the face in every session. Patients were followed up for a minimum of 1 month after completion of the whole therapy. Clinical improvement was assessed as a percentage reduction in MASI score. Statistical analysis was performed using the Statistical Package for the Social Sciences V22.0. The chi-square test was used to compare categorical variables and t-test was used to compare quantitative variables. P < 0.05 was considered statistically significant.
RESULTS
A total of 80 patients (71 females and 9 males) were enrolled in the study but three patients lost to follow-up. The mean age of presentation was 35.37 ± 8.66 years with the mean duration of disease being 5.09 ± 5.2 years. The majority of the patients had a centrofacial pattern, i.e., 48 cases (60%), followed by 29 cases (36.3%) of malar melasma and 3 cases (3.8%) of mandibular melasma. Wood’s lamp examination revealed the mixed type of melasma as most prevalent in 45 patients (56.3%) [Table 1]. The baseline mean MASI score on either side of patient’s face was 6.66 ± 2.42. It reduced to 3.87 ± 2.07 (P = 0.002) after three sessions of Nd: YAG laser therapy [Figure 1]. The change in mean MASI score between successive sessions was insignificant, but when compared with baseline, the reduction in MASI score was statistically significant after every session (P <0.05) [Table 2].
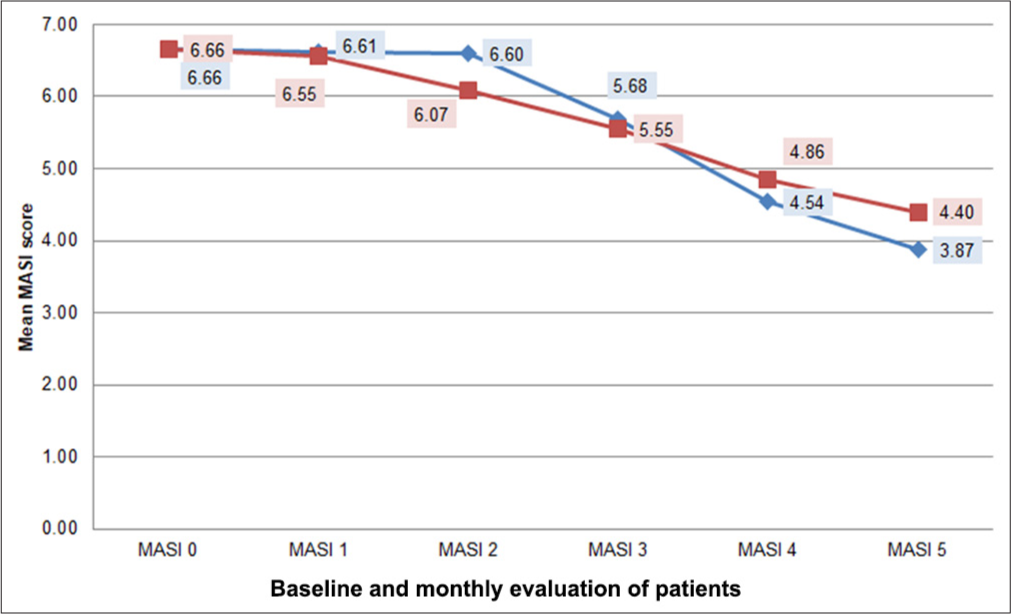
- Line diagram depicting percentage decrease in melasma area and severity index with Nd:YAG laser versus glycolic acid (GA) peel. Red line: MASI reduction with glycolic acid peeling, Blue line: MASI reduction with low-fluence ND;YAG laser, MASI: Melasma area and severity index, Nd:YAG: neodymium-doped yttrium aluminium garnet.
