Translate this page into:
A 7-year Experience with Keloid Fillet Flap and Adjuvant Intralesional Corticosteroids
Address for correspondence: Dr. Diogo Cerejeira, Rua Marta Mesquita da Câmara, nº110, A3 4ºDto-4150-485 Porto, Portugal. E-mail: Diogo_cerejeira@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Context:
Keloids are fibroproliferative scars characterized by excessive collagen deposition beyond the margins of the original wound. Although many treatment modalities were described in the literature, no single first-line therapy is recommended, and its recurrence rate remains high.
Aims:
The aim of this study was to investigate the efficacy rate in treating auricle keloids after fillet flap excision combined with adjuvant intralesional steroid injections.
Settings and Design:
This was a retrospective study.
Materials and Methods:
Between 2012 and 2019, a total of 16 auricle keloids were treated at our center with fillet flap excision and adjuvant steroid injections. Intralesional steroid injections were given at the end of the first week and then administered at 4-week intervals until the lesions were soft and flat. Postoperative efficacy, complications, recurrence, and patient satisfaction were analyzed.
Results:
A high improvement of the keloid was observed in 13 (81.2%) lesions. No major complications and no recurrence of the keloid were detected during the follow-up period (mean, 35 months). Regarding patient satisfaction, nine (81.8%) considered their result as excellent.
Conclusion:
This study showed that this approach is effective regardless of the keloid location at the auricle.
Keywords
Auricle keloid
keloid core excision
keloid fillet flap
This study shows that keloid fillet flap with adjuvant intralesional corticosteroids leads to a high improvement of the keloid regardless its location
This procedure seems to be safe and seems to be very well tolerated by the patients