| Mean age of presentation | 35.37±8.66 years |
| Mean duration of melasma | 5.09±5.2 years |
| Pattern of melasma | n (%) |
| Centro facial | 48 (60) |
| Malar | 29 (36.3) |
| Mandibular | 3 (3.8) |
| Type of melasma | |
| Epidermal | 28 (35) |
| Dermal | 7 (8.8) |
| Mixed | 45 (56.3) |
| n | Mean MASI±SD | On successive session | Comparison with baseline | ||||
|---|---|---|---|---|---|---|---|
| Decrease (%) | P-value | Decrease (%) | P-value | ||||
| MASI 0 | 80 | 6.66±2.42 | _ | _ | _ | _ | |
| MASI 1 | 77 | 5.68±2.17 | 13.9 | 0.313 | 14.76 | 0.061 | |
| MASI 2 | 77 | 4.54±1.90 | 20 | 0.049 | 31.87 | 0.001 | |
| MASI 3 | 77 | 3.87±2.07 | 14.7 | 0.7 | 41.93 | <0.001 | |
MASI: Melasma area and severity index, SD: Standard deviation, Nd:YAG: neodymium-doped yttrium aluminium garnet.
On the left side of the face, the mean MASI score reduced from 6.66 ± 2.42 on the baseline to 4.40 ± 2.21 (P = 0.003) after the fifth session of GA peeling [Figure 1]. As seen with Nd: YAG laser, the change in MASI score between two sessions of GA peeling was not statistically significant (P > 0.05), but the reduction became significant when compared to baseline after the second session of GA peel (P < 0.05) [Table 3].
| n | Mean MASI±SD | On successive session | Comparison with baseline | |||
|---|---|---|---|---|---|---|
| Decrease (%) | P-value | Decrease (%) | P-value | |||
| MASI 0 | 80 | 6.66±2.42 | _ | _ | _ | _ |
| MASI 1 | 77 | 6.55±2.39 | 1.6 | 1.00 | 1.63 | 1.00 |
| MASI 2 | 77 | 6.07±2.32 | 7.3 | 0.7 | 8.78 | 0.8 |
| MASI 3 | 77 | 5.55±2.09 | 8.5 | 1.00 | 16.61 | 0.032 |
| MASI 4 | 77 | 4.86±2.00 | 12.4 | 0.820 | 37.15 | 0.001 |
| MASI 5 | 77 | 4.40±2.21 | 9.4 | 0.79 | 33.97 | 0.001 |
MASI: Melasma area and severity index, SD: Standard deviation
On comparing the two sides of face, the total reduction in mean MASI score with Nd: YAG laser was found to be significantly more compared to the reduction with GA peeling (P = 0.003) [Table 4 and Figure 2].
| Side of face | Pre-treatment MASI | Post-treatment MASI | Percentage of improvement | P-value | P-value |
|---|---|---|---|---|---|
| Right half (Nd:YAG laser) | 6.66±2.42 | 3.87±2.07 | 41.93 | 0.002 | 0.003 |
| Left half (GA peel) | 6.66±2.42 | 4.40±2.21 | 33.97 | 0.003 |
MASI: Melasma area and severity index, GA: Glycolic acid, Nd:YAG: neodymium-doped yttrium aluminium garnet.