INTRODUCTION
Keloids are characterized by an excessive scar tissue growth that extends beyond the original margins of the lesion, and does not tend to regress.[1] It usually develops months or years after the primary inciting factor, and shows a preference for some anatomical locations such as the chest, shoulders, head and neck (especially auricle), and upper back.[2] Causes of keloids include surgeries, burns, abrasions, piercings, tattoos, immunization, insect bites, and inflammatory cutaneous processes, in particular acne and chicken pox.[1]
Keloid formation is commonly observed between the ages of 10 and 30[3] and its growth increases with pregnancy and puberty.[45] Both genders are equally affected, whereby the higher incidence reported in women is probably related to greater cosmetic concern and frequent ear piercing.[2] The development of keloids is correlated with skin pigmentation[4] (the incidence of keloids in dark skin is estimated to be 15 times as high as in light-skinned individuals)[16] and tends to run in families. The incidence of ear lobe keloid after piercing is estimated to be 2.5% and the condition is more likely to form after the age of 11 years.[78] Keloid scars only occur in humans; therefore, no animal model exists.[9]
Even though most of the patients are asymptomatic, keloids may cause pain, pruritus, burning, and disfigurement, which may lead to psychological stress, depression, and reduced quality of life.[9] Numerous therapy approaches have been carried out in an attempt to treat this condition. However, the plurality of established therapies only reflects its high recurrence rate and resistance to treatment, making keloids a particularly challenging entity. According to a literature review, surgical excision alone leads to success rates between 20% and 25% and recurrence rates ranging from 45% to 100%.[110] Hence, a combination of therapies is recommended to reduce the risk of relapse in predisposed individuals.[911] Some of the options available that may be combined with excision include steroid injection, button compression, interferon alfa-2b injection, radiation, laser, and imiquimod cream. The purpose of this retrospective study was to evaluate the efficacy of surgical excision with fillet flap in combination with adjuvant steroid injection. We also analyzed postoperative complications, recurrence rates, and patient satisfaction.
SUBJECT AND METHODS
Study population
Eleven patients with 16 auricle keloids underwent surgical excision with fillet flap and received adjuvant steroid injections at our center between 2012 and 2019. We excluded from the study patients with nonauricle keloids, surgical excision using nonfillet techniques, absence of adjuvant therapies with triamcinolone, and patients who were lost to follow-up. Keloids varied in size from 0.8 cm × 1 cm to 2.8 cm × 3.2 cm and all the patients had a history of ear piercing. None of the patients had keloids elsewhere in the body.
The patient group consisted of nine women (81.8%) and two (18.2%) men, age ranging from 16 to 34 years (mean age 22.9 years). Six (54.5%) of the patients had a Fitzpatrick skin type I–III and five (45.5%) individuals had a Fitzpatrick skin type IV–VI. Regarding location and distribution, nine (81.8%) had unilateral keloids and two (18.2%) had bilateral auricle keloids. The lobules (62.5%) were affected more than the auricle (37.5%) and the retro auricular side (87.5%) was affected more than the anterior side (12.5%). Two patients (18.2%) had preoperative therapy (one intralesional steroid injections and one wedge excision).
Postoperative surgical efficacy was rated as mild, moderate, or high, considering four parameters: softness, flattening, absence of pigmentation, and no recurrence (defined by the absence of relapse within a period of 6 months). A high improvement was registered when the four parameters were achieved (100%), moderate when three were achieved (75%), and mild when one or two parameters were achieved (25%–50%). Patient satisfaction was assessed by a subjective evaluation survey (poor, average, good, or excellent) [Table 1], conducted by telephone call in April 2019.
| Patient | Sex | Age, yr | Keloid | Location | Injections, n | Follow up, Monhs | Clinical Efficacy, % | Patient Perception |
|---|---|---|---|---|---|---|---|---|
| 1 | F | 34 | 1 | Rt. earlobe | 2 | 88 | 100 | Excellent |
| 2 | F | 16 | 2 | Rt. earlobe | 2 | 82 | 75 | Good |
| 3 | Lt. earlobe | 2 | 78 | 100 | Excellent | |||
| 3 | F | 18 | 4 | Rt. Helix | 2 | 62 | 100 | Excellent |
| 4 | F | 26 | 5 | Rt. Helix | 2 | 55 | 100 | Excellent |
| 5 | F | 27 | 6 | Rt. Helix | 2 | 44 | 75 | Excellent |
| 6 | F | 23 | 7 | Lt. earlobe | 2 | 24 | 100 | Excellent |
| 7 | F | 22 | 8 | Rt. earlobe | 2 | 20 | 100 | Excellent |
| 9 | Rt. earlobe | 2 | 20 | 100 | Excellent | |||
| 10 | Lt. earlobe | 2 | 18 | 100 | Excellent | |||
| 8 | F | 20 | 11 | Lt. Helix | 2 | 18 | 100 | Excellent |
| 12 | Lt. Helix | 2 | 16 | 100 | Excellent | |||
| 9 | F | 18 | 13 | Lt. scapha | 2 | 12 | 50 | Good |
| 10 | M | 30 | 14 | Rt. earlobe | 3 | 8 | 100 | Excellent |
| 15 | Rt. earlobe | 3 | 8 | 100 | Excellent | |||
| 11 | M | 23 | 16 | Lt. earlobe | 3 | 6 | 100 | Excellent |
Surgical protocol
The flap was marked so that the pedicle was in a hidden position [Figure 1]. Following the infiltration of local anesthesia around the keloid (2% lidocaine with epinephrine 1:100,000), a superficial incision was made in the keloid, 2 mm away from its margin, until approximately halfway [Figure 2]. The keloid flap, which consists of epidermis and a thin layer of dermis preserving the vascular plexus, was raised from the fibrous keloid core [Figure 3]. This flap is not easily separated from the keloid core with the scalpel, due to the presence of fibrous tissue, posing a risk of a transfixive lesion. Therefore, it is preferable to make a thicker flap in the first instance and curettage the excessive tissue afterward. After raising the flap completely, the fibrous keloid core was removed and the bleeding was meticulously controlled [Figures 4 and 5]. The redundant flap was trimmed and the wound was closed using 6-0 nylon interrupted suture [Figure 6]. Pressure dressing was applied with tugging stitches. No preventive procedures, intra or perioperatively, were applied. All specimens were sent for pathologic evaluation and were diagnosed as keloids.