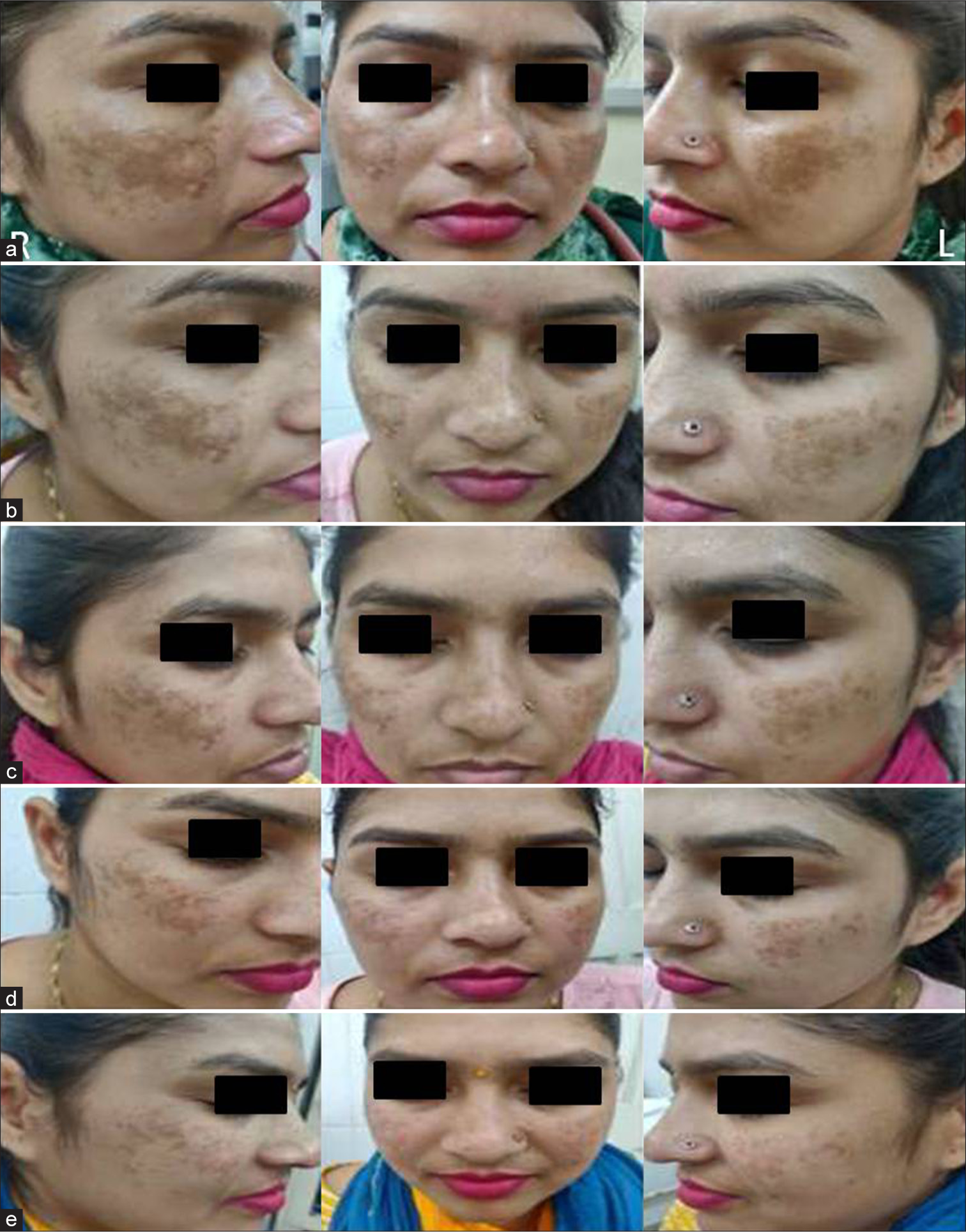
- (a) Pre-procedure image. (b–e) Results after glycolic acid (GA) peeling on the left side and low-fluence Nd:YAG laser on the right side. Nd:YAG: neodymium-doped yttrium aluminium garnet
Both treatment modalities showed better results in patients of epidermal melasma compared to mixed and dermal melasma. The mean MASI score in epidermal melasma reduced from 5.97 to 3.07 (P = 0.001) with laser and to 3.67 (P = 0.001) with GA peel. Mixed melasma improved from MASI 6.78 to 4.14 (P = 0.003) with laser and to 4.56 (P = 0.004) with GA peel. For dermal melasma, MASI score reduced from 8.22 to 5.48 (P = 0.011) with laser and to 6.43 (P = 0.013) with GA peel [Tables 5 and 6].