- A large 2.5 cm × 1.4 cm × 1.2 cm earlobe keloid

- Skin dissection from the overlying fibrous keloid core

- Fibrous keloid core after scalpel dissection

- Removal of the keloid mass

- Curettage of the remaining fibrous tissue

- Intraoperative result of the earlobe flap repair
Therapy regimen
Within the therapeutic regimen, surgical intervention was followed by an intralesional corticosteroid injection (1mL of 40mg/mL triamcinolone acetonide) at the end of the first week on the day of suture removal. The drug was injected intradermally, before the suture was removed, to prevent surgical wound dehiscence. Subsequent injections were administered at 4-week intervals until the lesions were soft and flat.
RESULTS
Follow-up ranged from 6 months to 7 years (mean follow-up, 35 months). In most cases, only two intralesional corticosteroid injections were needed (81.2%), whereas the remaining patients were administered three injections (18.8%). The scars were minimal [Figure 7] and were assessed according to the four established parameters: softness, flattening, pigmentation, and recurrence. Small nodules were apparent in two lesions (12.5%), whereas pigment dyschromia was also seen in two of them (12.5%). All lesions were soft and there was no evidence of recurrence neither in the first 6 months nor the overall follow-up period. A high improvement of the keloid was assessed in 81.2% of the lesions, 12.5% had moderate improvement, and 6.3% experienced mild improvement. No patients aggravated their clinical condition.
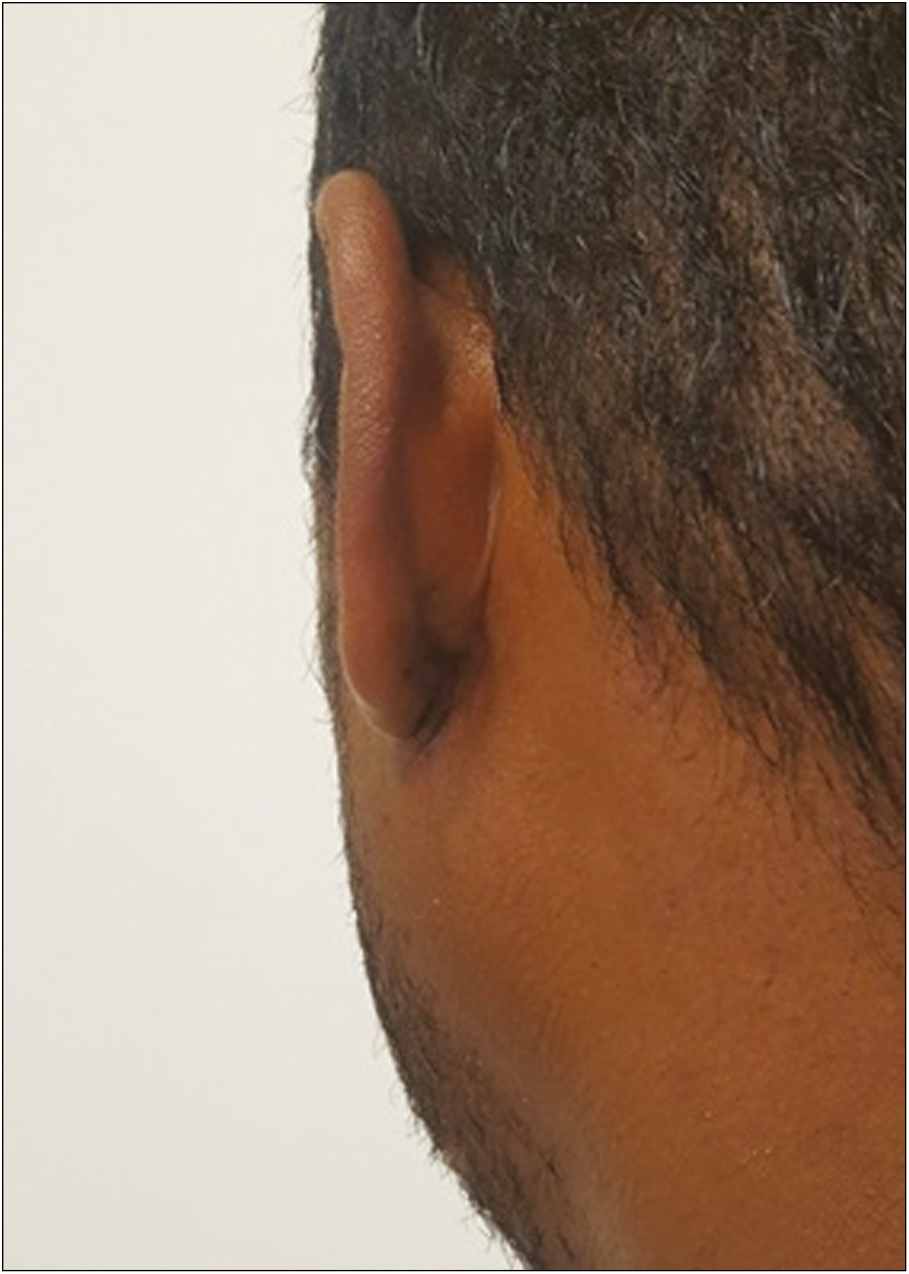
- Two-year postoperative follow-up
All flaps survived and no signs of necrosis were identified. There was also no dehiscence of the surgical wound, infection, or any other major complications. During the first month of follow-up, local edema, erythema, ecchymosis, and stinging sensations in variable percentages were observed, which reversed with time and/or the use of intralesional steroids.
Subjective analysis of the patients corroborated these numbers, as nine of them (81.8%) considered their result as excellent and two (18.2%) as good [Table 1].
DISCUSSION
Although both are characterized by excessive collagen deposition, keloids are different from hypertrophic scars. Hypertrophic scars (i) are generally confined to the limits of the original lesion, (ii) appear within 4 weeks after trauma, (iii) tend to respond to therapeutic procedures, and (iv) usually regress over time. In contrast, keloids (i) proliferate beyond initial margins of the wound, (ii) are usually developed months or years after the primary inciting factor, (iii) have a high recurrence rate, and (iv) do not tend to regress.[12] Thus far, no single first-line therapy is recommended concerning keloids.[1314] However, it is commonly accepted that most monotherapy options have high relapse rates associated.[9] Surgery followed by different adjuvant treatments is often considered the preferred multimodal treatment. Several adjuvant modalities have been described to prevent the recurrence after surgical excision, including intralesional steroids, pressure, imiquimod, interferon alfa-2b injection, laser, and radiotherapy. One of the most frequently used is the combination of surgical excision with intralesional steroid injections. This combination has been reported to yield a recurrence rate ranging from 3% to 25%,[15] which is in contrast to the 60% recurrence using standard excision alone.[1]
Although there are many surgical techniques described in the literature, keloid fillet flap is known to meet the “5 As and one B” (asepsis, atraumatic technique, absence of raw surface, avoidance of tension, accurate approximation of wound margin, and complete bleeding control) that might be important to reduce relapse rates. It also has fewer limitations to cover the defect compared to primary suture, secondary intention healing, skin grafts, and local flaps.[15]