| n | MASI 0 | MASI 5 | Decrease (%) | P-value | |
|---|---|---|---|---|---|
| Epidermal | 27.00 | 5.97 | 3.07 | 48.57 | 0.001 |
| Dermal | 6.00 | 8.22 | 5.48 | 33.33 | 0.011 |
| Mixed | 44.00 | 6.78 | 4.14 | 38.93 | 0.003 |
MASI: Melasma area and severity index, GA: Glycolic acid, Nd:YAG: neodymium-doped yttrium aluminium garnet.
| n | MASI 0 | MASI 5 | Decrease (%) | P-value | |
|---|---|---|---|---|---|
| Epidermal | 27.00 | 5.97 | 3.67 | 38.48 | 0.001 |
| Dermal | 6.00 | 8.22 | 6.43 | 21.73 | 0.013 |
| Mixed | 44.00 | 6.78 | 4.56 | 32.67 | 0.004 |
MASI: Melasma area and severity index
Immediate side effects (seen within 24 h of the procedure) were seen in 11.2% of patients on the side treated with Nd: YAG laser and 21.25% of patients on the side treated with GA peel [Table 7]. The most common side effect observed with both treatments was erythema in 7 patients (8.7%) with laser and 8 patients (10%) with GA peeling [Figure 3]. This was followed by stinging sensation in 2 patients (2.5%) with laser and 6 patients (7.5%) with GA peeling. In patients treated with GA peel, one patient developed localized swelling on the face, while two patients developed post-inflammatory hyperpigmentation [Figure 4]. Delayed side effects were not seen with GA peeling therapy, but one patient developed hyperpigmentation after 1 month of 2nd session of laser treatment.

- (a) Erythema after Nd:YAG laser therapy. (b) Erythema after glycolic acid (GA) peeling. Nd:YAG: neodymium-doped yttrium aluminium garnet.

- (a) Before and (b) after images of hyperpigmentation after glycolic acid (GA) peeling.
| With laser | With chemical peel | |||
|---|---|---|---|---|
| Number of patients | Percentage | Number of patients | Percentage | |
| None | 71 | 88.7 | 63 | 78.7 |
| Erythema | 7 | 8.7 | 8 | 10 |
| Stinging sensation | 2 | 2.5 | 6 | 7.5 |
| Swelling | 0 | 0 | 1 | 1.25 |
| Hyperpigmentation | 0 | 0 | 2 | 2.5 |
DISCUSSION
GA is a hydrophilic agent that belongs to the group of α-hydroxy acids.10 By its metabolic action, it decreases keratinocyte cohesion at low concentrations whereas at higher concentrations, it stimulates epidermolysis, followed by desquamation and the dispersion of epidermal melanin.11 Nd: YAG lasers on the other hand, function on the principle of selective photothermolysis. This states that when a specific wavelength of energy is delivered in a time period shorter than the thermal relaxation time of the target chromophore, the energy is confined to the target and thus causes minimal damage to the surrounding tissues.8,12 It has been seen that lasers target mature melanosomes and spare early-stage melanosomes.13,14 Thereby, both chemical peeling and laser provide targeted cutaneous pigment ablation for rapid and predictable results to a desired cutaneous depth.6
In our study, treatment with low-fluence Nd: YAG laser led to a 41.9% reduction in mean MASI score after 3 sessions (P = 0.002). Similar findings were observed by Kaur et al., who reported a 46.11% reduction after 4 sessions of lowfluence Nd: YAG laser.15 Another study by Kar et al. also used low-fluence Nd: YAG laser, but they used a more frequent and greater number of sessions (12 sessions, once/week) and reported a comparable reduction of 47.9% in MASI score.16 Thus, we can say that it is better to space subsequent sessions wide apart as they can achieve similar results while requiring fewer sessions along with the added benefit of being economically beneficial to the patient, minimizing the hospital visits, and having fewer side effects.