In our protocol, we describe a slightly different technique for keloid fillet flap: the usage of a curette when raising the flap facilitates the separation of the fibrous keloid core, allows a better control of flap thickness, and reduces the risk of accidentally provoking a transfixive lesion with the scissor or blade, which could lead to the formation of a new keloid. Subcutaneous sutures were not used to reduce the possibility of foreign body reaction. No intralesional steroids were injected perioperatively to prevent flap congestion. Instead, intralesional steroids were injected 1 week after, just before suture removal, as associated increased pressure could possibly lead to wound dehiscence.
Most lesions (81.2%) had an objective high improvement and no complications were detected apart from minor and expected ones (swelling, erythema, ecchymosis, and stinging sensations), which resolved during the first month. Although all the scars had an acceptable cosmetic appearance, scar pigmentation was more noticeable in two low Fitzpatrick skin type patients compared to higher skin types. The same method was applied to different located auricle keloids, but results do not seem to vary. No patients aggravated their clinical condition and there was no evidence of recurrence during the follow-up period (mean, 35 months). Finally, all patients considered their result either as excellent (81.8%) or good (18.2%) despite a mild-to-moderate improvement in three (18.8%) of the lesions.
Auricle keloids continue to be a therapeutic challenge due to its intricate process and high recurrence rates. Although keloid fillet flap with adjuvant intralesional steroids was already described as a possible therapeutic modality, our protocol differs slightly in some aspects, including curettage of the fillet flap, and has shown excellent results in efficacy, recurrence, and patient satisfaction.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Earlobe keloids: A pilot study of the efficacy of keloidectomy with core fillet flap and adjuvant intralesional corticosteroids. Dermatol Surg. 2013;39:1514-9.
- [Google Scholar]
- A new surgical treatment of keloid: keloid core excision. Ann Plast Surg. 2001;46:135-40.
- [Google Scholar]
- The aetiology of keloids: A review of the literature and a new hypothesis. S Afr Med J. 1964;38:913-6.
- [Google Scholar]
- Treatment of earlobe keloids by extralesional excision combined with preoperative and postoperative “sandwich” radiotherapy. Plast Reconstr Surg. 2010;125:135-41.
- [Google Scholar]
- Earlobe keloids: A novel and elegant surgical approach. Dermatol Surg. 2010;36:395-400.
- [Google Scholar]
- Clinical outcome and quality of life after a multimodal therapy approach to ear keloids. JAMA Facial Plast Surg. 2015;17:333-9.
- [Google Scholar]
- In search of the optimal treatment of keloids: Report of a series and a review of the literature. Ann Plast Surg. 1991;27:164-78.
- [Google Scholar]
- The impact of adenotonsillectomy on children’s quality of life. Clin Otolaryngol. 2008;33:56-9.
- [Google Scholar]
- On the nature of hypertrophic scars and keloids: A review. Plast Reconstr Surg. 1999;104:1435-58.
- [Google Scholar]
- German S2K guidelines for the therapy of pathological scars (hypertrophic scars and keloids) J Dtsch Dermatol Ges. 2012;10:747-62.
- [Google Scholar]
- International clinical recommendations on scar management. Plast Reconstr Surg. 2002;110:560-71.
- [Google Scholar]
- A surgical approach for earlobe keloid: Keloid fillet flap. Plast Reconstr Surg. 2004;113:1668-74.
- [Google Scholar]