On the side treated with GA peel, MASI score was significantly reduced by 33.3% (P = 0.003). Improvements ranging from 20% to 80% have been reported with varying concentrations of GA peel.16-19 This wide variation could be because several factors influence the outcome of chemical peeling, such as composition, concentration, or formulation of peeling agent (gel or aqueous-based) and frequency of treatment sessions.20
Studies are still not conclusive about the superiority or efficacy of chemical peel and laser over one another. Similar to our study, Kar et al. observed a clinically more significant reduction in MASI score with Nd: YAG laser compared to that with GA peeling, whereas Divya and Kaur and Kar reported comparable MASI scores with low-fluence Nd: YAG laser and GA peeling.15,16,21 Lack of standardized parameters for laser pigment ablation, variability in skin tones in the Indian population, and differing composition of chemical peeling agents are some of the factors that hinder a comparison between the two modalities. A split-face study aims to minimize patient-related confounding factors.
The study highlights an important but often missed advantage that is of serial photography of the patient. As observed, the mean MASI score reduction between successive sessions of either of the modalities was insignificant but the reduction was significant when compared to the baseline MASI score. Thus, while the patient may not notice the gradual improvement in pigmentation that occurs after each session, a baseline photographic documentation can help make this more evident and thus help in improving patient compliance and satisfaction.
In our study, immediate side effects observed on the same day of the procedure were seen more commonly with GA peel compared to low-fluence Nd: YAG laser. The most common side effect observed with both treatments was self-resolving erythema followed by a stinging sensation. We noticed a proportional increase in side effects with increasing concentration of peeling agent.5 One of the patients had post-inflammatory hyperpigmentation or burns with 70% GA peel. Thus, concentrations of GA reaching deeper dermis should therefore be used with caution in Fitzpatrick skin type IV and V. Priming the skin before the procedure and applying ice packs after the procedure to reduce inflammation may help to reduce the irritating side effects of both chemical peeling and laser.
In our study, delayed side effects during follow-up were not seen with GA peeling, but one patient developed hyperpigmentation after Nd: YAG laser treatment. None of the participants developed delayed mottled hypopigmentation. Fewer patients experienced side effects compared to other studies, probably due to a lesser number of sessions and a wider gap between subsequent sessions.
Limitation
Certain delayed side effects could have been missed due to the shorter duration of follow-up.
CONCLUSION
Both chemical peeling and low-fluence Q-switched Nd: YAG laser provides significant improvement in melasma. However, laser treatment has the added advantage of requiring a comparatively lesser number of sessions compared to GA peeling while being equally or more efficacious. Lasers selectively target melanin in the skin, so a sufficient period to remove this pigment by melanophages may improve the efficacy of therapy, be economically beneficial, and improve patient compliance. Furthermore, serial photography of patients plays a crucial role since the significant reduction in MASI score is seen when compared to baseline and not when compared to previous sessions. The irritating effects of both therapies, though seen in a few patients, could be minimized by following proper pre and post-procedure care while minimizing delayed complications and requiring targeting the basic pathology of the disease while concurrently using maintenance treatment and photoprotection. Lasers, while promising effective results, come with a warning of causing delayed post-inflammatory hyperpigmentation.
Authors’ contributions
Raina Arora: Principal investigator, literature search and review, data analysis, writing the manuscript, critical revision, approval of final version. Shreya Malhan: Designing the study, literature search and review, writing the manuscript, approval of the final version. Ravneet Kaur: Principal investigator, literature search and review, data analysis, writing the manuscript, critical revision, approval of final version. Dimple Chopra- Designing the study, literature search and review, data collection, critical revision, approval of the final version. Maninder Kaur: Literature search and review, data analysis, writing the manuscript, critical revision, approval of final version. Sharang Gupta: Designing the study, data collection and analysis, literature search and review, writing the manuscript, critical revision, approval of the final version.
Ethical approval
The research/study was approved by the Institutional Review Board at Baba Farid University of Health Sciences, Faridkot, number BFUHS/2K21p-TH/14771, dated 15th December, 2021.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Evaluation of vitamin D in melasma patients. Rev Rom Med Lab. 2019;27:219-22.
- [CrossRef] [Google Scholar]
- Melasma and thyroid disorders: A systematic review and metaanalysis. Int J Dermatol. 2019;58:1231-8.
- [CrossRef] [PubMed] [Google Scholar]
- Melasma: A clinical and epidemiological review. An Bras Dermatol. 2014;89:771-82.
- [CrossRef] [PubMed] [Google Scholar]
- Melasma: Clinical diagnosis and management options. Australas J Dermatol. 2015;56:151-63.
- [CrossRef] [PubMed] [Google Scholar]
- The treatment of melasma: A review of clinical trials. J Am Acad Dermatol. 2006;55:1048-65.
- [CrossRef] [PubMed] [Google Scholar]
- A practical approach to chemical peels: A review of fundamentals and step-by-step algorithmic protocol for treatment. J Clin Aesthet Dermatol. 2018;11:21.
- [Google Scholar]
- Update on melasma-part II: Treatment. Dermatol Ther (Heidelb). 2022;12:1989-2012.
- [CrossRef] [PubMed] [Google Scholar]
- Lasers for treatment of melasma and post-inflammatory hyperpigmentation. J Cutan Aesthet Surg. 2012;5:93.
- [CrossRef] [PubMed] [Google Scholar]
- Optimizing Q-switched lasers for melasma and acquired dermal melanoses. Indian J Dermatol Venereol Leprol. 2019;85:10-7.
- [CrossRef] [PubMed] [Google Scholar]
- Chemical peeling in ethnic skin: An update. Br J Dermatol. 2013;169:82-90.
- [CrossRef] [PubMed] [Google Scholar]
- Glycolic acid peels in the treatment of melasma among Asian women. Dermatol Surg. 1997;23:177-9.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of lowfluence 1064-nm Q-switched Nd: YAG laser with topical 20% azelaic acid cream and their combination in melasma in Indian Patients. J Cutan Aesthet Surg. 2012;5:266-72.
- [CrossRef] [PubMed] [Google Scholar]
- Heterogeneous pathology of melasma and its clinical implications. Int J Mol Sci. 2016;17:824.
- [CrossRef] [PubMed] [Google Scholar]
- Lasers in melasma: A review with consensus recommendations by Indian pigmentary expert group. Indian J Dermatol. 2017;62:585-90.
- [CrossRef] [Google Scholar]
- A prospective, randomised, split-face comparative study of 50% glycolic acid peel versus laser toning in the treatment of melasma in Asian skin. Int J Res. 2020;6:371.
- [CrossRef] [Google Scholar]
- A comparative study on efficacy of high and low fluence Q-switched Nd: YAG laser and glycolic acid peel in melasma. Indian J Dermatol Venereol Leprol. 2012;78:165-71.
- [CrossRef] [PubMed] [Google Scholar]
- Safety and efficacy of glycolic acid facial peel in Indian women with melasma. Int J Dermatol. 2001;40:354-7.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative study of trichloroacetic acid versus glycolic acid chemical peels in the treatment of melasma. Indian J Dermatol Venereol Leprol. 2010;76:447.
- [CrossRef] [PubMed] [Google Scholar]
- A study on fractional erbium glass laser therapy versus chemical peeling for the treatment of melasma in female patients. J Cutan Aesthet Surg. 2013;6:148-51.
- [CrossRef] [PubMed] [Google Scholar]
- Chemical peels in melasma: A review with consensus recommendations by Indian pigmentary expert group. Indian J Dermatol. 2017;62:578-84.
- [CrossRef] [Google Scholar]
- Efficacy and safety of 70% glycolic acid versus Q Switched Nd: YAG laser in the treatment of melasma: A comparative study. Int J Res. 2017;3:1.
- [CrossRef] [Google Scholar]







